![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
73 Cards in this Set
- Front
- Back
|
|
|
|
|
|
|
|
|
|

|
|

|

|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|
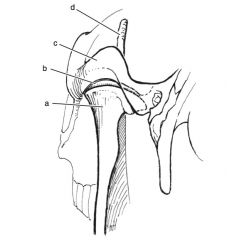
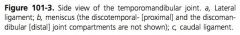
Shape of TM joint:
|
incongruous formed ventrally by mandibular condly and dorsally by zygomatic process of temporal bone with meniscus separating joint into dorsal and larger ventral compartments
|
|
|
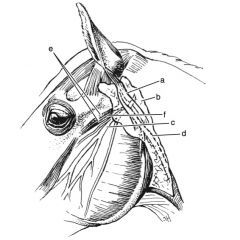
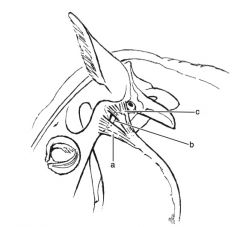
What structures are associated with the TM joint?
|
Parotid, transverse facial artery and vein ventrally, transverse facial branch of auricular-temporal nerve
|
|
|
Indications for TM arthroscopy:
|
debridement of meniscal tears, removal of osseous fragments
|
|
|
Indications for condylectomy of the mandible:
|
chronic septic OA of TM joint, fractures of TM joint, TM luxation, severe chronic OA of TM joint as a savage procedure
|
|
|
Complication of condylectomy of the mandible:
|
development of pseudocondyles, masseter atrophy, malocclusion, difficulty in prehension or mastication
|
|
|
What mand/max fractures can be managed conservatively?
|
Unilateral fractures of the mandible, maxilla, premaxilla, or incisive bone that are minimally displaced
|
|
|
Indications for mand/max fracture repair:
|
fractures that are unstable, cause malocclusion of teeth, bilateral, reluctance to eat or drink because of pain
|
|
|
Benefits of mand/max fracture repair vs conservative management:
|
improved cosmetic outcome, more rapid healing
|
|
|
What is the tension side of the jaw?
|
Oral surface of mandibular and maxilla
|
|
|
Why is intra-oral wiring not indicated with comminuted fractures?
|
Fragment collapse when wires tightened resulting in malocclusion
|
|
|
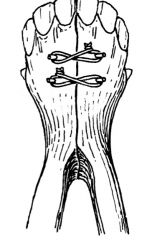
How is collapse prevented in comminuted mand/max fractures repaired with intra-oral wire?
|
Buttress with intra-oral splint, external fixator, plates
|
|
|
Why are loose teeth not removed with fracture repair?
|
Viability is difficult to determine at surgery, provide anchor sites and support neighboring teeth during intra-oral wiring
|
|
|
Benefit of intra-oral wiring + external fixation vs internal fixation in mand/max fractures:
|
inexpensive, fixation can be varied to accommodate fracture configuration, screws are easily stripped, screw placement to avoid teeth is difficult, implants become infected and have to be removed, difficult to place plate on tension surface
|
|
|
Where are plates placed for internal fixation of mand/max fracture?
|
Lateral or ventrolateral surface of mandible and lateral to dorsolateral for maxilla
|
|
|
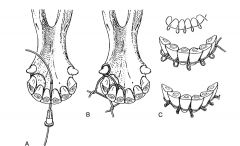
Indications for intra-oral wiring:
|
fracture of incisors, incisive bone, mandibular symphysis, premaxilla
|
|
|
What can provide caudal anchoring with intra-oral wiring?
|
Canine, 4.5 cortex screw in interdental space, 2.5 mm hole drilled across lateral edge of interdental space, 2nd premolar
|
|
|
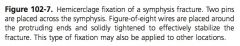
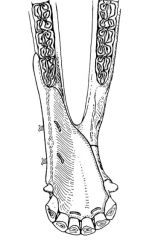
Indications for hemicerclage wire mand/max fixation:
|
fracture of mandibular symphysis in young foals
|
|
|
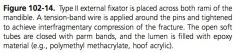
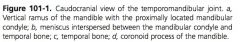
Indications for figure 8 wiring of the mandible:
|
fracture of interdental space in young foals
|
|
|
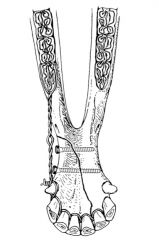
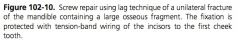
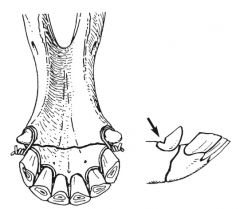
Indications for tension band wiring to cheek teeth:
|
fractures of the diastema of the mandible
|
|
|
What stabilizes tension band wiring to cheek teeth:
|
intact mandible with unilateral fracture, bilateral wiring, with premaxilla fractures the facial bones, nasal septum, and concha
|
|
|
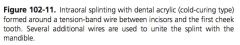
how is an intra-oral splint fitted?
|
Contoured to roof or floor of mouth to level of ’06, wired through splint and bone and secured with wire
|
|
|
disadvantages of U bar fixation:
|
time consuming to apply
|
|
|
Advantage of U bar fixation:
|
very stable
|
|
|
Indication for mand/max fracture screw repair:
|
fracture of the mandibular symphysis or diastema
|
|
|
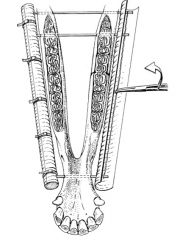
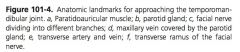
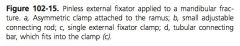
Indications for mand/max external fixator:
|
fractures of the ramus or body of mandible, premaxilla, maxilla
|
|
|
Advantage of mand/ max external fixator:
|
closed repair, reduced risk of infection, easy to remove, good stability
|
|
|
Disadvantage of mand/ max external fixator:
|
technical expertise to apply, expense of equipment, trauma to roots, infection of pin resulting in loosening
|
|
|
Indications for type 1 external fixator in mand/max fracture:
|
unilateral fracture of horizontal ramus of mandible
|
|
|
Indications for type 2 external fixator in mand/max fracture:
|
bilateral fractures of mandible, premaxilla, unstable unilateral fracture
|
|
|
Pin size and type for mand/max external fixator:
|
4 mm end threaded for type 1, centrally threaded for type 2
|
|
|
Connecting bar options for mand/max external fixator:
|
6mm Steinman pin, acrylic side bar +/- wiring around pins prior to filling with PMMA
|
|
|
What type of fixator is the pinless external fixator?
|
1
|
|
|
Benefits of pinless EF:
|
lack of pin tract infection, doesn’t traumatize roots, flexibility in application points, adjust construct during healing, debridement of sequestrum at fracture without disturbing construct
|
|
|
Disadvantage of pinless EF:
|
cost
|
|
|
Indications for mand/ max plate fixation:
|
fracture of ramus and body of mandible
|
|
|
Where are plates placed for internal fixation of the mandible?
|
Ventral, ventrolateral, lateral
|
|
|
Disadvantage of ventral application of plate to the mandible?
|
Biomechanically inferior to placement on the ventrolateral aspect
|
|
|
Disadvantage of ventrolateral application of plate to mandible:
|
exposure difficult because of parotid duct and screw placement difficult because of roots
|
|
|
When are implants removed from mand/max fractures?
|
6-8 weeks
|
|
|
Treatment of skull fractures:
|
closed reduction, open reduction +/- wire suture or flapfix system, reconstruction plates in severely comminuted or unstable fractures
|
|
|
When should skull fractures be fixed?
|
Delayed until soft tissue swelling decreases but within 2-3 days
|
|
|
Complications of skull fracture:
|
poor cosmetic outcome, secondary sinusitis, sequestrum formation
|
|
|
Treatment of periorbital fractures:
|
reduction of fragments (open or closed) with or without a bone hook +/- suture wiring, reconstruction plates for severely comminuted fractures of the zygomatic arch
|
|
|
Indications for periorbital fracture repair:
|
fragment impingment on eye or ocular structures
|
|
|
Complications of periprobital fractures:
|
trauma to the eye( rupture, proptosis, corneal ulceration or laceration, chemosis, injury to nasolacrimal duct), emphyema of sinuses
|
|
|
Why does suturing skin over a sinus fistula result in necrosis of the skin flap?
|
Air is in the sinus under the flap, which dehydrates the skin causing necrosis
|
|
|
Treatment for sinus fistula:
|
periosteal + cancellous bone graft or biodegradable bone cement or muscle flap
|
|
|
Complications of sinus fistula repair:
|
complete or partial breakdown of repair, infection
|
|
|
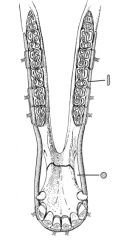
Indications for rostral mandibulectomy:
|
ossifying fibroma (most common), adamantinomas, fungal and parasitic disease
|
|
|
Complications of mandibulectomy:
|
recurrence of lesion, flaccidity of lower lip, protrusion of tongue
|
|
|
Term for wry nose:
|
campylorrhinus lateralis
|
|
|
Cause of wry nose:
|
genetic predisposition in Arabians, interuterine positioning
|
|
|
When is surgical repair of wry nose performed?
|
Delayed until foal is at least 2-3 months old so maxilla is strong enough to support implants
|
|
|
Approaches to wry nose correction:
|
rostal septal resection with ostectomy and stabilization with unilock plate, Steinman pins or LCP; distraction osteogenesis with type 2 external fixation device
|
|
|
Complications of wry nose repair:
|
infection, fixation failure, partial collapse of nasal passage
|
|
|
What is prognathia?
|
Asymmetry of maxilla and mandible with mandible shorter than maxilla
|
|
|
What is brachygnathia?
|
Asymmetry of maxilla and mandible with maxilla shorter than mandible
|
|
|
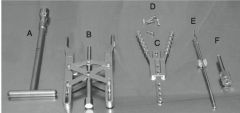
Treatment of prognathia or brachygnathia:
|
retard growth on the longer component with tension wiring of incisors and cheek teeth or application of a rachetdis system with distraction on the shorter side
|

