![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
117 Cards in this Set
- Front
- Back
|
1. You are called to see a 30 year old man with rapidly deteriorating asthma. Following appropriate medical management an endotracheal tube is inserted and he is ventilated with a mechanical ventilator with a tidal volume of 600ml and a rate of 12 breaths per minute. Five minutes later the blood pressure is unrecordable and external cardiac massage is commenced. Arterial blood is taked and shows ph 7.08, pCO2 96 mmHg, pO2 36 mmHg, SpO2 46% and bicarbonate 27 mmol/L. He is administered adrenaline, salbutamol, pancuronium, bicarbonate and calcium gluconate. The ECG shows sinus rhythm at a rate of 60 beats per minute. The patient remains pulseless and cyanosed with fixed dilated pupils and distended neck veins. The most appropriate management is to |
D. "If profound hypotension does occur when assisted ventilation has been initiated, consideration should be given to disconnecting the patient from the circuit (possibly with the addition of pressure on the chest wall to assist expiratory flow) to allow full passive expiration". CEACCP 2008. Management of life threatening asthma in adults.
|
|
|
2. A patient known to have porphyria is inadvertently administered thiopentone on induction of anaesthesia. In recovery the patient complains of abdominal pain prior to having a seizure and losing consciousness. Which drug should NOT be given
A. Pethidine B. Diazepam C. Haematin D. Suxamethonium E. Pregabalin |
A- decreases seizure threshold
Pethidine probably safe in porphyria, but should be avoided in seizures/epilepsy - lowers seizure threshold |
|
|
3. A 42 year old lady presents for right pneumonectomy with a left sided double-lumen tube. She is 132kg and 160cm. What depth, measured at the incisors, is likely to give the ideal position?
A. 24cm B. 26cm C. 28cm D. 30cm E. 32cm |
C - 28cm
Formula is 29 cm +/- 1 cm depth for every +/-10 cm change in height from 170cm OHCA p372 |
|
|
4. What is the most effective method of minimizing acute kidney injury following an elective open abdominal aortic aneurysm repair?
A. give IV crystalloid as a ‘preload’ before cross-clamp B. give IV mannitol before cross-clamp C. give IV frusemide before cross-clamp D. give preoperative N-acetylcysteine E. minimize aortic cross-clamp time |
E
|
|
|
5. [New] Features of severe pre-eclampsia include:
A. Foetal growth retardation B. Peripheral oedema C. Systolic BP more than 160 D. Thrombocytopenia E. Severe proteinuria |
C
|
|
|
6. [Repeat] Earliest sign of a high block in a neonate post awake caudal:
A. Increased HR B. Increased BP C. Reduced HR D. Desaturation E. Loss of consciousness |
D. Desaturation (due to blockade of intercostal mm.)
"Vagally mediated parasympathetic tone predominates" (OHA p.801) Little vasodilation and hypotension from sympathetic blockade. Won't get same degree of bradycardic response from high block as adults |
|
|
7. A 20 year old man was punched in the throat 3 hours ago at a party. He is now complaining of severe pain, difficulty swallowing, has a hoarse voice and had has some haemoptysis. What is your next step in his management? |
D
|
|
|
8. A 60 year old man with normal LV function is having coronary artery bypass grafting. After separation from the bypass machine he becomes hypotensive with ST elevation in leads II and aVF. The Swan Ganz Catheter showed a PCWP of 25 and CVP of 15 with normal PVR and SVR. The TOE is likely to show: |
B |
|
|
11. You are working in a theatre with a line isolation monitor, which is working. You touch a wire. What is going to happen? |
B incomplete Q, but if you touch a live wire and the LIM is working, there should be no earthing to ground through you, as the two circuits should be equipotent (ie no difference in energy therefore no current/electron flow generated)
http://www.anaesthesia.med.usyd.edu.au/resources/lectures/electricity.html |
|
|
12. What is the test is decreased in Iron deficiency anaemia?
A. microcytosis B. serum ferritin C. serum iron D. transferrin E. total iron binding capacity |
B serum ferritin
Serum Iron is also low but is low in Anaemia Chronic Disease too, whereas ferritin is more specific for Fe Deficiency. in Fe deficiency anaemia transferrin/Total Iron Binding Capacity is increased, as total body stores of iron are low and the carrier molecule (transferrin) is being underutilised. Therefore Transferrin SATURATION will be low also. |
|
|
3. A full size C oxygen cyclinder (size A in New Zealand) has pressure regulated from
A. 16000kpa to 400kpa B. 16000kpa to 240kpa C. 11000kpa to 400kpa D. 11000kpa to 240kpa E. 7600kpa to 240kpa |
A
BOC website |
|
|
14. MRI Telsa 3, least likely to cause harm
A. Cochlear implant B. mechanical heart valve C. Implanted intrathecal pump D. Recently placed aortic stent E. shrapnel fragment |
B, not D as recently placed so not endotheliolised
|
|
|
15-What happens when you place a magnet over a biventricular internal cardiac defibrillator
A. Switch to asynchronous pacing B. Damage the internal programming C. Nothing D. Switch off antitachycardia function E. Switch of rate responsiveness |
D, but retains PPM functions.
depends on the device |
|
|
16-You are performing an awake fibreoptic intubation, through the nose, on an adult patient. In order, the fibrescope will encounter structures with sensory innervation from the following nerves
A. facial, trigeminal, glossopharyngeal B. facial, trigeminal, vagus C. glossopharyngeal, trigeminal, vagus D. trigeminal, glossopharyngeal, vagus E. trigeminal, vagus, glossopharyngeal |
D
|
|
|
19 Electrocardiogram in the Cs5 configuration. What are you looking at when monitoring lead I.
A. anterior ischaemia B. atrial C. inferior D. lateral E. septal |
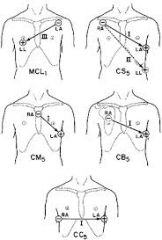
A - anterior ischaemia
Central subclavicular (CS5) lead particularly well suited for detection anterior myocardial wall ischemia. - right arm (RA) electrode under right clavicle, left arm (LA) electrode in V5 position, and left leg electrode usual position to serve as a ground. - Lead I: detection of anterior wall ischemia - Lead II: monitoring inferior wall ischemia or for the detection of arrhythmias. - If a unipolar precordial electrode is unavailable, this CS5 bipolar lead is the best and easiest alternative to a true V5 lead for monitoring myocardial ischemia. http://web.squ.edu.om/med-Lib/MED_CD/E_CDs/anesthesia/site/content/v03/030340r00.htm |
|
|
20 Lowest extension of thoracic paravertebral space
A. t10 B. t12 C. l2 D. l4 E. s1 |
B
The thoracic paravertebral space begins at T1 and extends caudally to terminate at T12. CEACCP 2010. Paravertebral block. |
|
|
21 20 yr old male presents to ED with 30% burns from a fire. His approx weight is 80kg. Based on the Parkland formula, how much fluid is required in the first 8hrs from time of injury?
A. 2.4L N/S B. 3.6L N/S C. 3.6L Hartmann's D. 4.8L N/S E. 4.8L CSL |
E
Parkland Formula 4 mL/kg x BSA burned 1/2 in first 8/24, remainder in next 16/24 |
|
|
22 In regards to systemic sclerosis, what is the least likely cardiac manifestation?
A. accelerated coronary artery disease B. atrioventricular conduction block C. myocarditis D. pericardial effusion E. valvular regurgitation |
E Valvular
Although accelerated coronary artery disease is NOT a feature (vasospastic lesions occur), myocardial infarction is a greater risk than in the general population. (UTD) |
|
|
23 (repeat) The reason that desflurane requires a heated vapour chamber can be best explained by its:
A. Low saturated vapour pressure b) High saturated vapour pressure c) High boiling point B. ? C. ? D. Low molecular weight E. Very low solubility |
B
|
|
|
24 (New but on a repeated theme)A 30 year old lady has a vaginal forceps delivery without neuroaxial blockade. The next day she is noted to have loss of sensation over the anteriolateral aspect of her left thigh. There are NO motor symptoms. The is best explained by damage to the left sided:
A. Lumbosacral trunk B. Lateral cutaneous nerve of the thigh C. Pudendal nerve D. L2/3 Nerve root E. Sciatic nerve |
B
|
|
|
25.->AZ84 When performing laryngoscopy using a Macintosh blade, your best view is of the patient's epiglottis touching the posterior pharyngeal wall. Using the Cormack and Lehane scale this is grade
A. 1 B. 2 C. 3a D. 3b E. 4 |
D
|
|
|
26. A healthy 20 year old patient undergoing nasal surgery under general anaesthesia has the nose packed with gauze soaked in 0.5% phenylephrine and a submucosal injection of lignocaine with 1:100,000 adrenaline. Over the next 10 minutes the blood pressure rises from 130/80 to 220/120 mmHg and the heart rate from 60 to 100 beats per minute. The LEAST appropriate management of this situation would be to
A. administer glyceryl trinitrate B. administer esmolol C. administer labetalol D. administer sodium nitroprusside E. deepen anaesthesia with isoflurane |
C
Avoid B blockers (plus labetolol longer lasting than esmolol) See black bank (search AC108) |
|
|
27. An 8 year old 30kg girl presents for resection of a Wilms tumour. Her starting haematocrit is 35% and you decide that your trigger for transfusion will be 25%. The amount of blood that she will need to lose prior to transfusion is
A. 400mL B. 500mL C. 600mL D. 700mL E. 800mL |
C
Answer: 600 ml MABL = Maximum Allowable Blood Loss MABL = EBV x (Starting hematocrit - Target Hematocrit)/Starting hematocrit = 30kg x 70mL/kg x (35-25)/35 = 600mL |
|
|
28. An adult male preoperatively complains of pain similar to his angina. Initial treatment is all below except:
A. Aspirin B. heparin C. morphine D. nitrates E. oxygen |
B
|
|
|
29. What cannot be used for tocolysis in a 34/40 pregnant woman:
A. Clonidine B. Indomethacin C. Magnesium D. Salbutamol E. Nifedipine |
A. Clonidine - ?no tocolytic effect.
B. Indomethacin: is a tocolytic, but can cause premature PDA closure after 34/40. |
|
|
30. Pringles procedure for life threatening liver haemorrhage includes clamping of:
A. Hepatic artery B. Hepatic vein C. Portal pedicle D. Aorta E. Splenic Artery |
C Hepatoduodenal ligament clamping. max time 20 mins
|
|
|
31. Your patient has smoked cannabis prior to arrival in the OT. Pt taking cannabis might lead to:
A. Intraoperative Bradycardia B. Decreased anaesthetic requirement C. Increased nausea and vomiting D. Increased risk of awareness E. Decreased BIS reliability |
B if acutely intoxicated
Stoelting A&CED. |
|
|
32. MVA trauma patient arrives in ED BP100/60 HR 100 with the following CXR (‘’I thought it looked like an aortic dissection/rupture with a widened mediastinum’’). The most appropriate next investigation would be:
A. Aortography B. CT Chest C. MRI D. TOE E. TTE |
D
|
|
|
33. A 70 year old man with slow atrial fibrillation is reviewed for insertion of a permanent pacemaker. He is otherwise well. He is on warfarin with an INR of 2.2. Prior to PPM insertion do you
A. Cease warfarin and commence dabigatran B. Cease warfarin and commence Enoxaparin C. Cease warfarin and recommence post procedure D. cease warfarin and commence heparin E. Continue warfarin |
E. BRUISE trial, NEJM, 2013
|
|
|
34. A 40 year old man with Marfan's has undergone a thoracoabdominal aneurysm repair. 48 hours post procedure there is blood noted in his CSF drain and he is obtunded. Your next course of action is:
A. Coagulation studies B. CSF microscopy and culture C. CT Head D. MRI Head E. MRI Spine |
C ? subdural
Complications of spinal fluid drainage in thoracoabdominal aortic aneurysm repair: a report of 486 patients treated from 1987 to 2008. J Vasc Surg 2009, 49(1), 29-34. |
|
|
36. You are anaesthetising a fit 50 year old woman for an elective laparoscopic cholecystectomy. In her pre operative assessment she has a normal cardiovascular exam and her BP is 115/75. You induce anaesthesia with 100mcg fentanyl, 100mg propofol and 50 mg rocuronium. Soon after induction her ECG looks like this (showed narrow complex tachycardia around 180-200/min – ie SVT). Her BP is now 95/50. What is the most appropriate management?
A. adenosine B. amiodarone C. DC cardioversion D. GTN E. metaraminol |
A
|
|
|
37. The electrical requirement that distinguishes a "cardiac protected area" from a "body protected area" is the
A. isolation transformer B. line isolation monitor C. equipment has a maximum leakage current of 500 microamperes D. residual current device E. equipotentiality |
E
http://www.rch.org.au/bme_rch/electrical_safety/#body |
|
|
38. After ingestion of 500mg/kg aspirin, the most efficient therapy to enhance the elimination is
A. normal saline infusion B. bicarbonate infusion C. mannitol D. frusemide E. haemodialysis |
E
|
|
|
39. Most cephalic interspace in neonate to perform spinal while minimising the possibility of spinal cord puncture
A. L1-L2 B. L2-L3 C. L3-L4 D. L4-L5 E. L5-S1 |
C. L3/4
NYSORA. Spinal Anesthesia in Children. Conus medullaris ends approx L1 in adults and L2 or L3 in neonates and infants. In order to avoid potential injury to SC, dural puncture should be performed below level of SC, i.e. below L2-L3 in neonates and infants. (from this - assume L3/4 is highest interspace can be sited with minimal risk) |
|
|
40. 6 week old baby is booked for elective right inguinal hernia repair. An appropriate fasting time is
A. 2 hours for breast milk B. 4 hours for formula C. 5 hours for breast milk or formula D. 6 hours for solids E. 8 hours for solids, 4 hours for all fluids. |
B
Poor question as ANZCA guideline changeover age is 6/52. RCH guidelines are different to ANZCA guidelines (shown below) Best choice- B For healthy adults having an elective procedure, limited solid food may be taken up to six hours prior to anaesthesia and clear fluids totalling not more than 200 mls per hour may be taken up to two hours prior to anaesthesia. For healthy children over six weeks of age having an elective procedure, limited solid food and formula milk may be given up to six hours, breast milk may be given up to four hours and clear fluids up to two hours prior to anaesthesia. For healthy infants under six weeks of age having an elective procedure, formula or breast milk may be given up to four hours and clear fluids up to two hours prior to anaesthesia. Only medications with a little water if required as ordered by the anaesthetist should be taken less than two hours prior to anaesthesia. |
|
|
41. For a nurse monitoring an opioid PCA, the earliest sign of respiratory depression is;
A. Number of boluses of PCA per hour B. Respiratory rate C. Oxygen saturation D. Sedation score E. Pupil size |
D
Acute pain management text ANZCA (3rd ed.) "Resp depression.. best early clinical indicator is increasing sedation" p.65 (pg 111 on PDF) |
|
|
42. A reduction in DLCO can be caused by;
A. Asthma B. COPD C. Left to right shunt D. Pulmonary haemorrhage E. Bronchitis |
B COPD
Nunn's p.153: Factors affecting diffusing capacity 3 major mechs: - changes in effective surface area of gas XC mem (e.g. emphysema - destruction alveolar septa) - changes in physical properties of the mem - changes related to uptake of gas at RBC |
|
|
43. You place a thoracic epidural for a patient having an elective open AAA repair. There are 4cm in the epidural space and you aspirate blood. What is the most appropriate management plan:
A. inject 5 mL of saline, and if you can no longer aspirate blood, leave in place and use B. inject 5 mL lignocaine 2% with adrenaline. If there is no rise in HR be happy that it is not intravascular and secure in place and use C. Remove and postpone surgery for 24 hours D. Remove and place epidural 1 level higher E. Remove and postpone surgery for 4 hours |
C
|
|
|
44. You are anaethetising a lady for elective laparoscopic cholecystectomy, who apparently had an anaphylactic reaction to rocuronium in her last anaesthetic. There has not been sufficient time for her to undergo cross-reactivity testing. What would be the most appropriate drug to use:
A. rocuronium B. suxamethonium C. pancuronium D. atracurium E. cisatracurium |
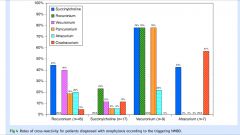
E
anaphylaxis to neuromuscular blocking drugs bja 2013 "Cisatracurium had the lowest rate of cross-reactivity in patients who had previously suffered anaphylaxis to rocuronium or vecuronium" |
|
|
45 Patient with subdural haematoma, on warfarin. INR 4.5. Needs urgent craniotomy. Vit K given already by ED resident. What further do you give for urgent reversal of this patient's INR?
A. Factor VII B. Cryoprecipitate C. FFP D. Prothrombinex E. FFP + prothrombinex |
E
warfarin reversal guidelines. MJA 2013. |
|
|
46 Regarding endotracheal tubes used in laser surgery:
A. They are more resistant to combustion when the cuff is covered in blood B. Resistant to ignition from electrocautery C. The cuff is resistant to ignition if hit by the laser D. Have an external diameter which is larger than a normal PVC endotracheal tube (compared to the internal diamater) E. Have 2 cuffs which are resistant to combustion |
D
CEACCP. Lasers and surgery 2003. |
|
|
49 Elderly lady post operatively with painful eye. Differential between narrow angle glaucoma and corneal abrasion
A. ? B. C. D. E. Relieved by topical local anaesthetic |
E- will be relieved by topical anaesth if Corneal abrasion.
|
|
|
50 During an elective thyroidectomy a patient develops symptoms consistent with the diagnosis of “thyroid storm” which of the following treatment options in NOT appropriate
A. Carbimazole B. Beta-blocker C. Propythiouracil D. Plasmaphoresis E. Hydrocortisone |
D- least practical
all options described in Rx thyroid storm |
|
|
53 Two days post upper spinal surgery, patient notices parathesia of the right arm, surgeon thinks this is an ulnar nerve palsy due to poor positioning. What sign will distinguish a C8-T1 nerve root lesion from an ulnar nerve neuropathy?
A. parasthesia in little finger B. parasthesia in the distribution of the interscalene nerve C. weakness in adductor digiti minimi D. weakness in abductor pollicis brevis E. weakness in lateral interosseus |
D
A- no, ulnar nerve territory B- no such nerve (that I can find!) C- if they meant ABDUCTOR digiti minimus then no, as supplied by ulnar, as are all intrinsic muscles of the hand except lateral two lumbricals & the three muscles of the thenar eminence (abductor pollicis brevis, flexor pollicis brevis, opponens brevis; median nerve innervates these) D. YES If abductor pollicis brevis weak, then must be C8/T1 lesion, as this muscle supplied by MEDIAN nerve but shares the nerve root origin of C8/T1 with the ulnar nerve. |
|
|
54 A 54 year old man, is on warfarin for atrial fibrillation, has a history of alcohol abuse and liver failure with an albumin of 30 and a bilirubin of 28. What is his CHADS 2 score?
A. 0 B. 1 C. 2 D. 3 E. 4 |
A 0
CCF/Hypertension/Age >75/ Diabetes/ Stroke,TIA, TED previously (this scores 2) |
|
|
57 You are 2 hours into an operation. 3L of IV Crystalloid has been given. There has been minimal blood loss. The dilutional anaemia is compensated by:
A. Cellular anaerobic metabolism B: Capillary vasodilation C: Increased cardiac output D: Increased tissue oxygen extraction E: Rightwards shift of the Oxygen – Haemoglobin dissociation curve |
c
Blood Transfus. Oct 2009; 7(4): 250–258 Clinical evidence of blood transfusion effectiveness |
|
|
58 You are putting in an Internal Jugular CVC. Which manoeuvre will cause maximum venous distension of the jugular vein?
A. Continuous Positive Airway Pressure (No value given) B: Breath hold at end-expiration C: Manual compression at the base of the neck D: Trendelenburg position E: Patient performs a valsalva |
E
Eur J Radiol. 2006 May;58(2):307-9. Epub 2005 Dec 13 Valsalva and gravitational variability of the internal jugular vein and common femoral vein: ultrasound assessment |
|
|
59. What is approximately the systolic blood pressure in an awake neonate (mmHg)
A. 55 B. 70 C. 85 D. 100 E. 115 |
B 70
http://www.health.vic.gov.au/neonatalhandbook/procedures/blood-pressure.htm |
|
|
60. The volatile agent most likely to be associated with carbon monoxide production when used with a soda lime scrubber is:
A. Desflurane B. Isoflurane C. Sevoflurane D. Halothane E. Enflurane |
A desflurane
Stoelting Ch 2 Carbon monoxide toxicity Des > Enfl > Isofl |
|
|
65. A new antiemetic decreases the incidence of PONV by 33% compared with conventional treatment. 8% who receive the new treatment still experience PONV. The no of patients who must receive the new treatment instead of the conventional before 1 extra patient will benefit is
A. 3 B. 4 C. 8 D. 25 E. 33 |
D- 25
This question is asking about Number Needed to Treat NNT= 1/ARR (absolute risk reduction) ARR= CER- EER, expressed as fraction of 1 CER= Control Event Rate EER= Experimental Event Rate In this example, a 33% reduction in relative risk leaves 8% still with PONV, so conventional (Control) treatment 12% Event rate New (experimental) treatment 8% Event rate ARR= 4% So NNT = 1/0.04 = 25 |
|
|
66. According to guidelines endorsed by ANZCA, the label of an intra-osseous infusion should be
A. beige B. blue C. Pink D. Red E. yellow |
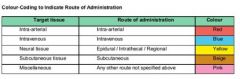
C pink
|
|
|
69. During apnoeic oxygenation under light anaesthesia, the expected rise in PaO2 would be:
A. 0.5 mmHg per min B. 1 mmHg per min C. 2 mmHg per min D. 3 mmHg per min E. 5 mmHg per min |
If Q was rise in PaCO2,
D 3 mmHg per min |
|
|
70. In the Revised Trauma Score, the initial assessment parameters include Glascow Coma Scale, Blood Pressure, and :
A. Heart Rate B. Saturation C. Respiratory Rate D. Urine Output E. Temperature |
C RR
|
|
|
72. Absolute Contraindication to ECT
A. Cochlear implants B. Epilepsy C. Pregnancy D. Raised intracranial pressure E. Myocardial infarction |
D
|
|
|
73. 80 year old female for open reduction and internal fixation of a fractured neck of femur. Fit and well. You notice a systolic murmur on examination. Blood pressure normal. On transthoracic echo, she has a calcified aortic valve, with aortic stenosis with a mean gradient of 40mmHg. How do you manage her:
A. Instigate low dose beta blockade B. Defer, and refer to a cardiologist C. Perform a transoesophageal echo to get a better look at the valve D. Proceed to surgery with no further investigation E. Perform a dobutamine stress echo |
D emergency surgery and doesn't need intervention anyway.
|
|
|
75 A 25 y.o. male has a traumatic brain injury on a construction site. GCS 7. Intubated on site and transported 1 hour to hospital. Haemodynamically stable and no other injuries. Most appropriate pre hospital fluid:
A. 4% albumin B. Dextran 70 in 0.9%N/saline C. 6% hydroxyethyl starch D. Ringers lactate E. 0.9% N/saline |
E N Saline
|
|
|
76 A 40 y.o. female newly diagnosed ITP. Retinal detachment for surgery in 2 days. Platelets 40 and blood group A+. Management of her ITP:
A. Administer Anti-D antibodies 6 hrs pre op B. Admister desmopressin one hour pre op C. Administer methylpred and IVIg 2 days pre op D. Recheck platelet count morning of surgery and if not dropped continue E. Platelet transfusion morning of surgery |
C.
http://bestpractice.bmj.com/best-practice/monograph/138/treatment/step-by-step.html Acc to UTD- For management of life-threatening bleeding, treatment options include: ■Platelet transfusions ■IVIG (1 g/kg, repeated the following day if the platelet count remains <50,000/microL) ■Pulse methylprednisolone (1 g intravenously, repeated daily for three doses) ■Recombinant human factor VIIa no mention of desmopressin, and no mention of Anti-D for use in the acute phase. |
|
|
77. (Rpt) A neonate will desaturate faster than an adult at induction because
A. FRC decreased more B. Faster onset of induction agents C. More difficult to pre-oxygenate D. E. |
A |
|
|
78. (Rpt Jul 07) Isoflurane is administered in a hyperbaric chamber at 3 atmospheres absolute pressure using a variable bypass vaporizer. At a given dial setting and constant fresh gas flow, vapour will be produced at:
A. the indicated vapour concentration B. three times the indicated vapour concentration C. one third the partial pressure obtained at 1 atmosphere D. the same partial pressure as is obtained at 1 atmosphere E. three times the partial pressure obtained at 1 atmosphere |
D.
Anaesthetic science viva book (p.284) Altitude: Imagine that the atmospheric pressure halves to 380mmHg. A vaporiser calibrated to deliver 1% at sea level will therefore deliver 2% (760/380). One per cent at sea level represents a partial pressure of 7.6mm (0.1/760), which is the same as 2% at altitude (0.2/380). Although the output of vapour in volumes percent increases, the partial pressure remains unchanged. As it is the partial pressure of the agent that is responsible for anaesthesia the vaporiser can therefore be used as normal either at altitude or under hyperbaric conditions. Also - CEACCP article (but not for desflurane..) |
|
|
79. [AP CXR and lateral] – ‘’showed hydropneumothorax’’ This grossly abnormal CXR is
A. right basal pneumothorax B. right hydropneumothorax C. artifact D. right pleural effusion E. right R lower lobe atelectases |
Assuming:
B |
|
|
80. 37 female presents to ED with headache and confusion. She is otherwise neurological normal and haemodynamically stable. Urine catheter and bloods takes. UO > 400ml/hr for 2 consecutive hours, Serum Na 123 mmol/l, Serum Osmolality 268, Urine Osmolality 85 The most likely diagnosis is
A. Central diabetes insipidus B. Nephrogenic diabetes insipidus C. Psychogenic polydipsia D. Cerebral salt wasting E. SIADH |
C
■A low plasma sodium concentration (less than 137 meq/L) with a low urine osmolality (eg, less than one-half the plasma osmolality) is usually indicative of water overload due to primary polydipsia. ■A high-normal plasma sodium concentration (greater than 142 meq/L, due to water loss) points toward DI, particularly if the urine osmolality is less than the plasma osmolality [1]. ■A normal plasma sodium concentration is not helpful in diagnosis but, if associated with a urine osmolality more than 600 mosmol/kg, excludes a diagnosis of DI. -from UTD |
|
|
83 A 45 year old obese man complains of headache, lower limb weakness and polyuria. On examination, his blood pressure is 150/70mmHg. He has a displaced apex beat. Bloods revealed Na145, K2.8, Cl101, HCO3 27. What is the most likely diagnosis
A. Cushings B. Diabetes C. Primary hyperaldosteronism D. Hypothyroidism E. Phaeochromocytoma |
C Hyperaldosteronism:
Primary usually from adenoma causes- salt retention, hypervolaemia (therefore hypertension), causing mildly increased serum Na (145-147) Potassium wasting from cortical collecting tubule, which causes muscle weakness (usually not til K <2.5) Hydrogen ion excretion from distal tubule Mild Mg wasting |
|
|
84 Which of the following is the best predictor of a difficult intubation in a morbidly obese patient
A. Pretracheal tissue volume B. Mallampati score C. Thyromental distance D. BMI E. Severity of OSA |
A
an abundance of pretracheal soft tissue at the level of vocal cords is a good predictor of difficult laryngoscopy in obese patients.. Prediction of Difficult Laryngoscopy in Obese Patients by Ultrasound Quantification of Anterior Neck Soft Tissue. Anaesthesia 2003 Nov |
|
|
85. You wish to compare a new method of BP measurement with the gold standard. The best way to do this is:
A. CUSUM analysis B. Friedman's test C. ? D. Pearson’s correlation E. Bland-Altman plot |
E- repeat
Bland and Altman plots are extensively used to evaluate the agreement among two different instruments or two measurements techniques. Bland and Altman plots allow us to investigate the existence of any systematic difference between the measurements (i.e., fixed bias) and to identify possible outliers. The mean difference is the estimated bias, and the SD of the differences measures the random fluctuations around this mean. |
|
|
86. After intubating for an elective case you connect up the circuit and notice that you are unable to ventilate and observe high airway pressures. The next most appropriate step is to:
A. Auscultate the lungs B. Release the APL valve C. Remove the endotracheal tube and bag mask ventilate D. Turn on the ventilator E. Low positive end expiratory pressure |
A
|
|
|
87. You insert a thoracic epidural in a patient for a liver resection with an upper abdominal incision. You have recently topped it up. On waking the patient appears weak, despite adequate reversal. He can breathe spontaneously and can flex his biceps but is not able to extend triceps. The level of the block is most likely to be:
A. C5 B. C6 C. C7 D. C8 E. T1 |
C
Myotomes. Last's anatomy. 5-6 shoulder movt 5-6 elbow flexion 7-8 elbow extension 6-7 wrist flexion/extension 8-T1 finger movt see myotome dance :) http://www.youtube.com/watch?v=NHaZMFpKOMA |
|
|
88. (repeat) You are anaesthetizing a pregnant woman for neuro-radiological coiling. At what gestation is it important to monitor uteroplacental sufficiency?
A. 22 weeks B. 24 weeks C. 26 weeks D. 28 weeks E. 32 weeks |
B
CEACCP 2012. Anaesthesia for non-obstetric procedures during pregnancy |
|
|
89 During the neurosurgical management of a cerebral aneurysm. The drug to administer to facilitate permanent clip placement is?
A. Nimodipine B. Adenosine C. Mannitol D. Hypertonic Saline E. Thiopentone |
B
Adenosine in cerebral aneurysm clipping Current Anesthisiol Rep 2013 Recently, adenosine induced transient circulatory arrest has undergone a resurgence in neurosurgical practice to assist in complex aneurysm clip ligation. |
|
|
90. Prior to seeking consent from family/relatives for DCD, it is important to confirm which of the following?
A. Not a coroners case B. Pt will have a cardiac death within 90 minutes in the absence of life-support C. Potential organ recipient's identified and are available D. Patient's wishes have been considered E. Decision confirmed by an external committee |
D
|
|
|
91. You see a young man prior to surgery. He describes a history of throat swelling and difficulty breathing both spontaneously and in association with minor dental procedures. His brother has had similar episodes. The most likely mechanism is:
A. C1-esterase deficiency B. Factor V deficiency C. Low bradykinin levels D. Mast cell degranulation E. Tryptase release |
A
CEACCP article - Angio-oedema diff dx and mx.. |
|
|
92. A 5 year-old child with recently diagnosed Duchenne muscular dystrophy has an inhalation induction with sevoflurane for closed reduction of a distal forearm fracture. No other drugs have been given. 10 minutes later the child suffers a cardiac arrest. After a further 5 minutes a venous blood sample shows a potassium level of 8.5mmol/L. The most likely mechanism for the hyperkalaemia is: |
E
See CEACCP - Anaesthesia for children with neuromuscular disease |
|
|
95. You are anaesthetising a 6 month-old infant for repair of a VSD. You perform an inhalational induction with 8% sevoflurane and 50% nitrous oxide. Several minutes later, whilst trying to secure IV access, the infant’s oxygen saturations fall to 85%. The most appropriate next step in management:
A. give a fluid bolus B. change from sevoflurane to isoflurane C. apply CPAP D. reduce the FiO2 E. reduce sevoflurane |
E
|
|
|
96. A 30-year old patient, who takes paroxetine, has suffered a traumatic amputation. The most appropriate medication to reduce her developing chronic post-operative pain is: |
C. gabapentin
See ANZCA acute pain management book p240 Key message: 2. Calcitonin, morphine, ketamine, gabapentin, amitriptyline and tramadol reduce phantom limb pain. |
|
|
97. A 3 year old child has suffered a fractured arm. What is the most appropriate way to assess her pain?
A. the reported severity from the child B. the reported severity from the parent C. the reported severity from the nursing staff D. using the FLACC scale E. the Wong-Baker Faces scale |
D
FLACC until about 4-5 years old, then Wong baker faces can be used for children able to self-report (ANZCA Acute Pain Mx 2010 p342) |
|
|
98 buprenorphine patch removed morning of surgery. What time till PLASMA reaches half original level
A. 12 hours B. 18 hours C. 24 hours D. 30 hours E. 36 hours |
D
|
|
|
101. [Repeat - 2013A Q48] The clinical sign that a lay person should use to decide whether to start CPR is:
A. Absent central pulse B. Absent peripheral pulse C. Loss of consciousness D. Obvious airway obstruction E. Absence of breathing |
E
ARC BLS algorithm- Start CPR if not responding and not breathing normally (no longer recommends checking pulses) |
|
|
102. [Similar to 2013A Q38] Central sensitization, resulting in prolongation of post-operative pain, is caused by:
A. Increased intra-cellular gene expression B. Increased intra-cellular magnesium C. Low frequency activation of A-delta fibres D. Primary activation of N-methyl-D-aspartate receptor E. Increased glycine as a major neurotransmitter |
A
Power & Kam p.390 |
|
|
103. [New] A 15yo girl with a newly diagnosed mediastinal mass presents for lymph node biopsy under general anaesthesia. The most important investigation to perform preoperatively is.
A. CXR B. CT chest C. MRI chest D. PET scan E. Transthoracic echocardiogram |
B. CT scan
Gotthard 2008. Anesthetic Considerations for Patients with Anterior Mediastinal Masses. - CT scanning provides the bulk of information relating to extent of a mediastinal mass, its anatomic location, and the invasion of surrounding structures - MRI not used routinely (may be helpful if posterior neurogenic tumor suspected). - PET not used for primary imaging (can be used to follow up germ-cell tumors after initial Rx). - If invasion or obstruction of vascular structures such as the pulm arteries or SVC is suspected, angiography and/or echocardiography may provide further useful information, but a high-quality CT scan usually is sufficient. |
|
|
104. [New] A 63yo woman with chronic AF has a history of hypertension, Type 2 Diabetes Mellitus and has previously had a CVA. What is her annual risk of stroke without anticoagulation?
A. <1% B. 1.9% C. 2.8% D. 4% E. 8.5% |
E
CHADs2 score: Hypertension- 1 Diabetes- 1 Prev. stroke -2 score= 4, yearly risk = 8.5% 0-1.9 1- 2.8 2- 4.0 3- 5.9 4- 8.5 Wikipedia page CHADS2 Article: Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ (2001). "Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation". JAMA 285 (22): 2864–70 |
|
|
105. [New] A 30 year old multi trauma patient one week post injury has severe ARDS. He is currently ventilated at 6ml/kg tidal volume, PEEP of 15cm H20 and pa02/Fi02 is less than 150. The next step to improve oxygenation is: |
E
PROSEVA study Among patients with severe ARDS, does prone positioning reduce all-cause mortality at 28 days when compared to supine-only positioning? Among patients with severe ARDS (P:F ratio <150 mmHg), prone positioning reduces 28-day mortality. (17% reduction in all cause mortality) See also Oh's ICU manual p381. |
|
|
106. [Repeat 2013A] The incidence and severity of vasospasm post sub arachnoid haemorrhage is greatest at: |
C
but rebleed highest in first 24 hrs Management of cerebral vasospasm. Neurosurg Rev 2006 |
|
|
107. [Repeat 2013A] The insulation on the power cord of a piece of class 1 equipment is faulty such that the active wire is in contact with the equipment casing. What will happen when the power cord is plugged in and the piece of equipment is turned on |
C
|
|
|
108. [Repeat 2013A] In adult cardiopulmonary resuscitation in the community include all of the following EXCEPT:
A. Allow equal time for chest compression and relaxation B. Chest compression at 100bpm C. C. Chest compression should be at least 5cm depth D. D. Give 2 rescue breath before commencement of CPR E. Chest compression to breaths ratio at 30:2 |
D- no longer advised to give 2 rescue breaths in case this prevents them from moving onto chest compressions if they don't want to do mouth-to-mouth
|
|
|
109. [New] Regarding intra-osseous cannulation in paediatric during resus for shock/cardio arrest, a correct statement is:
A. distal tibial above medial malleolus is preferred due to easy access B. drug reaction time is the same as central venous route C. 12G used to ensure adequate flow D. bicarbonate cannot be infused due to bone damage E. fat embolism is common complication |
B
|
|
|
110. [New] During endovascular aneurysm repair, GA is preferred due to:
A. risk of uncontrolled haemorrhage B. renal ischaemia is painful C. aorta traction is painful D. long duration of apnoea is needed E. contrast used can cause CVS instability |
D.
Possibly A. No good reference found. |
|
|
111. [Repeat 2013A Q26] A 35yo G1P0 with a dilated cardiomyopathy presents for a Caesarean section. She has an ejection fraction of 35%. The benefits of a regional anaesthetic over a general anesthetic in this patient may include:
A. decreased heart rate B. decreased systolic blood pressure C. increased ejection fraction D. decreased preload E. increased myocardial contractility |
D
|
|
|
112. [New] In attempting to make a precise diagnosis of parathyroid adenoma, you would expect all of the following are found in hyperparathyroid disease EXCEPT:
A. decreased urinary calcium B. extraosseous calcifications C. increased plasma calcium D. increased urinary phosphate E. renal calculi |
A.
little correlation between preoperative 24-hour urine calcium and preoperative serum calcium, PTH, or vitamin D levels. 24-hour urinary calcium in primary hyperparathyroidism.Clin Med Res. 2013 Dec;11(4):219-25 extraosseous calcifications can happen due to pseudogout ( calcification of extraarticular cartilage) bones, stones, abdominal moans and psychic groans. from hypercalcaemia |
|
|
115. Patient is intubated and ventilated, the ETCO2 trace below is caused by
A. Endobronchial intubation B. ETT cuff leak C. Gas sample line leak D. Spontaneous ventilation E. obstructive airway disease |
see images
|
|
|
116. Which general anaesthetic agent contributes the most to green house gas? (Now I'm not 100% sure on the stem recall, but I got the impression it was asking for the agent that is the absolute worse for green house gases (desflurane), not so much which one do we use the most and thus ends up contributing the most to the total green house gas volume (iso or sevo)
A. Desflurane B. Isoflurane C. Sevoflurane D. Propfol E. N2O |
A Desflurane
(article on respective Greenhouse gas contributions) |
|
|
119. [New] A patient's competence to give informed consent is determined by all the following EXCEPT:
A. Ability to communicate a choice B. Ability to apply reasoning C. Ability to understand consequences D. The provision of significant information E. ?? |
D? depending on what E was, as this question is querying the PATIENTs' competence, not their capacity (I think), and to give informed consent the degree of information given IS a factor.
|
|
|
120. [Repeat] A patient undergoes a femoral-popliteal bypass and has a mildly elevated troponin on day 1 post-operatively. They are otherwise asymptomatic with no other signs/symptoms of myocardial infarction and have an uneventful recovery. What do you do?
A. Arrange for a cardiology follow-up and outpatient angiogram because he is at increased risk of future myocardial infarction B. Arrange coronary angiogram as an inpatient prior to discharge C. Inform the patient that while the result is real the significance is questionable D. Repeat in one week’s time as a second troponin is a better indicator of long-term myocardial infarction risk E. Ignore the result as it is likely a laboratory error |
A – according to stoelting even a mildly elevated troponin is an indicator of future morbidity/mortality and should be referred to a cardiologist.
Among patients undergoing noncardiac surgery, the peak postoperative TnT measurement during the first 3 days after surgery was significantly associated with 30-day mortality. JAMA. 2012 Jun 6;307(21):2295-304 Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. |
|
|
121. St John's wort will reduce the effect of
A. aspirin B. clopidogrel C. dabigatran D. heparin E. warfarin |
E. warfarin.
TGA Alert- St John's wort induces CytochromeP450 enzymes and so decreases the effect of Warfarin, digoxin, theophylline There are also reasonable grounds for concern that St John's Wort may reduce the efficacy of the following medicines Increases serotonergic effects of SSRIs with increased risk of sideffects. Potentiates clopidogrel as it is a prodrug which requires conversion by p450 enzyme to become active. |
|
|
122. The most important effect of Lugol's iodine administration before thyroid surgery is
A. reduce incidence of thyroid storm B. reduce incidence of vocal cord palsy C. increase likelihood to identify and preserve parathyroid glands D. pigmentation of thyroid gland to help identify thyroid gland E. reduce vascularity of thyroid gland. |
E
J Clin Endo Metab 2007. Effect of Lugols solution on thyroid blood flow. 92(6) |
|
|
123. Performed a brachial plexus block. Normal sensation still remains in medial forearm. Which part of brachial plexus is most likely to have been missed
A. Inferior trunk B. Ulnar nerve C. Median brachial cutaneous nerve D. Anterior division E. Posterior cord |
A- inferior trunk -> medial cord -> medial cutaneous nerve of the forearm.
|
|
|
124. You are pre assessing A 70 year old patient treated for congestive cardiac failure. They are able to shower themselves and complete other ADLs but get dyspneoa on mowing the lawn. They are New York Heart Association classification
A. Class 1 B. Class 2 C. Class 3a D. Class 3b E. Class 4 |
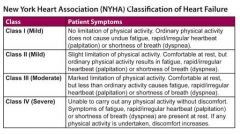
B if any symptoms at all, then can't be class 1
Canadian heart failure network (NYHA 3A/B): 3A: LImitation of physical activity. Comfortable at rest, but ordinary activity causes fatigue, palpitations or SOB. 3B: Significant limitation of physical activity. Comfortable at rest, but minimal activity causes fatigue, palpitations or SOB. |
|
|
126 Fluoroscopy in the operating theatre increases the exposure of theatre personnel to ionising radiation. Best method to minimise one's exposure to such radiation is to
A. have dosimeter checked at least 6-monthly B. limit exposure time to radiation C. maximal distance from radiation source D. stand behind transmitter of C arm E. wear protective garments |
C
|
|
|
127 Prothrombin VX (?prothrombinex VF) useful in perioperative period to correct the coagulopathic defect of all except
A. Isolated factor II deficiency B. Isolated factor VII deficiency C. Isolated factor IX deficiency D. Isolated factor X deficiency E. Warfarin |
B
Prothrombinex®-VF (product info CSL) sterile freeze-dried powder containing purified human coagulation factors II, IX and X and low levels of factors V and VII |
|
|
129. (Repeat Q) A 70 year old male presents for right lower lobectomy. Preoperative spirometry shows an FEV1 of 2.4L and an FVC of 4.2L. The predicted post-operative FEV1 is:
A. 1.0 B. 1.3 C. 1.5 D. 1.7 E. 1.9 |
D
|
|
|
130. (Repeat Q) You see a Type 1 diabetic woman preoperatively at 0700hrs who has been starved since 2200hrs for surgery today. You decide to start her on a Glucose-Insulin-Potassium infusion. Insulin decreases glucose levels by:
A. Increasing glucose uptake into hepatocytes B. Increasing glucose uptake into skeletal muscle C. Increasing gluconeogenesis D. Decreasing proteolysis E. Inhibiting glucagon release |
B.
In muscle tissues, facilitated diffusion of glucose (via GLUT-4) into skeletal and cardiac muscle cells is enhanced by insulin See Power & Kam (endo chapter) |
|
|
133. The organ that is least tolerant of ischaemia, after removal for transplant, is:
A. Cornea B. Heart C. Kidney D. Liver E. Pancreas |
B heart
BJA 2012 108 (51) i29-i42 Organ transplantation: historical perspective and current practice Heart>Lung> liver~pancreas>kidney 4:6:12:18 hours respectively |
|
|
134. 75yo woman with an ejection systolic murmur presents for elective total knee joint replacement. Focussed transthoracic echocardiogram is performed. The feature most consistent with severe aortic stenosis is:
A. Mean gradient across aortic valve of 30mmHg B. Peak gradient across aortic valve of 40mmHg C. Peak velocity across aortic valve of 4.2m/s D. Aortic valve area of 1.2cm2 E. Calcification and restriction of the aortic valve |
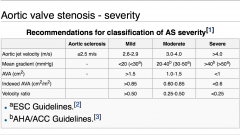
C. Peak velocity 4.2 m/s
See echopedia.org (aortic valve stenosis) Echocardiographic features of severity in AS: mean gradient > 40mmHg peak velocity > 4m/sec Valve area < 1.0 cm squared See |
|
|
135. Which of the following statements regarding patients with ankylosing spondylitis is FALSE?
A. amyloid renal infiltration is rarely seen B. cardiac complications occur in less than 10% of cases C. normochromic anaemia occurs in over 85% of cases D. sacroileitis is an early sign of presentation E. uveitis is the most common extra-articular manifestation |
C.
Approximately 15% of patients present with a normochromic normocytic anemia of chronic disease http://emedicine.medscape.com/article/332945-workup#aw2aab6b5b2 Also from that article: A. Amyloidosis is a very rare complication of AS B. Clinically significant cardiovascular involvement occurs in fewer than 10% of AS patients D. Inflammatory back pain is the most common symptom and the first manifestation in approximately 75% of patients E. Uveitis (also called iritis or iridocyclitis) is the most common extra-articular manifestation of AS, occurring in 20-30% of patients B. Stoelting C. Anaemia not a feature usually |
|
|
136. A healthy 25 year old woman is 18 weeks pregnant. Her paternal uncle has had a confirmed episode of malignant hyperthermia. She has never had susceptibility testing. Her father and siblings have not been tested either. The best test to exclude malignant hyperthermia susceptibility before she delivers is |
D muscle biopsy father
condition is autosomal dominant and best to avoid any anaesthetic if possible during pregnancy. ?E - can do IVCT under local/nerve block |
|
|
139. During the first stage of labour, pain from uterine contractions + cervical dilatation is from nerve roots: A.-E. ( multiple options of thoracic - lumbar roots ) |
T10- L1 (initially T11-12, then spreads one level each way.
Miller's 6th ed. Ch 58 Anesthesia for Obstetrics (p2316) |
|
|
140. A test has a sensitivity + specificity of 90% for a disease with a prevalence of 10%. What is the positive predictive value?
A. 10% B. 50% C. 82% D. 90% E. 99% |
B- 50%
Prevalance = 10%- this is the actual rate of disease in population screened True positives= test positive & disease positive we know disease positive is 10% from prevalance, and sensitivity is 90%, so true positive will be 9, and false negative will be 1 True Negatives= test negative and disease negative. we know disease negative will be 90%, and specificity is 90%, so true negative will be 81, and False negative will be 9. PPV = If positive test, likelihood of being disease +ve = TP/ (TP + FP) = 9/ (9+9) =0.5 (x100 to gain %) = 50% (NPV= if negative test, likelihood of being disease -ve =TN/ (TN+FN) = 81/ 82 = 0.98 or 98%) |
|
|
.141. A female with type 1 von Willebrand disease presents for a dilation and curettage. She is a Jehovah’s Witness. In regards to desmopression to prevent haemorrhage in this patient all of the following are true EXCEPT:
A. It is a synthetic substance and therefore acceptable to Jehovah's Witnesses B. It is likely to reduce haemorrhage in this patient C. It should be given as an infusion 30 minutes prior to surgery D. The effect will last 5 days E. The dose is 0.3μg/kg |
D.
See vWD oxford handbook p218. vWD CPG from RCH site. Desmopressin used in vWD type I. From emedicine: Typically, a maximal rise of vWF and FVIII is observed in 30-60 minutes. The typical maximal rise is 2- to 4-fold for vWF and 3- to 6-fold for FVIII. Additionally, hemostatic levels of both factors are usually maintained for at least 6 hours. |
|
|
142. A 25 week post conceptual age infant is being ventilated in the Neonatal Intensive Care Unit. To reduce the risk of retinopathy of prematurity, they are being ventilated to a target oxygen saturation of 85-89% instead of 91-95%. This is associated with:
A. Increased acute lung injury B. Increased mortality C. Increased sepsis D. Reduced intracerebral haemorrhage E. Reduced necrotizing enterocolitis |
B Increased mortality
Targeting an oxygen saturation below 90% with the use of current oximeters in extremely preterm infants was associated with an increased risk of death. BOOST II trial NEJM 2013 |
|
|
144. An 80 year old man undergoes a unilateral lumbar sympathectic blockade. THe most likely side effect that he experiences is:
A. Genitofemoral neuralgia B. Haematuria C. Postural hypotension D. Lumbar radiculopathy E. Psoas haematoma |
A Genitofemoral neuralgia
Waldman. Pain Management 2nd ed. Ch 164 College website. The most common complication following LSB is genitofemoral neuralgia Incidence 15% Most cases transient and resolve |
|
|
145. Regarding Le Fort fractures:
A. External signs correlate with internal skeletal damage B. Le Fort fractures don't usually occur in combination (for example I and II) C. Patients with a Le Fort I fracture should NOT undergo nasal intubation D. Patients with a Le Fort II fracture should have evaluation of the base of skull prior to nasal intubation E. Le Fort III fracture is associated with fracture of the cribiform plate |
D
A- no B- no, they often occur in combination C- Le Fort 1 is an isolated lower Maxillary fracture and often need nasal intubation to facilitate assessment of teeth occlusion by surgeons D- yes, but more commonly associated with Le Fort III fractures E- Yes and most likely correct answer. Cribiform plate is on ethmoid bone and can be fractured in extensive midline injuries. E- |
|
|
145. Greatest predictor of AF post CPB
A. advanced age B. history of hypertension C. history of CVA D. history of CCF E. prolonged CPB |
A
Predictors of Atrial Fibrillation After Coronary Artery Surgery. Circulation. 1996; 94: 390-397 Independent predictors of postop AF: increasing age 70-80 yrs [OR=2], age >80 years [OR=3], male gender (OR=1.7), hypertension (OR=1.6), need for IABP (OR=3.5), postop pneumonia (OR=3.9), ventilation >24 hours (OR=2), return to ICU (OR=3.2). Others: PHx HTN (p= 0.055), CHF (p = 0.085), prev stroke (p= 0.4), bypass time (90 vs 92 min between groups) |
|
|
146. 2yr child post op following stabismus surgery. ETT 4.5 used. Awake, stridor and tracheal tug. Immediate action?
A. inhalational induction B. CPAP with facemask C. propofol 1mg/kg D. dexamethasone 0.4mg/kg E. adrenaline nebuliser 1:1000 05ml/kg |
B- showing signs of laryngospasm
|
|
|
149. Transient neurological (radicular) syndrome ONLY occurs with
A. Hyperbaric local anaesthetics B. Intrathecal lignocaine C. Lithotomy positioning D. Following complete resolution of motor blockade E. When there has been a dense motor block with spinal anaesthetic |
D.
CEACCP 2005. Spinal anaesthesia: an update. TRANSIENT NEUROLOGICAL SYMPTOMS FOLLOWING SPINAL ANESTHESIA FOR CESAREAN SECTION 2010 Transient neurological symptoms (TNS) are defined as symmetrical bilateral pain in the back or buttocks or pain radiating to the lower extremities after recovery from spinal anesthesia |
|
|
150. 50yo lady, attempted suicide attempt, jumped from 5th floor building. She does not open her eyes or vocalise and there is no response to pressure on her nail-bed. What is her GCS?
A. 2 B. 3 C. 5 D. 8 E. 12 |
M- 1
V-1 E-1 So GCS 3- B is answer |
|
|
The features that distinguish a "cardiac protected" from body protected area is" a. Equipotent earth b. Isolating transformer c. Line isolation monitor d. maximum patient leakage of <500microamperes e. Residual current device |
A |
|
|
A 30 year old woman is admitted to ICU after a 500mg/kg aspirin overdose. What is the most effective therapy to enhacne her elimination of the aspirin? a. Frusemdie b. Haemodialysis c. Mannitol d. 0.9% Sodium Chloride e. Sodium bicarbonate |
B |
|
|
A 40yo female with primary pulmonary hypertension is to have a laparoscopic cholecsytectomy. Her preoperative PAP is 80/60mmHg. During the procedure she suddenly desaturates to 87%, BP 80/40mmHg, and ETCO2 45mmHg. Likely findings on TOE will include: A: Increased LV wall thickness, abnormal septal wall motion, TR, RA dilation B: Increased RV:LV area, abnormal septal wall motion, increased LV wall thickness, RA dilationC: Increased RV:LV area, abnormal septal wall motion, TR, RA dilation D: Increased RV:LV area, abnormal septal wall motion, TR, PR E: Increased RV:LV area, TR, PR, RA dilation |
C |
|
|
The principal resistance to airflow in an ETT is: A: density of the gas B: diameter of the tube C: length of the tube D: temperature of the gas E: viscosity of the gas |
B |

