![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
Briefly describe Apoptosis
|
programmed cell death that allows the cell to die without lysing. The entire process is highly regulated and prevents an immune response, preserving surrounding tissue. Apoptosis can be initiated whenever a cell is too old, damaged, or just needs to be removed and allows for formation of new cells. Killing a cell is a last resort, therefore, there are a bajillion steps and interactions required to successfully kill the cell by apoptosis, which must go through a family of caspases.
|
|
|
Describe the mechanisms of apoptosis
|
Apoptotic cells will receive a signal to start shutting down which is propagated by cysteine proteases called capsizes. Small blebs (irregular bulging on the plasma membrane) will then form on the cell membrane. The nucleus will break down within the blebs and the cell breaks into several apoptotic bodies with functional organelles. Everything is then phagocytosed and safely removed from the area, minimizing surrounding tissue damage
|
|
|
Explain the intrinsic pathway of apoptosis
|
Intrinsic Pathway: something inside the cell (genetic mutation, virus, lots of intracellular stress, etc.) initiates apoptosis, which begins in the mitochondria, to activate apoptotic factors
|
|
|
explain the extrinsic pathway of apoptosis
|
Extrinsic Pathway: some external factor recognizes that the cell needs to die (certain hormones, too much cell growth, etc.). These signals require apoptotic cellular receptors of the apoptotic death domain.
|
|
|
Is apoptosis a normal process?? give examples that support your answer
|
Apoptosis is physiologically normal and important to keep rapidly growing cell populations of cells under control. Without apoptosis, what would happen to all the cells of the GI tract that need to be replenished every 3-4d? Normal apoptosis is also important in embryology (webbing of hands and toes, tail retraction)
|
|
|
What problems can arise from apoptosis gone wrong
|
Dysfunctions of apoptosis present pathophysiologic ally in cancer, viral infections, and neurodegenerative disorders (Huntington’s, lateral sclerosis, Parkinson’s, etc.)
|
|
|
explain necrosis
|
unprogrammed cellular destruction resulting in cell lysis and spillage of reactive enzymes from organelles. Enzymes then blindly act in the surrounding extracellular environment, eliciting an immune response, which can contribute to tissue damage, leading to chronic inflammation (discussed later). Unlike apoptosis, necrosis interrupts new cell growth, magnifying tissue damage.
|
|
|
what is the mechanism necrosis
|
Necrotic cells, like apoptotic cells, form small blebs. To differentiate the two in the early stages, note the shape of the necrotic nucleus changes. As necrosis progresses, blebs fuse and become larger, and organelles do not breakdown. Eventually, the cell will lyse and spill its activated lysosomal contents into surrounding tissue. This creates a mess of debris that the body has a difficult time removing --> gangrene
|
|
|
what controls necrosis? does it also regulate it?
|
a family of proteases controls (does not regulate) necrosis called cathepsin
|
|
|
Explain dry gangrene
|
results from an interference with arterial blood supply in extremities, and is a common result of diabetes and frostbite. Blockage of arterie -->ischemia -->cellular swelling --> cell lies
|
|
|
what are the symptoms of dry gangrene
|
blackened skin. Black color is due to chronic hemostasis in necrotic tissue, resulting in heme
interaction with bacteria. Bacterial H2S reacts with heme -->FeS, yielding a black color. There will be a distinct line in the skin indicating the point where oxygen saturation is insufficient to generate sufficient ATP. |
|
|
what is the treatment for dry gangrene
|
cut the affected area or it could also just fall off on its own
|
|
|
Describe wet gangrene
|
results from interference with venous blood supply, resulting in accumulation
of blood in the tissue. This results in bacterial growth as a result of hemostasis and a lesser appearance of darkened skin. This is most commonly found in patients with chronic pressure (bedsores), or as a result of infection, especially in burn patients (lots of fluid moves to the site of the burn). |
|
|
what are the symptoms of wet gangrene
|
less dramatic discoloration of the skin with an edematous, and clammy appearance from fluid buildup
|
|
|
what is the treatment for wet gangrene
|
O2 therapy, antibiotics, debridement, or with special sterile-bred maggots.
|
|
|
What methodology do you do in order to assess a case?
|
use SOAP (Subjective, Objective, Assessment, Plan for treatment)
|
|
|
what are the groups at highest risk for HBV
|
the groups with highest risk are patients on dialysis, people who have previously had STD treatment, people who work around blood, and those who got some artwork in the slammer.
|
|
|
explain the immune tolerant phase
|
the immune tolerant phase where the virus resides in hepatocytes and HBsAg is present on hepatocytes
|
|
|
explain Induction of Immune response
|
Induction of Immune response: begins as soon as virion replication in the immune tolerant phase causes cell lysis allowing virions to enter extracellular spaces. This phase elicits an immune response resulting in patient symptoms.
The immune response release of cytotoxic chemicals to kill hepatocytes with HBsAg present affects the surrounding region, but, the destruction of infected hepatocytes results in liver enzymes and contents (such as Bilirubin) to enter circulation |
|
|
what are symptoms of liver inflammation
|
• Fatigue: energy is required to mount a large scale immune response
• Hepatomegaly: inflamed liver increases in size • Athralgias: joint pain of larger proximal joints, common with large scale inflammation episodes • Polyarteritis nedosa: large red blotches on skin resulting from rupture of medium sized arteries. This is ultimately due to increased circulating estrogen and testosterone that is no longer cleared as a result of less hepatocyte function. These hormones affect the dilation and strength of the vessel walls. • Mambranoproliferative Glomerulonephritis • Jaundice |
|
|
explain bilirubin and how it relates to messed up hepatocytes
|
RBCs go through reticular endothelial system in liver and spleen that look for senescent RBCs (>120d old). RBC breakdown results in heme processing within the reticular endothelial system. damaged hepatocytes cannot move Bilirubin efficiently into the GI tract for clearance resulting in overflow of Bilirubin into blood and eventually to urine.
|
|
|
what are the 3 HBV immune outcomes? describe them
|
1. Immune Stage: all HBsAg is completely
cleared from all hepatocytes 2. Inactive carrier stage: no injury or chronic inflammation, but some lingering cells can cause acute hepatitis induced by some insult. 3. Chronic Hepatitis: (she sort of glossed over this) could lead to liver failure, jaundice, impaired glycogenolysis and gluconeogenesis, reduction in bile salt production, impaired hormone clearance (cortisol, aldosterone, estrogens...). The chronic stage is often a result of a poor T-cell response and continuous destruction of the liver leading to cirrhosis. |
|
|
explain acute inflammation
|
Acute inflammation: an insult causes an immediate response leading to vascular dilation and cellular reaction (getting immune cells into tissues) allowing the immune cells to quickly get to the affected area to eliminate pathogens. Ultimately, leukocytes will be the cause of tissue injury.
|
|
|
What are the steps for vascular dilation
|
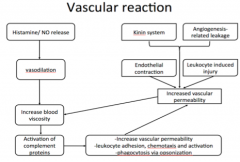
|
|
|
What are the steps for cellular reaction?
|
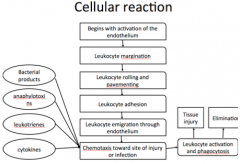
|
|
|
explain chronic inflammation
|
there is continuous T-cell activation resulting in increased TNF-alpha. The specific role of TNF-alpha is to allow the proliferation of fibroblasts --> fibrosis. This ultimately changes the structure of the tissue. Since we know that structure leads to function, it is the more fibrous tissue that leads to less function in tissue in chronic states. For example, fibrosis in the liver --> scarring -->cirrhosis. Note (in red arrows), that the increase in TNF-alpha contributes to a cyclic affect to continuously activate more T-cells further compounding chronic inflammation.
|
|
|
what are the steps for chronic inflammation
|
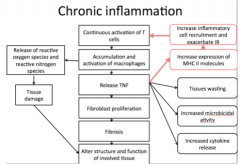
|
|
|
Describe Diabetic Nephropathy
|
In rats, she found that inflammation helped to progress diabetic nephropathy. She also found that there were a whole lot more macrophages (by CD68 and MCP-1 protein markers) in diabetic nephrons. The distribution of macrophages was also different between male and female mice. That’s some weird, wild, stuff.
|

