![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
65 Cards in this Set
- Front
- Back
|
What are 5 signs of stroke?
|
sudden numbness/weakness in face arm or leg, esp. on one side of body
sudden confusion, trouble speaking/understanding sudden trouble seeing in one or both eyes sudden trouble walking/dizziness/loss of balance or coordination sudden, severe headache w. no known cause |
|
|
definition of aphasia (Rosenbek, LaPointe and Wertz)
|
impairment due to:
acquired & recent damage of the CNS. Effects ability to comprehend and formulate language. Multimodal disorder w/ variety of impairments in: auditory comprehension, reading, oral-expressive language and writing. Disrupted lg. may be influenced by physiological inefficiency or impaired cognition, but it cannot be explained by dementia, sensory loss, or motor dysfunction. |
|
|
What is the exception to Rosenbek, LaPointe and Wertz' definition of aphasia?
|
Primary Progressive Aphasia...
doesn't "erupt", it "creeps" |
|
|
disrupted language can be influenced by...?
|
a. physiological inefficiency
b. impaired cognition |
|
|
disrupted language cannot be explained by...
|
dementia
sensory loss motor dysfunction |
|
|
Aphasia is...
|
acquired & recent (except for primary progressive aphasia)
damage to CNS a multimodal disorder explained by physiological inefficiency |
|
|
name the 4 modalities affected by aphasia
|
oral-expressive language
auditory comprehension reading writing |
|
|
Name 4 causes of aphasia
|
CVA (cerebrovascular accident)
infection (e.g., meningitis) trauma (TBI) tumor |
|
|
What are the 8 risk factors for stroke?
|
high blood pressure
diabetes mellitus smoking high cholesterol heavy drinking obesity lack of exercise heart disease |
|
|
name and define the two types of blood pressure.
|
Systolic: the highest number. Pressure created by contraction of heart muscle and elastic recoil of aorta
Diastolic: lower number. Reflects resistance in small arteries throughout body & load against which the heart must work. The relaxation of the heart ventricles between beats. |
|
|
Healthy adult blood pressure?
|
110/75
|
|
|
blood pressure at age 60?
|
130/90
|
|
|
measurement used for blood pressure?
|
mmHg
millimeters mercury |
|
|
to reduce risk of stroke by ____%, one should lower BP by ____mmHg systolic and ____mmHg diastolic
|
38%
10-12 mmHg systolic 5-6 mmHg diastolic |
|
|
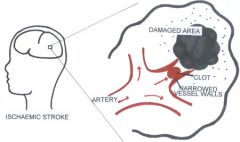
name two main categories of CVAs
|
Ischemic
Hemorrhagic |
|
|
Name the 2 types of Ischemic strokes.
|
Thrombotic stroke
Embolitic stroke |
|
|
When we don't know whether stroke is caused by a thrombus or an embolism, we call it a...
|
thrombo-embolitic stroke
|
|
|
___% of strokes are Ischemic.
|
75-85%
|
|
|
Ischemic (Occlusive) strokes usually occur in the ...
|
Middle Cerebral Artery (MCA)
or Internal Carotid Artery (ICA) |
|
|
blockage results in...
|
cerebrovascular inefficiency
(deprivation of blood flow) |
|
|
define cerebral thrombosis
|
a blood clot in a plaque-narrowed artery which blocks blood flow.
|
|
|
Define TIA
|
Transient Ischemic Attack
A warning stroke. Temporary blockage that causes a sudden, immediate reduction of blood flow (temporary cerebrovascular insufficiency) |
|
|
What happens with a TIA?
|
Temporary cerebrovascular insufficiency lasting a minute or hours. No cell death occurs, but displays immediate consequence.
|
|
|
A TIA indicates a problem in the __________________.
|
Internal Carotid Artery
|
|
|
Describe the treatment for a TIA.
|
administration of Clotbuster (enzymes that dissolve clot) to break up clot.
|
|
|
1. Thrombus = ?
2. Embolism = ? |
1. plug, blockage
2. blockage caused by clot that was formed elsewhere (often in the heart) that travels through blood stream until it gets lodged in a smaller vessel |
|
|
describe ischemia, infarct, and astrocytes
|
Ischemia is the occlusion, Infarct is the damaged tissue that liquifies and dissipates leaving a cavity, astrocytes are the rim around the cavity.
|
|
|
A thrombus is located _________.
|
... in its place of origin.
|
|
|
2 causes of thrombosis...
|
ARTERIOsclerosis: variety of pathological conditions causing thickening, hardening, loss of elasticity of vessel walls.
ATHEROsclerosis: FORM OF arteriosclerosis. Thickening due to LOCALIZED deposits of lipids (fat and fibrous material) |
|
|
Describe a cerebral embolism.
|
Sudden, NO TIA. Clot forms somewhere else, circulates and then plugs when it gets to vessel too small to pass. Commonly originate from wall of heart.
|
|
|
Arteriosclerosis and Atherosclerosis often occur in 3 spots. Name them.
|
MCA, ICA, Basilar Artery
|
|
|
Can a thrombus be part of an embolism?
|
No, but an embolism can be part of a thrombus.
|
|
|
What is the I.V. med used when a person has a thromboembolitic cerebrovascular accident?
|
T-pa: Tissue plasminogen activator (clotbuster)
|
|
|
Name and describe a non-pharmeceutical method to removing a thrombus.
|
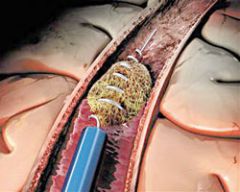
Clot Retriever
|
|
|
can an embolism be 'fixed' or 'stationary'?
|
Yes. Both a thrombus and an embolism can be 'fixed' or 'stationary', but only a thrombus exists in its 'place of origin'.
|
|
|
20% of all strokes are ________.
|
Hemorrhagic
|
|
|
What causes a hemorrhage?
|
Extreme fluctuation in blood pressure.
Traumatic injury Weakness in blood vessel wall |
|
|
What happens in a hemorrhage?
|
break in blood vessel wall, blood flows out, pools around surrounding tissue, rapidly expands.
|
|
|
___% of hemorrhagic stroke victims survive.
|
50% (but less than half of those that survive are functional)
|
|
|
Name the 2 major categories of hemorrhagic stroke.
|
INTRAcerebral: within brain or brain stem
EXTRAcerebral: btwn brain & skull (rupture of vessels in meninges) |
|
|
Extracerebral hemorrhage is frequently caused by...
|
head injury
|
|
|
Name the 3 types of extracerebral hemorrhage
|
subdural
subarachnoid (most common) extradural |
|
|
What is the most common extracerebral hemorrhagic event and what is it characterized by?
|
subarachnoid hemorrhage: severe, violent headache
nausea vomiting |
|
|
what is the location of a subarachnoid hemorrhage.
|
under the arachnoid membrane... geesh!
|
|
|
Can a subarachnoid hemorrhage be prevented?
|
Yes. Can be identified and Dx'd before rupture and surgically repaired.
|
|
|
describe what happens when a person has a subarachnoid hemorrhage...
|
swelling & blood from hemorrhage compress neighboring structures - this is why recovery of skills happens. Swelling goes down, skills come back.
|
|
|
an aneurysm is most common in people ages ___-___.
|
can occur at any age, but is most common in 25-50 yo
|
|
|
What is the most common cause of a subarachnoid hemorrhage?
|
aneurysm
|
|
|
What are the causes of an aneurysm?
|
congenital (malformation)
anything that could weaken vessel wall (TBI) |
|
|
what are the most common locations for an aneurysm?
|
ICA (30%)
ACA (30%) MCA (25%) BA (10%) |
|
|
90% of _______________ hemorrhages are due to high blood pressure.
|
Intracerebral
|
|
|
What are the structures that are affected by an intracerebral hemorrhage?
|
thalamus
basal ganglia brainstem cerebellum |
|
|
Why is there an increase in thalamic stroke?
|
easier to block the smaller vessels that run off the MCA... can be result of clotbuster meds
|
|
|
What determines the manifestation of an intracerebral hemorrhage?
|
the size and location of hemorrhage will manifest in different symptoms by application of pressure on neighboring tissue
|
|
|
t/f Tissue affected by an intracerebral hemorrhage is destroyed
|
False. Pressured is applied, but tissue is not destroyed.
|
|
|
Give and spell term that describes the temporary affectation of surrounding structures.
|
diaschesis
connected areas "go on strike" for a few weeks. Return in 3-6 months. |
|
|
Provide timeline of neurological stability and recovery post-stroke.
|
wait 2-3 weeks before giving prognosis
effects are continuous for awhile after 3-4 wks, damage is chronic acute events will dissipate and stabilize Now recovery will start to occur. |
|
|
If patient does NOT have an ischemic attack, they may have a ...
|
Reversible
Ischemic Neurological Deficit |
|
|
1. acute=
2. stable= |
1. Event is not over. Damage still occuring
2. No more damage. Stroke not getting worse. |
|
|
acute effects of stroke last approximately _____ hours.
|
24-72 hours
|
|
|
when do we determine severity?
|
once patient is stable, however if treatment is started immediately (within first month) improvements may be greater.
|
|
|
Recovery of occlusive stroke
|
gradual but continuous months past onset
would improve w/o Tx, but improvements are greater w. Tx |
|
|
Recovery of hemorrhagic stroke
|
very little progress in first few months
recovery is delayed, but it will happen |
|
|
Recovery of TBI
|
classic stair step (up/plateau... up/plateau...)
if injured when young, problems can occur later: adolescents may have problems with lang. & memory |
|
|
Name 4 kinds of stroke
|
TIA: quick attack & then over (on/off)
RIND: stroke in progress Occlusion: (acute/chronic) Hemorrhage: (acute/chronic) |

