![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
SA Node blood supply |
RCA (55%) Left circumflex (45%) |
|
|
Normal Heart rates of different intrinsic pacemakers |
SA Node: 60-90 bpm AV Node: 45-60 bpm His-Prkinje/BB Fibers: 30-45bpm |
|
|
AV Nodal Blood supply |
RCA (90%) Left circumflex (10%) |
|
|
Blood supply of Bundle Branches |
RBB: LAD LAF: LAD LPF: RCA or Left circumflex |
|
|
Mechanisms of DYSRHYTHMIA |
(1) Increased automaticity (2) Triggered activity - Early Afterpolarizations - Late Afterpolarizations (3) Reentry circuits - Two paths, one with a relatively slower refractory period |
|
|
Action of myocardial cell and relation to ion flow |
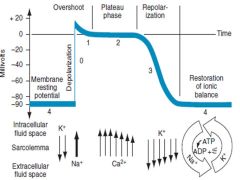
|
|
|
Overview of Anti-Arrhythmics |

|
|
|
Effect of of Anti-Arrhythmics on ECG intervals |
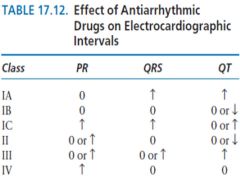
|
|
|
Adverse effects of Amiodarone |
Acute Effects
Common
Less Common
Drug Interactions |
|
|
Electrophysiological effects of digoxin |
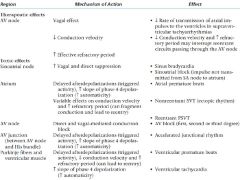
|
|
|
Causes of sinus bradycardia
|
Pharmacological
Non-pharmacological
|
|
|
Differential Diagnosis of causes of bradycardia |
|
|
|
Differential of regular vs irregular bradycardia
|
Regular
Sinus bradycardia Junctional bradycardia/Idioventricular Complete AV block (junctional escape) Atrial flutter with high degree block Irregular Sinus arrhythmia, pause or arrest Sinoatrial exit block (second degree) Atrial fibrillation with slow ventricular response Atrial flutter with variable block Second degree AV block, type I Second degree AV block, type II |
|
|
Sick Sinus Syndrome |
group of dysrhythmias from disease |
|
|
Type I vs Type II AV BLOCK |
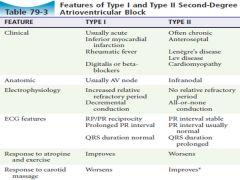
|
|
|
Bigeminy |
Extrasystole after every native beat |
|
|
Ashman phenomenon |
wide complex QRS complexes that follow a short R-R interval preceded by a long R-R interval
This wide QRS complex represents an aberrantly conducted complex that originates above the AV node
occurs because the duration of the refractory period of the myocardium is proportional to the R-R interval of the preceding cycle |
|
|
PAC vs PVC |
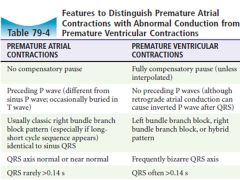
|
|
|
Cause of PVCs and Vtach |
Acute or previous myocardial infarction or ischemia |
|
|
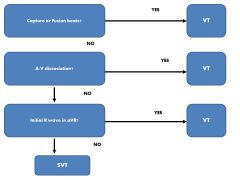
Tachycardia Algorithim |
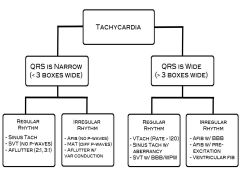
|
|
|
Causes of sinus tachycardia |
Drugs/Meds/Iatrogenic Anticholinergic Catecholamines Alcohol Caffeine Tobacco Cocaine β-blocker withdrawal Supraventricular tachycardia ablation
Medical Anemia Dehydration Exercise Anxiety Pain Pulmonary embolus Fever Infection Pericarditis Aortic or mitral regurgitation Myocardial infarction Pneumothorax Hyperthyroidism Hypoglycemia |
|
|
Potential Causes of A Fib |
Cardiac causes
|
|
|
2014 CCS Algorithim for who needs anticoagulation with a fib |
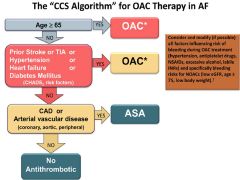
|
|
|
Relative risk reduction for stroke in patients with afib: - ASA - Wargarin |
ASA: 22% (NNT = 34) Warfarin: 64% (NNT = 14) |
|
|
CVA risk at different CHADS2 scores |
0: 1.9 1: 2.8 2: 4.0 3: 5.9 4: 8.5 5: 12.5 6: 18.2 |
|
|
2014 CCS reccomendations regarding OACs |
(1) for OAC with nonvalvular AF, dabigatran, rivaroxaban or apixaban in preference to warfarin
(2) for OAC patients with a mechanical prosthetic valve, rheumatic mitral stenosis or eGFR of 15-30 ml warfarin is prefered over NOACs
(3) Consider lower dose age >75 and CRF |
|
|
CCS ED algorithim for management of A Fib |
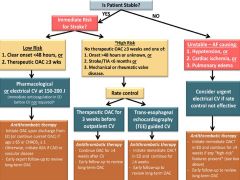
|
|
|
AVRT with orthodromic conduction (AV node 1st) |
|
|
|
AVRT with antidromic conduction (bypass 1st) |
|
|
|
Diseases associated with WPW |
Idiopathic* |
|
|
SVT with aberrancy versus VT |
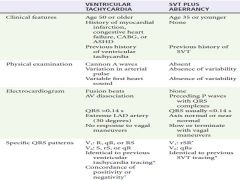
|
|
|
Criteria for Torsade de Pointes |
1. Ventricular rate greater than 200 beats/min |
|
|
Classification of Conditions that can lead to to Torsade de Pointes |
Pause Dependent (Acquired)
Adrenergic Dependent (Tachycardia Prompted) |
|
|
Rx for Torsade de Pointes (acquired) |
Empiric magnesium D/C any QT pronlonging agents Correct Electrolyte abnormalities Increased HR to shorten QT |
|
|
Ainsworth SVT vs VT |
|
|
|
ECG Findings to search for in syncope |
(1) Acute coronary syndrome |
|
|
Critical diagnoses to consider in patient with syncope |
Life threatining dysrhythmias Myocardial infarction
Outflow obstruction Critical aortic stenosis PE Pericardial tamponade Hypertrophic cardiomyopathy
Vascular catastrophes SAH Thoracic aortic dissection Abdominal aortic aneurysm Ectopic pregnancy
Hypovolemia/Hemorrhage/Anemia Toxic/Metabolic derangements Stroke |

