![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
245 Cards in this Set
- Front
- Back
|
Functions of the Lymphatic system |
1. Returns excess interstitial fluid to the cardiovascular system 2. Defense against microorganisms 3. Absorption of dietary lipids from the digestive tract 4. Harbors leukocytes |
|
|
Lymphatic vessels |
Transport lymph Leukocyte movement |
|
|
Lymph nodes |
1. Primary organ of immunity 2. Filter lymph 3. Monitor lymph for pathogens |
|
|
Spleen |
1. Destroys worn-out erythrocytes 2. Monitors blood for pathogens 3. Reservoir for blood |
|
|
Tonsils 5 |
1. Provides immune activity around oral cavity 2. Traps and digest bacteria and particulate matter |
|
|
Function of Thymus |
Site of T-cell development |
|
|
Bone marrow |
1. Site of luekocyte production 2. Site of B-cell development |
|
|
Peyer's patches |
1. Provides immune surveillance around small intestines 2. Reduce bacterial numbers in GI tract 3. Important for immune development via sampling of gut microbiota |
|
|
Appendix |
1. Similar function to peyer's patches 2. Harbors beneficial bacterial for recolonizing colon |
|
|
Associated lymphoid tissues (SALT, GALT, MALT) |
1. Deep to skin and mucous epithelia 2. Concentration of macrophages and lymphocytes in connective tissue 3. Monitor for pathogen breach of skin and mucous membrane |
|
|
What filters lymph? |
Macrophages & phagocytosis |
|
|
What monitors lymph for pathogens? |
Lymphocytes & adaptive immunity |
|
|
What destroys worn-out erythrocytes? |
Macrophages in red pulp |
|
|
What monitors blood for pathogens? |
Lymphocytes in white pulp |
|
|
What assists in luekocyte production? |
Hematopoietic stem cells |
|
|
What is the directional flow of lymph? |
One direction: from the body's tissues towards the heart |
|
|
Pathway of lymph flow |
1. Tissue interstitial fluid 2. Lymphatic capillaries 3. Lymphatic collecting vessels 4. Lymph nodes 5. Lymphatic collecting vessels 6. Lymphatic trunk 7. Lymphatic ducts 8. Junction of subclavian veins & internal jugular veins 9. Venous return to the right heart |
|

What are these areas drained by? |
A. Drained by right lymphatic duct B. Drained by thoracic duct |
|
|
For lymph to enter lymphatic capillaries, what would have to be the relationship between the pressure of the interstitial fluid and the pressure inside the Lymphatic system? |
Interstitial fluid pressure needs to be greater than pressure inside lymphatic system |
|
|
What are lymphatic capillaries? |
Blind-ended tubes that allow one-way entry of interstitial fluid into the Lymphatic system |
|
|
Characteristics of lymphatic capillaries |
More permeable (compared to blood capillaries) Overlapping endothelial cells to form flap-like minivalves which ensures one-way flow of lymph |
|
|
Are lymphatic capillaries more or less permeable during inflammation? |
More permeable |
|
|
During inflammation, lymphatic capillaries have a greater ability to absorb what? |
Cellular debris & pathogens |
|
|
Due to high permeability of lymphatic capillaries, what has an easier time entering? |
Metastatic cancer cells & leukocytes |
|
|
Name the components, and their function, of leukocytes that provides an environment to help in the efficient removal of pathogens |
Macrophages- phagocytosis; antigen presenting cell B & T lymphocytes- adaptive immunity response Dendritic cells- antigen presenting cell Reticular cells- produce fibers Reticular fibers- provide framework for immune cell interaction |
|
|
Locations of lymph nodes |
1. Clustered along lymphatic collecting vessels 2. Major junction points of body parts 3. Along the intestinal tract |
|
|
What do lymph nodes form at major junction points of body parts? |
Lymph node plexus |
|
|
Lymph nodes primary functions |
Filter lymph & activate the adaptive immune response |
|
|
3 Steps to filtering lymph |
1. Lymph enters node through afferent vessels 2. Macrophages phagocytize microbes and cellular debris, while lymphocytes monitor lymph for specific pathogens 3. Lymph exits node though efferent vessels |
|
|
A. What does the Lymphatic system lack that causes its vessels to have extremely low pressure? B. As a result, lymph flow is assisted by what? |
A. dedicated pumping organ B. Contraction of neighboring skeletal muscles (similar to venous return assistance) |
|
|
Immunity is the ability to do what? |
Defend against pathogens & abnormal host cells |
|
|
Two categories of immunity |
Innate defense Adaptive defense |
|
|
Characteristics of innate defense |
In place from birth Non-specific Respond immediately |
|
|
Characteristics of adaptive immunity |
1. ID specific pathogens/abnormal cells 2. Follow innate response 3. Capability increase with repeat exposure (memory) |
|
|
What category of defense is the First Line of Defense? Components? |
Innate defense; Physical barriers: Intact skin Intact mucous membranes |
|
|
Forms a continuous dry mechanical barrier to prevent entry of most pathogens and toxins. What is the component of this function/characteristic? |
Intact skin & Intact mucous membrane |
|
|
Secretions are acidic, salty and contains the digestive enzyme, lysozome. What is the component of this function/characteristic? |
Intact skin |
|
|
Normal bacterial microbiota out-compete pathogens for space and resources. What is the component of this function/characteristic? |
Intact skin & Intact mucous membrane |
|
|
Sticky mucus traps microbes; ciliary action (in respiratory tract) mechanically removes them. What is the component of this function/characteristic? |
Intact mucous membranes |
|
|
A variety of digestive enzymes destroy pathogens (lysozomes, gastric and intestinal enzymes). What is the component of this function/characteristic? |
Intact mucous membranes |
|
|
Acidic secretion inhibits growth. What is the component of this function/characteristic? |
Intact mucous membrane |
|
|
Dynamic movements (urine & fecal movement, breathing) reduce bacterial numbers. What is the component of this function/characteristic? |
Intact mucous membrane |
|
|
Reflex activity (coughing, sneezing, vomiting, diarrhea) increase rate of pathogen clearance. What is the component of this function/characteristic? |
Intact mucous membrane |
|
|
What category of defense is the Second Line of Defense? Components? |
Innate Cellular & chemical defenses: 1. Antimicrobial compounds 2. Complement 3. Fever 4. Iron-binding compounds 5. Inflammation 6. Interferons 7. Phagocytes 8. NK cells |
|
|
Function/characteristics in second line of defense Phagocytes |
1. Engulf and destroy pathogens & cell debris. 2. Macrophage and dendritic cells process and present antigen for adaptive immunity (APC's). |
|
|
Function/characteristics in second line of defense NK cells |
Attack and destroy virally-infected or abnormal host cells (non-specific mechanism). |
|
|
Function/characteristics in second line of defense Inflammation |
1. Slows the spread of pathogens, 2. increases blood flow and 3. attracts Phagocytes; 4. stimulates tissue repair. |
|
|
Function/characteristics in second line of defense Fever |
Slight increase in body temperature inhibits bacterial growth and increases host metabolic rate. |
|
|
Function/characteristics in second line of defense Interferons |
Secreted by virally-infected host cells to slow spread of virus and attract NK cells & Tc cells. |
|
|
Function/characteristics in second line of defense Complement |
Plasma protein which enhances inflammation, osponize bacteria and cause lysis of bacteria cells. |
|
|
Function/characteristics in second line of defense Iron-binding compounds |
Strongly bind iron to make it less available to pathogens |
|
|
Function/characteristics in second line of defense Antimicrobial compounds |
Peroxidases are lethal to bacterial.
Lysozome digest bacterial wall cells.
|
|
|
What category of defense is the Third line of defense? Components? |
Adaptive immunity: 1. B lymphocytes 2. Antibodies 3. T lymphocytes |
|
|
Function/characteristics in third line of defense B lymphocytes 2 |
memory B cell provide long-term immunity against subsequent infection.
Plasma cells produce antibodies to target specific pathogens for destruction and removal. |
|
|
Function/characteristics in third line of defense Antibodies |
Activates complement, neutralizes pathogens & toxins, osponizes bacteria to enhance phagocytosis.
Immune proteins which bind to specific antigen to facilitate its removal. |
|
|
Antibody, IgM |
Bond to B-cell membranes; B-cell and complement activation; Initial antibody response. |
|
|
Antibody; IgG |
Primary serum antibody; Crosses the placenta to provide infant with serum immunity; Activates complement |
|
|
Antibody; IgA |
Associated with mucous membrane; Binds antigen to mucus; found in tears, saliva & mucus; Secreted in breast milk to provide infant with mucosal immunity |
|
|
Antibody; IgE |
1. Binds to mast cell and basophil membranes to trigger symptoms of Type I Hypertensitivity 2. Antibody response against worms and other parasites. |
|
|
What is the function/characteristic of this third line of defense? T Lymphocytes |
1. Helper T-cells secrete a variety of cytokines to direct the immune response. 2. Cytotoxic T-cell attacks and destroys virally infected and abnormal host cells |
|
|
Function of neutrophil |
1. Circulating short-lived phagocyte (~4 days) 2. Most abundant leukocyte; most common Phagocyte 3. Enters tissue during inflammation 4. Ingests and destroys cellular debris and pathogens |
|
|
Function of eosinophil |
1. Secretes chemicals to attack worms and other parasites 2. Implicated with type I Hypertensitivities |
|
|
Function of basophil |
1. Secretes histamine to trigger inflammation 2. Causes symptoms of Type I Hypertensitivity |
|
|
Function of monocyte 2 |
1. Circulating phagocyte 2. Matures into macrophage upon entering tissues
|
|
|
Function of macrophage |
Tissue phagocyte; processes and presents antigen to lymphocytes |
|
|
Specialized macrophages |
Alveolar macrophage: lung macrophage Dendritic cell: epidermal macrophage Microglial cell: CNS macrophage Kupffer cell: hepatic macrophage |
|
|
Function of Natural killer cell (NK cell) as a leukocyte |
1. Secretes perforins to destroy virally infected or abnormal host cells. 2. Cytotoxic activity is not specific to any particular antigen |
|
|
What is the component of this function? Effector form coordinates immune activity via cytokine release |
Help T lymphocyte TH cell |
|
|
What is the component of this function? This type of cell activated determines antibody versus cytotoxic cell response. |
Help T lymphocyte TH cell
|
|
|
What is the component of this function? These memory cells provides long term immunity against subsequent exposure. |
B Lymphocytes B cell
Help T Lymphocyte TH cell
Cytotoxic T Lymphocyte TC cell |
|
|
What is the component of this function? Effector form secretes perforins to destroy virally infected or abnormal host cells. |
Cytotoxic T lymphocyte Tc cell |
|
|
What is the component of this function? This activity is specific to a particular antigen. |
Cytotoxic T lymphocyte Tc cell |
|
|
What is the component of this function? Implicated with Type IV Hypertensitivities and transplant rejection. |
Cytotoxic T lymphocyte Tc cell |
|
|
What are the two most common types of Phagocytes? |
Neutrophil Macrophage |
|
|
What Phagocytes engulf and digest pathogens and cellular debris? |
Neutrophil Macrophage |
|
|
Which phagocyte cannot serve as an antigen presenting cell? |
Neutrophil |
|
|
Which phagocyte can process and present antigen to activate adaptive immunity? |
Macrophage |
|
|
Steps to phagocytosis |
1. Phagocyte bind and engulf antigen into phagosome. 2. Lysosomes fuse with phagosome to make phagolysosome. 3. Antigen & enzymes mix in phagolysosomes. 4. Antigen degrades. 5. Macrophage displays antigen fragments on membrane surface to activate adaptive immunity. 6. Neutrophils void antigen residue via exocytosis |
|
|
What are three primary fundamentals to adaptive immunity? Define them. |
Specificity- identifies specific pathogens
Memory- protects against subsequent exposure
Self vs non-self- IDs what belongs and what doesn't |
|
|
What molecules trigger an immune response? |
Antigens |
|
|
What molecule is unique to a certain type of cell or organism? |
Antigen |
|
|
Antigens can be specifically found where? |
In B-cell & T-cell receptors |
|
|
The process where body cells display antigen fragments of the pathogen in MHC molecules on their cell membranes |
Antigen presentation |
|
|
Cell-mediated immunity chart |
1. T-cell recognizes antigen (via APC)
2a. Helper T-cell activation = macrophage & B-cell activation
2b. Cytotoxic T-cell activation = kill infected or abnormal host cells
3. Helper and cytotoxic = memory cells provide subsequent protection |
|
|
Inflammatory response. Part 1-effects of inflammatory mediators |
1. Tissue damage occurs. 2. Damaged & mast cells release inflammatory mediators. 3. Inflammatory mediators trigger: A. Vasodilation of arterioles causing redness & heat. B. Increased capillary permeability causing swelling (edema). C. Pain causing possible loss of function. D. Recruitment of other cells: Chemotaxis leading to part 2 |
|
|
The inflammatory response: Part 2- phagocyte response |
1. Local macrophage activated. 2. Neutrophil migrate by Chemotaxis to the damaged tissue and phagocytize bacteria & cellular debris. 3. Monocytes migrate to the tissue by Chemotaxis and become macrophages, which phagocytize pathogens & cellular debris. 4. Bone marrow increases leukocyte production, leading to leukocytosis. |
|
|
T-cell maturation (4 steps) |
1. Cells of the lymphoid line divide in the bone marrow. 2. Immature T-cells exit the bone marrow and migrate to the thymus. 3. The thymus stimulates T-cell maturation and destroys self-reactive T-cells. 4. Mature naive T-cells migrate to lymphoid organs. |
|
|
A. Examples of antigens from an intracellular source. B. Examples of antigens from an extracellular source. |
A. Virus or cancer B. Bacteria, worms, fungi, protozoa |
|
|
Antigens from an intracellular source are presented via? Leading to? |
MHC I molecules Leading to cytotoxic T-cell activation |
|
|
Antigens from an extracellular source are presented via? Leading to? |
MHC II molecules
Leading to helper T-cell activation |
|
|
Antibody-mediated immunity chart |
1. B-cell recognizes antigen 2. Helper T-cell activates B-cell 3. Plasma cell produces and secretes appropriate antibody. Facilitates antigen clearance. 4. Memory cells provide subsequent protection. |
|
|
B-cell maturation (3 steps) |
1. Cells of the lymphoid line divide in the bone marrow. 2. B-cells mature in bone marrow, where self-reactive B cells are destroyed. 3. Mature naive B-cells exit the bone marrow and take up residence in lymphoid organs. |
|
|
Antibody structure |
1. Two arms are antigen binding sites where each end is specific for one type of antigen. 2. The base allows for bonding of host macrophages (only if antigen is bound to ABS) |
|
|
What is formed when antibodies are activated? |
Immune-complexes with their antigens |
|
|
Describe what occurs during the first exposure to an antigen and what is it called? |
Called the primary immune response. Relatively slow Weak and short lived Person experiences illness |
|
|
Describe the secondary immune response |
Much faster More intense Longer-lasting Person typically doesn't experience illness |
|
|
Compare the primary vs secondary immune response Lag phase |
Primary longer Secondary shorter |
|
|
Compare the primary vs secondary immune response Time until antibody peak |
Primary- longer time Secondary- shorter time |
|
|
Compare the primary vs secondary immune response Primary antibody |
Primary- IgM Secondary- IgG |
|
|
Compare the primary vs secondary immune response Duration of response |
Primary- shorter duration Secondary- longer duration |
|
|
Antibody mediated immunity Active immunity vs passive immunity |
1. Makes antibodies 2a. Naturally acquired through exposure via infection. 2b. Artificially acquired through vaccination. 3. Memory cell formation and lasting protection. |
|
|
Antibody mediated immunity Active immunity vs passive immunity |
1. Receives antibodies 2a. Naturally acquired through passage from mother to fetus and in breast milk. 2b. Artificially acquired through injection of antibodies to toxins or venoms. 3. No memory cells formed, no lasting protection |
|
|
What is the most protective form of active and passive antibody mediated immunity? |
Active immunity, naturally acquired |
|
|
What is the most dangerous way of acquiring immunity? |
Active, Natural exposure |
|
|
Causes and characteristics/symptoms of Edema |
Blockage of lymphatic drainage leads to accumulation of intestinal fluids (ISF)
Increase in ISF volume disrupts capillary exchange |
|
|
Causes and characteristics/symptoms of Tonsillitis |
1. Inflammation of tonsils, caused by bacteria or virus 2. May lead to middle ear infection (ottis media) 3. Removal of tonsils is now rare except in chronic or recurrent cases |
|
|
Causes and characteristics/symptoms of Lymphoma |
1. Cancer of lymphoid tissues, most commonly lymph nodes 2. Hodgkin's Lymphoma is typically easier to treat than non-Hodgkin's Lymphoma |
|
|
Causes and characteristics/symptoms of Type I Hypersensitivity |
1. Immediate allergies to harmless allergens 2. B-cells produce excess IgE which binds to mast cells and basophils 3. Subsequent exposure to allergen causes rapid histamine release 4. Anaphylaxis may be mild and local, or systemic and life-threatening |
|
|
Causes and characteristics/symptoms of Type IV Hypersensitivity |
1. Delayed allergies, taking 2-3 days for symptoms to appear 2. T-cells are sensitized to allergens 3. Contact dermatitis is a typical result |
|
|
Causes and characteristics/symptoms of Autoimmunity |
1. Immune response against self leafs to tissue destruction 2. Examples of autoimmune disease: Type I diabetes Lupus Rheumatoid arthritis Graves' disease Multiple sclerosis |
|
|
Causes and characteristics/symptoms of AIDS |
1. HIV infects helper T-cell and macrophage 2. Loss of helper T-cell leads to inability to direct the immune response properly 3. Patient succumbs to unusual opportunistic infections and rare cancers |
|
|
Equation for aerobic respiration |

|
|
|
Provisions of C6H12O6 |
Provided by the digestive system and body stores via the blood |
|
|
Provisions of 6O2 |
Provided by the respiratory system via the blood |
|
|
Provision of 6CO2 |
Removed by the respiratory system via the blood |
|
|
Provisions of 6H2O |
Joins the pool of body water |
|
|
List the events of human respiration in the order of the flow of Oxygen |
Pulmonary ventilation Pulmonary gas exchange Gas transport Tissue gas exchange Cellular respiration |
|
|
List the events of human respiration in the order of the flow of carbon dioxide |
Cellular respiration Tissue gas exchange Gas transport Pulmonary gas exchange Pulmonary ventilation |
|
|
Describe pulmonary ventilation |
Breathing |
|
|
Describe pulmonary gas exchange |
Between lungs and blood |
|
|
Describe gas transport |
Through blood |
|
|
Describe tissue gas exchange |
Between blood and respiring tissues |
|
|
Describe cellular respiration |
ATP synthesis |
|
|
Functions in the Respiratory System |
1. Assists with venous and lymphatic returned 2. Entry and absorption of oxygen 3. Excretes carbon dioxide 4. Regulates blood pH and blood pressure 5. Smell 6. Vocalization |
|
|
Functions & hormones of the nasal cavity |
Warms, filters and moistens inhaled air Dissolution and binding of odorant molecules to trigger olfaction |
|
|
Functions & hormones of the pharynx |
Channels air to lower respiratory tract Channels food & drink to esophagus (digestive system) |
|
|
Functions & hormones of the larynx |
1. Channels air to trachea 2. Superior epiglottis covers glottis to close lower respiratory tract during swallowing 3. Vocal chords produce sound, to be shaped into speech by oral cavity |
|
|
Functions & hormones of the trachea |
Channels air into bronchi of lung Remains patent due to cartilage rings in the wall |
|
|
Functions & hormones of the lungs |
Relatively hollow, filed with branching bronchi, bronchiole & alveoli Dramatically increases surface area for rapid diffussion of respiratory gases |
|
|
Functions & hormones of the pleura |
Serous membrane reduces friction between lungs & thoracic cavity wall Ensures lungs remain inflated against cavity wall due to surface tension and negative pressure gradient |
|
|
Functions & hormones of the bronchi |
Channel air to the lungs Remain patent due to cartilage rings/plates in wall |
|
|
Functions & hormones of the bronchioles |
Channel air into alveoli for gas exchange Smooth muscle in walls allow for constriction and dilation of lumen |
|
|
Functions & hormones of the alveoli |
1. Thin-walled air sacs which allow gas exchange with pulmonary capillaries. 2. Type II alveolar cells produce surfactant to minimize surface tension and prevent alveolar collapse. 3. Macrophage phagocytize microbes, particulate matter and cellular debris |
|
|
Functions & hormones of the diaphragm |
1. Primary inspiratory muscle; pulls downward during contraction. 2. Contraction increases chest volume during inspiration; decreasing intrapulmonary pressure 3. Relaxation decreases chest volume during expiration; increasing intrapulmonary pressure |
|
|
Functions & hormones of the external intercostals |
1. Inspiratory muscles; pulls outward and upward during contraction. 2. Contraction increases chest volume during inspiration; decreases intrapulmonary pressure 3. Relaxation decreases chest volume during expiration; increases intrapulmonary pressure |
|
|
Functions & hormones of the respiratory epithelium |
1. Ciliated epithelial mucosa traps particulate matter and microbes. 2. Ciliary action removes mucus with trapped particles (mucociliary escalator). 3. Lines nasal cavity, larynx, trachea, bronchi & bronchioles (but not pharynx) |
|
|
Functions & hormones of the respiratory membrane |
1. Two layers of simple squamous epithelium with shared basement membrane: Capillary endothelium & type I alveolar cells. 2. Allows rapid diffussion of respiratory gases between alveoli and blood |
|
|
What's included in the upper respiratory tract (URT)? |
Organs/structures superior to the trachea |
|
|
What's included in the lower respiratory tract (LRT)? |
Organs/structures inferior to larynx. |
|
|
What determines the pitch we make? |
The tautness of the true vocal fold cords |
|
|
What determines the loudness we make? |
The force of air flow through the true vocal folds |
|
|
What allows us to make sounds into speech? |
Throat Oral cavity |
|
|
What is the inner trachea and much of the respiratory tree lined with? |
Mucosa which forms the respiratory epithelium |
|
|
About how many alveoli are there per lung? |
150 million |
|
|
What do the lungs have that's important for recoiling during expiration? And fluid drainage? |
Elastic fibers Lymphatic drainage |
|
|
Right lung is shorter due to? Left lung is more narrow due to? |
Inferior liver Heart |
|
|
Function of Type I alveolar cell |
Surface for gas exchange |
|
|
Function of Type II alveolar cell |
Secrete surfactant to reduce surface tension |
|
|
Function of Alveolar macrophage |
Phagocytize particles and cellular debris |
|
|
Boyles law |
Volume of gas is inversely proportional to its pressure |
|
|
Intrapleural pressure is how much lower than the atmospherics and intrapulmonary pressure? |
~4 mmHg |
|
|
When is the intrapulmonary pressure equal to the atmospheric pressure? |
During pulmonary rest (not inhaling or exhaling) |
|
|
Pressure of intrapulmonary and intrapleural during inspiration |
Intrapulmonary- decreases Intrapleural- decreases |
|
|
Pressure of intrapulmonary and intrapleural during expiration |
Intrapulmonary- increases Intrapleural- increases |
|
|
5 Steps in inspiration |
1. Inspiratory muscles contact. 2. Thoracic volume increases. 3. Lung volume increases. 4. Intrapulmonary pressure decreases below atmospheric pressure. 5. Air flows into lungs. |
|
|
5 steps to expiration |
1. Inhibitory muscles relax. 2. Thoracic volume decreases due to elastic recoil. 3. Lung volume decreases. 4. Intrapulmonary pressure increases to above atmospheric pressure. 5. Air flows out of lungs. |
|
|
What happens to airway resistance and smooth muscles as diameter of airway increases? |
Airway resistance decreases and smooth muscles relaxes |
|
|
What happens to airway resistance & smooth muscles as diameter of airway decreases? |
Airway resistance increases and smooth muscles contacts |
|
|
How does surfactant reduce surface tension? |
It's is amphipathic meaning it has a hydrophilic and hydrophobic parts. This disrupts the hydrogen bonds of the water molecules so the alveoli remains inflated. |
|
|
What is pulmonary compliance and what determines it? |
Ability of the lungs and chest wall to stretch. Determined by: Alveolar surface tension Distension of elastic lung tissue Ability of chest wall to move |
|
|
Function of Dorsal Respiratory Group (DRG) nuclei |
Contains inspiratory center Establishes rhythmic potentials to stimulate inspiratory muscle contraction |
|
|
Function of ventral respiratory group (VRG) nuclei |
Contains expiratory center Inactive during quiet/resting breathing |
|
|
Function of cervical spinal nuclei |
Motor control over the diaphragm |
|
|
Function of phrenic nerve |

Carries nerve impulse from the cervical spinal nuclei to the diaphragm |
|
|
Function of the Thoracic spinal nuclei |
Motor control over the intercostal muscles |
|
|
Function of the intercostal nerves |
Carries nerve impulse from the thoracic spinal nuclei to the intercostal muscles |
|
|
Homeostasis: response to increase arterial PCO2 and/or H+ concentration by a negative feedback loop |
Receptor: central chemoreceptors detect increase
Control center: chemoreceptors relay information to DRG; which stimulates the VRG
Effector/response: VRG triggers hyperventilation and additional CO2 is lost
Homeostatic range: feedback decreases VRG simulation |
|
|
Homeostasis: response to decrease arterial PCO2 and/or H+ concentration by a negative feedback loop |
Receptor: central chemoreceptors retest decrease
Control center: chemoreceptors relay information to DRG; which stimulates the VRG
Effector/response: VRG triggers hypoventilation and additional CO2 is retained
Homeostatic range: feedback decreases VRG simulation |
|
|
How do peripheral chemoreceptors contribute to respiratory control? |
By providing input about oxygen levels via chemoreceptors in aortic and carotid bodies |
|
|
Description of a Sneeze |
Forceful expulsion of air through nose due to irritants in nasal cavity |
|
|
Description of cough |
Forceful expulsion of air against closed glottis due to irritants in the LRT |
|
|
What is partial pressure? |
The proportion of pressure in a gas mixture, accounted for by an individual gas |
|
|
Four significant gases |
N2 O2 CO2 water vapor |
|
|
List the PO2 gradient from highest to lowest concentration |
Atmosphere Alveoli Systemic supply Tissue ECF Cytoplasm |
|
|
List the PCO2 gradient from highest to lowest concentration |
Cytoplasm Tissue ECF Systemic return Alveoli Atmosphere |
|
|
What is pulmonary gas exchange driven by? |
Standard diffussion based on partial pressure of each individual gas and their pressure gradients |
|
|
How does the respiratory membrane surface area influence gas exchange? |
Affected directly by number of alveoli More alveoli = more surface area = more gas exchange |
|
|
How does the thickness of respiratory membrane influence gas exchange? |
Affected inversely by alveolar wall thickness; often affected by inflammation
Thicker = harder for gas exchange |
|
|
How does ventilation-perfusion matching influence gas exchange? |
Ventilation of alveoli and capillary blood flow (perfusion) must match |
|
|
Ventilation
Perfusion |
The amount of air flow to the alveoli
Amount of blood flow to the pulmonary capillaries |
|
|
A. Low PO2 in alveolus B. High PO2 in alveolus |
A. Pulmonary arterioles constricts. Less blood flow. B. Pulmonary arteriole dilates. More blood flow. |
|
|
A. Low PCO2 in arteriole. B. High PCO2 in arteriole. |
A. Bronchioles constrict B. Bronchioles dilate |
|
|
How does Pulmonary gas exchange occur? |
Movement of respiratory gases between alveoli and blood, across respiratory membrane |
|
|
How does tissue gas exchange occur? |
Movement of respiratory gases between the blood and respiring tissue, across the capillary endothelium |
|
|
How does Gas transport occur? |
Moment of oxygen and carbon dioxide between the alveoli and body tissues via the blood |
|
|
Is oxygen and carbon dioxide polar or non polar? |
Non-polar Doesn't dissolve well in H2O |
|
|
True or false Hemoglobin can reversible bind oxygen and carbon dioxide in a pH-dependent manner |
True |
|
|
True or false Hemoglobin can reversibly bind CO and oxygen. |
False CO competes for oxygen binding sites |
|
|
What is the abbreviation and characteristic of oxyhemoglobin |
HbO2
Saturated, with four oxygen molecules |
|
|
What is the abbreviation and characteristic of deoxyhemoglobin? |
HHb Not fully saturated with oxygen |
|
|
What is the abbreviation and characteristic of Carbaminohemoglobin? |
HbCO2 Bound with carbon dioxide (to peptide chain) |
|
|
Percentage of O2 bound to hemoglobin |
98.5% Oxyhemoglobin |
|
|
Percentage of O2 dissolved in plasma |
1.5% |
|
|
Percentage of CO2 as bicarbonate |
70% Affects plasma pH |
|
|
Percentage of CO2 bound to hemoglobin |
~20% |
|
|
Percentage of CO2 dissolved in plasma |
~10% |
|
|
4 steps to loading and unloading of hemoglobin in erythrocytes |
1. Loading. Oxygen from alveoli bonds to hemoglobin (Hb) in pulmonary capillaries, converting it to oxyhemoglobin (HbO2). H+ released. 2. Oxygen-rich blood travels to the heart, which pumps it to the systemic circulation 3. Unloading. Hb in the systemic capillaries releases oxygen to the tissue cells 4. Oxygen-poor blood returns to the heart, which pumps it back to the pulmonary circulation |
|
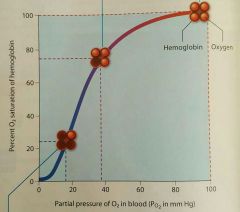
Distinguish the first 2 points in this oxygen-hemoglobin dissociation curve |
Lower point: vigorous exercise. Hb unloads most of its O2 in the tissue. Hb entering venous blood is ~25% saturated.
Middle point: resting. Hb unloads ~25% of its O2 to the tissues. Hb in systemic venous blood is ~75% saturated. |
|
|
How is the loading and unloading of oxygen affected by temperature change? |
Temperature increase causes more O2 unloading Temperature decrease cause less O2 unloading |
|
|
How is the loading and unloading of oxygen affected by H+ concentration? |
H+ concentration increase causes more O2 unloading |
|
|
How is the loading and unloading of oxygen affected by PCO2? |
Increased PCO2 causes more O2 unloading |
|
|
Write the balanced, catalyzed reversible equitation for the conversion of CO2 to bicarbonate |

|
|
|
5 steps in a bicarbonate formation at the respiring tissue (systemic capillary) |
1. CO2 diffuses from cells into erythrocyte. 2. Carbonic anhydrase catylizes CO2 & H2O and converts them to H2CO3 3. H2CO3 disassociate into HCO3- and H+ 4. H+ binds to Hb 5. HCO3- enters the plasma (as Cl enters erythrocyte) |
|
|
3 steps in CO2 formation at the alveoli (pulmonary capillary) |
1. H2CO3 is re-formed in the erythrocyte. 2. H2CO3 breaks down into H2O and CO2. 3. CO2 diffuses into the alveolus. |
|
|
Summarize respiratory physiology of the lungs |
1. O2 from inspired air in alveoli diffuses into blood, then erythrocytes 2. O2 binds to deoxyhemoglobin in erythrocyte. 3. Oxyhemoglobin releases H+ 4. O2 is transported through systemic blood to tissue cells |
|
|
Summarize the steps of respiratory physiology of the tissues |
1. CO2 diffuses from tissue cells into blood, then erythrocytes 2. CO2 + H2O =H2CO3, catalyzed by carbonic anhydrase 3. H2CO3 = H+ + HCO3- 4. HCO3- diffuses into plasma, Cl diffuses into erythrocyte 5. Some CO2 binds to hemoglobin (carbaminohemoglobin) 6. H+ causes slight reduction in cytoplasmic pH of RBCs 7. Reduced pH in erythrocytes reduces hemoglobin's affinity for O2. 8. O2 is released and diffuses into tissue cells. 9. H+ binds to deoxyhemoglobin |
|
|
Summarize respiratory physiology of the lungs when CO2 is released |
1. Release of H+ from oxyhemoglobin causes HCO3- to enter erythrocytes; Cl- diffuses into plasma 2. H+ + HCO3- = H2CO3 3. H2CO3 = CO2 + H2O, catalyzed by carbonic anhydrase 4. Higher PCO2 in blood causes diffussion of CO2 into alveoli expiration |
|
|
Effects of age to the respiratory system |
1. Respiratory epithelium thins especially with exposure to pollutants 2. Fibrous tissue accumulate 3. Loss in elasticity 4. Retain more stale air 5. Reduces O2 availability and increases CO2 retention 6. Alveolar surface area decreases
|
|
|
H+ in erythrocyte causes slight reduction in... |
Cytoplasmic pH in RBCs |
|
|
Reduced pH in erythrocytes reduces... |
hemoglobin's affinity for O2 |
|
|
Name the 5 oxygen imbalances |
Hypoxia Anemic hypoxia Hypoxemic hypoxia Ischemic hypoxia Cyanosis |
|
|
Causes & characteristics/symptoms of hypoxia |
Oxygen deficiency in a tissue Inability to use oxygen |
|
|
Causes & characteristics/symptoms of Hypoxemic hypoxia |
State of low arteriole PO2 due to inadequate pulmonary gas exchange Causes: high elevation, downing, respiratory arrest |
|
|
Causes & characteristics/symptoms of ischemic hypoxia |
Inadequate blood circulation Causes: congestive heart failure, infarction, stroke |
|
|
Causes & characteristics/symptoms of anemic hypoxia |
Blood's inability to carry adequate oxygen Cause: anemia |
|
|
Causes & characteristics/symptoms cyanosis |
Blueness of the skin Sign of hypoxia; most noticeable in nail beds and lips |
|
|
Causes & characteristics/symptoms of pneumothorax |
Presence of air in the pleural cavity, often from a penetrating chest wound. Loss of negative pressure causes lung collapse. |
|
|
Causes & characteristics/symptoms of acute rhinitis |
Common cold, caused by several respiratory viruses. Symptoms: Congestion, sneezing, runny nose, and dry cough |
|
|
Causes & characteristics/symptoms of pharyngitis |
Sore throat, most commonly formed by viral infection Streptococcal pharyngitis (strep throat) is less common, but more of a concern |
|
|
Causes & characteristics/symptoms of pneumonia |
Lower respiratory tract infection, typically bacterial or viral. Causes accumulation of fluid in alveoli and thickening of respiratory membrane |
|
|
Causes & characteristics/symptoms of tuberculosis |
Caused by infection with Mycobacterium tuberculosis After phagocytosis by macrophage, lungs form fibrous nodules to isolate bacteria |
|
|
Causes & characteristics/symptoms of asthma |
Most commonly triggered by allergens Inflammation results in bronchospasms and increased mucus production |
|
|
Causes & characteristics/symptoms of cystic fibrosis |
1. Mutation results in lack of chloride ion transport proteins 2. Mucus in respiratory tract becomes dehydrated and sticky 3. Respiratory passages becomes clogged with mucus 4. Clogs secretory ducts of the pancreas (digestive)
|
|
|
Causes & characteristics/symptoms of emphysema |
1. Chronic infections lead to breakdown in alveolar structure 2. Results in decreased respiratory membrane for gas exchange 3. Lungs become fibrotic and lose their elasticity (reduced compliance) |
|
|
Causes & characteristics/symptoms of lung cancer |
1. Most commonly caused by tobacco smoke (fist and second hand) 2. Tumors invade bronchial wall and compress airways 3. Metastasis is rapid, with diagnosis typically occurring after metastasis begins |
|
|
Causes & characteristics/symptoms of chronic obstructive pulmonary disease (COPD) |
1. Chronic obstruction of airways reduces pulmonary ventilation 2. Associated with chronic bronchitis and emphysema 3. Results in hypoxia and respiratory acidosis |
|
|
Causes & characteristics/symptoms of pulmonary embolism |
Thrombosis in systemic veins (DVT in legs) results in embolism in the lungs. Blockage of blood flow to lungs reduces oxygen exchange, causing hypoxia. |
|
|
Causes & characteristics/symptoms of pulmonary edema |
1. Occurs when right ventricle output exceeds left ventricle output. 2. Back-pressure into pulmonary circulation causes fluid accumulation in lungs. 3. Often occurs with congestive heart failure on the left side |
|
|
Function of the blood |
Transport gases, nutrients, wastes & hormones |
|
|
Function of the heart |
Pumps blood through body |
|
|
Function of the arteries |
Carries blood from heart to body tissues |
|
|
Function of the veins |
Carries blood from body tissues to the heart |
|
|
Function of the capillaries |
Location of exchange between blood and body tissues |
|
|
Function of the hypothalamus |
Overall control of homeostasis Simulates pituitary hormone secretion |
|
|
Function of the pituitary gland |
Simulates hormone secretion from other endocrine glands
Control of growth |
|
|
Function of the thyroid gland |
Metabolic control Calcium homeostasis |
|
|
Function of the parathyroid gland |
Calcium homeostasis |
|
|
Function of the adrenal gland |
Fight or flight response Metabolic control Blood pressure control |
|
|
Function of the pancreas |
Blood glucose homeostasis |
|
|
Functions of the integumentary system |
1. Protects body from dehydration, microbial invasion, and abrasion 2. Synthesizes vitamin D 3. Tactile receptors (cutaneous senses)... touch, pain, pressure, temp 4. Thermoregulates via sweating and vascular changes 5. Excretes metabolic waste and excess electrolytes (when sweating) 6. Reservoir for blood (due to high number of dermal vessels) |
|
|
Functions of the skeletal system |
1. Provides support and protection for various organs 2. Provides leverage for movement 3. Stores minerals and lipids 4. Produces blood cells |
|
|
Functions of the muscular system |
1. Provides force for movement 2. Maintains posture and body position 3. Stabilizes joints 4. Supports soft tissues 5. Produces heat for thermoregulation |
|
|
Functions of the nervous system |
1. Coordinates body functions -sensory input -integration -motor output 2. Control is fast-acting but short-lived |
|
|
Functions of the endocrine system |
Coordinates body function, most commonly to maintain homeostasis Control of slow-acting but long-lasting via hormones Effects are often systemic |
|
|
Function of the cardiovascular system |
Transports nutrients, wastes, hormones, and respiratory gases Maintains Balance and composition of interstitial fluids via capillary exchange |

