![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
What are the sizes of arterioles?
|
50 micrometers diameter and below
|
|
|
What 2 things affect the radius of arterioles?
|
Local influences
Reflexes |
|
|
How are arterioles tonically dilated?
|
By substances released by the endothelium which act on vascular smooth muscle (NO [nitric oxide] and PG)
|
|
|
An increase in shear stress leads to an increase in...
|
the release of NO and PG
|
|
|
Some vasolidator substances (e.g. ACh) cause dilation by...
|
releasing NO and PGs
|
|
|
What is myogenic tone?
|
Arterioles constrict in response to stretch (intravascular pressure)
|
|
|
What is the consequence of myogenic tone?
|
Maintains a high TPR, therefore high ABP
|
|
|
Which is greater - myogenic tone or tonic dilator influence of the endothelium?
|
Tonic dilator influence of the endothelium
|
|
|
In which tissues do you find the arterioles with the stronger myogenic responses?
|
brain and kidney arterioles
|
|
|
Why does blood flow remain constant over a wide range of mABP?
|
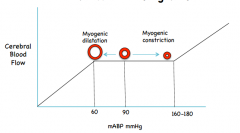
Myogenic responses to change in arterial resistance
|
|
|
What if functional/active hyperaemia?
|
Increase in blood flow to tissues due to increased metabolic activity.
|
|
|
What is the aim of functional/active hyperaemia?
|
To match blood flow to metabolism
|
|
|
Where is function/active hyperaemia most important?
|
Tissues that show large changes in metabolic activity
skeletal muscle, cardiac muscle, brain glandular tissue i.e. sweat glands and salivary glands |
|
|
How much does blood flow increase in:
skeletal muscle during strenuous exercise? cardiac muscle during a large increase increase in cardiac work? brain during increases in neurone activity? |
25
5 3 (regionally) |
|
|
Where do the substances act on arterioles in functional/active hyperaemia?
|
From the interstitial fluid
|
|
|
Which substances are considered to be the most important vasodilators in:
skeletal muscle cardiac muscle brain |
skeletal; high K+ (muscle action potential) and Pi + adenosine (ATP breakdown)
cardiac: high levels adenosine brain: high K+ (AP), CO2, H+ and adenosine, low O2 |
|
|
How is glandular tissue activated?
|
Sweat glands: activated by sympathetic cholinergic fibers
Salivary and GIT glands: activated by parasympathetic cholinergic fibres |
|
|
What molecule acts as a vasodilator and where does it come from?
|
Bradykinin
Acinar cells secrete secretion + kallikrein Kallikrein cleaves kininogen (plasma globulin) which produces bradykinin |
|
|
What is the innervation of arterioles and where is it most/least dense?
|
sympathetic noradnergic fibres
most dense in skin least dense in brain, cardiac muscle and lungs It can be overcome by functional hyperaemia in exercising muscle and cardiac muscle |
|
|
What is the effect of increasing sympathetic activity to arterioles?
|
More release of NAdr
Stimulation of alpha adrenoreceptors Vasoconstriction |
|
|
What 2 effects can sympathetic fibers have?
|
Increase ABP by acting on all arterioles
redistribute CO by acting on a particular tissue |
|
|
How do you neurologically vasodilate the arterioles?
|
tonic effect
remove the sympathetic activity vasodilation |
|
|
What do sympathetic cholinergic fibers supply?
What do they do? |
skeletal muscle
in addition to sympathetic noradnergic fibres existance in humans is doubted vasodilation via mAChR - only active in emotional stress |
|
|
What do parasympathetic cholinergic fibers innervate?
|
arterioles in cerebral, coronary circulation
genitalia and reproductive tissues vasodilation via mAChR role in brain + coronary circulation unclear |
|
|
When is parasympathetic cholinergic fiber activity in reproductive tissue important?
|
During intercourse, menstrual cycle and pregnancy
Increases blood flow to these tissues |
|
|
What are catecholamines and where do they come from?
|
NAdr and Adr
Adrenal medulla |
|
|
What does noradrenaline do?
|
weak constriction of all arterioles (alpha receptors)
Increase HR and contractility (beta 1 receptors) |
|
|
What does adrenaline do?
|
vasodilation in skeletal muscle (beta 2 receptors)
vasoconstriction everywhere else (alpha receptors) Increase HR and contractility (beta 1 receptors) |
|
|
What do antidiuretic hormone and vasopressin do and where do they come from?
|
vasoconstriction
pituitary gland important when ABP is low due to haemorrhage and dehydration |
|
|
What does angiotensin do and where does it come from?
|
vasoconstriction
action of renin from kidney important when ABP is low due to haemorrhage and dehydration |
|
|
5-hydroxytryptamine (5-HT) and serotonin
Where do they come from? What do they do? |
release from activated platelets at site of wound
vasoconstrict at site of wound reducing blood loss |

