![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
Antigen
|
specific protein on an infectious agent that can be “recognised” by the immune system
|
|
|
Antibodies
|
specific proteins produced by the immune system that react with antigens (immunoglobulins : Ig)
|
|
|
B cells
|
produce antibodies
|
|
|
T cells
|
destroy pathogens via cells. Also coordinate the production of antibodies at first exposure
|
|
|
antibody response graph
|
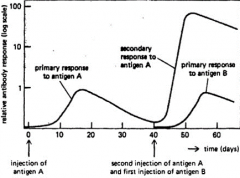
Antibody production starts off slow and then declines rapidly. next exposure, antibody production is faster as it is already in the system. it also lasts longer. over time if antigen is not encountered, antibody levels will fall. vaccines can be given to boost immunity. |
|
|
vaccination
|
The administration of an antigen to promote antibody production and memory.
|
|
|
natural vaccination
|
Exposure to living, normal pathogen Eg. Strangles Usually provides strong, long lasting immunity. Deliberately used in herd situations for low morbidity diseases. |
|
|
live vaccines
|
The living pathogen is modified so that it does not produce significant disease, or a non-pathogenic strain is used May cause a mild form of disease (e.g. Pi/BB)Replicate within the host – mimics primary exposure to natural infection Strong immune response |
|
|
inactivated vaccines
|
Whole pathogen which has been killed, or just part of the pathogen (Ag proteins) E.g. Bacterial vaccines No replication in host Smaller immune response Adjuvants are used to create slow-release effect+/- immune stimulants |
|
|
antisera
|
Creation of Antibody in one individual that are then harvested for use in another Colostrum is natural antisera Provides large dose of Antibody, but does not stimulate production or give any memory Not a vaccine To treat or prevent diseaseEg. Snake bite, tetanus |
|
|
benefits to vaccinating
|
Decrease suffering and risk of death No treatment for viral infections Some bacterial and parasitic infections cause severe damage too quickly to treat Group / herd benefits Reduce morbidity and mortality Suppress transmission Reduce public health risks Neonatal protection |
|
|
disadvantages to vaccinating
|
Adverse reactions Local tissue damage (adjuvants) Immune mediated disease Anaphylaxis Carcinogenesis? Rare |
|
|
problems with vaccines
|
Live vaccines have a risk of reverting to pathogenic type May cause foetal damage Can become contaminated Adjuvants in inactivated vaccines can cause allergic reactions |
|
|
why not vaccinate?
|
Cost and logistics Storage considerations Herd considerations Efficacy? - the ability to produce an desired or intended result MDA Live vs killed vs individual response Antibody response testing Cost UK legal limitations |
|
|
Maternally derived antibodies (MDA)
|
Antibody proteins are excreted in milk In the first 24-36 hours of life, neonates absorb whole Antibodies across the Gastro Intestinal Tract Antibodies from milk after 36 hours stay in the GIT These Antibodies will react with Antigens, protecting the neonate from infections They will also react with vaccine Antigens, destroying it before the immune cells can respond (less Antigens, lower efficacy) How long is it a factor? Depends on disease Depends on species Depends on colostrum absorption Hypervaccinated colostrum? On average, MDA effect is lost for most diseases by 8 – 16 weeks |
|
|
to jab or not to jab
|
Risk and consequence of disease To the individual To the herd/group To humans Which vaccines are available? How must it be used to achieve best vaccination? Age(s) of animals Will the vaccine need boosting? Duration of immunity? Will there be gaps in protection? (e.g. MDA) Can it / should it be combined with other vaccinations? |
|
|
Canine vaccinations
|
Parvo virus (live) Distemper virus (live) Hepatitis (adenovirus type 2) (live) Parainfluenza virus (live) Bordatella bronchiseptica bacteria (live) Rabies virus (inactivated) Coronavirus (inactivated) Leptospira icterohaemorrhagiae & canicola bacteria (inactivated) Leishmania (inactivated) Herpesvirus (inactivated) |
|
|
Essential puppy vaccines
|
Considered so due to mortality of diseases Combination of parvo, distemper, hepatitis Primary schedule2 vaccinations, 2-4 weeks apart, last must be older than 10 weeks Booster scheduleDepends on product license (1-3 years) Duration of immunity? |
|
|
other common vaccines for dogs
|
Parainfluenza, BB, coronavirus, lepto, rabies Consider risk of disease Lifestyle (socialisation, kennels, travel) Geography (lepto more common in wet environments) Prevalence of disease (coronavirus may be prevalent in certain areas) |
|
|
Feline vaccinations
|
Panleucopenia (live or inactivated) Calicivirus (live or inactivated) Rhinotracheitis herpesvirus (live or inactivated) Chlamydophila felis (live or inactivated) Bordetella bronchiseptica (live) FeLV - Feline leukaemia virus (inactivated) Rabies (inactivated) FIV - Feline immunodeficiency Virus (not licensed in UK) |
|
|
Essesntial kitten vaccines
|
Due to mortality and infectivity Enteritis (panleucopenia) Rhinotracheitis (herpes) Calicivirus Primary schedule2 vaccinations, 3 weeks apart. Must be 12 -16 weeks old at 2nd Booster schedule- annually |
|
|
Other common vaccines for kittens
|
FeLV, rabies Consider lifestyleI ndoor vs outdoor Travel Retroviruses Lifelong infection Vaccination after infection has no benefit Antibiotic testing? |
|
|
Rabbit Vaccines
|
Used to be complicated in rabbits Myxomatosis vaccine only lasted 6 months Some of vaccine had to be intradermal VHD could not be given within 2 weeks. New Nobivac vaccineContains myxo and VHDAnnual S.C. booster only |
|
|
Bovine Vaccines
|
Respiratory vaccines IBR (live or inactivated) BVD (live or inactivated) LungwormParainfluenza 3 (live or inactivated) Respiratory Syncitial virus (live or inactivated) Manheimia haemolytica prev. pasturella (inactivated) Scour vaccines BVDE. Coli (inactivated) Salmonella (inactivated) Rotavirus (inactivated) Coronavirus (inactivated) Mastitis vaccines E. Coli (inactivated) Staph aureus (inactivated) Other vaccines Leptospirosis (inactivated) Clostridial bacteria (inactivated and toxoid) Bluetongue virus (inactivated) Ringworm (live) Q fever (inactivated) |
|
|
Maternal vaccinations
|
Vaccinating pregnant cows can increase Antibodies content of colostrum and milk Provides scour protection for calvesEg. Lactovac vaccine given 2-6 weeks prior to calving gives greater Antibodies for rotavirus, coronavirus and E. coli Absorbed in first day, then provides protection within GIT Bottle formulations for calves of harvested, concentrated Antibodies |
|
|
Marker vaccines
|
For some diseases eg. IBR, BVD Antibody production remains high for life Need to differentiate between infected and vaccinated animals Marker vaccines have an antigen deleted, so that the Antibodies produced against the vaccine are different to the Antibodies produced against the agent. |
|
|
Sheep Vaccines
|
Clostridial bacteria (inactivated and toxoid) Enzootic abortion (chlamydiophilus abortus) D. nodosus (footrot bacteria) Bluetongue virus Mannheimia haemolytica and Pasteurella trehalosi (inactivated) Orf virus (live) Tetanus (toxoid) Toxoplasma gondii (live) |
|
|
Orf Vaccine
|
scabby mouth” - zoonosis Innoculation by skin scratch |
|
|
Natural vaccination
|
Disease only affects animals at certain ageEg. Border disease Expose unpregnant sheep to infective lambs before mating Immunity developed by the time they are pregnant No effect on mum – protects new pregnancies |
|
|
Equine Vaccines
|
Tetanus (toxoid) Equine Influenza (inactivated) Rotavirus (inactivated – colostrum) West Nile Virus (inactivated) Equine Arteritis Virus (inactivated) |
|
|
Standard UK horse vaccines
|
1st vac - 6 months 2nd vac - 7 months 3rd vac - 12 months 4th vac - 2 years 5th vac - 3 years etc.. |

