![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
156 Cards in this Set
- Front
- Back
|
When performing a thorough clinical patient history, what are some of the things you need to ask about? |
1. Last normal 2. Presenting complaint 3. Progression of disease 4. Manifestation of disease (other symptoms) 5. Past medical history 6. Current medications/vaccine history |
|
|
What are the most important body systems to evaluate first when performing a physical exam? |
Cardiovascular Respiratory Neurologic (mentation) |
|
|
What is the shock dose of fluids for a dog? Cat? At what interval do you want to give it? What is the endpoint for shock dose therapy? |
90mL/Kg (dog) 66mL/Kg (cat) Give 1/3rd or 1/4th of the fluid and then reassess the patient to see if more has to be given When the vitals normalize |
|
|
What are the three things that diagnostic tests should help you develop? |
1. Establish a Diagnosis 2. Provide a prognosis 3. Give a treatment plan |
|
|
2nd degree AV block is normal in athletic horses. What test can you do to see if it truly normal or abnormal? |
Exercise the horse. If it goes away during exercise, it is normal. If it persists, it is abnormal |
|
|
When should a NON-emergent (either urgent or elective) surgery be performed when it comes to the best outcome for the patient? |
When the patient is stabilized (O2 sats, resp. rate, heart rate, temp, etc.) |
|
|
What are the goals of a pre-surgical assessment of a patient? |
1. Maximize the chance of success, minimize the risk of complications 2. Make the correct diagnosis and associated surgical plan 3. Decide if the surgery is emergent, urgent or elective 4. Recognize co-morbidities that may exist that may complicate or delay surgery |
|
|
In an older injury, what are some of additional questions you ask in order to take a thorough history? |
1. Condition of animal now? Has it changed since the time of the injury? 2. What has happened since? 3. Any therapy done since the injury? Changes in the animal with the therapy? 4. New problems that have developed? |
|
|
If you have signs of systemic illness in a patient, would you consider this an emergency, urgent or elective? |
Emergency |
|
|
In a blocked cat, what nutritional imbalance would be the cause of a bradycardia? What would an ECG look like? How would you treat? |

Hyperkalemia Tall T waves, prolonged PR interval, absent P waves, wide/bizarre QRS You would want to stablize the hyperkalemia first- give 3cc/cat of calcium gluconate immediately. |
|
|
Draw out the DO2 diagram as presented by Dr. Beal What are the three pathological paths to shock? |
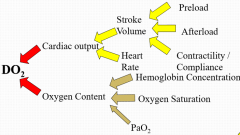
Failure of delivery of O2 to tissues (DO2), most common Failure of utilization of O2 by the tissues DO2/VO2 mismatch |
|
|
Explain why shock can eventually lead to death and should be taken seriously |
Shock alters metabolism, leading to decreased ATP, increased lactic acid, cell and organ failure and then eventually animal death |
|
|
What reactions in the body are seen when Cardiac output is decreased |
1. Increase in sympathetic nervous system, increasing MAP, Stroke volume, H2O and Na retention 2. Increase in renin/angiotensin leading to increased Na/H2O retention and MAP 3. Increase ADH leading to increased H2O retention |
|
|
What is the number one thing you must do before giving any fluid therapy to a shock patient? What signs would warrant you to not give fluids? |
Perform a physical exam in order to rule out cardiogenic shock! Cardiogenic shock has symptoms of arrhythmias, murmurs, perihilar edema, distended jugulars, gallop, muffled heart sounds, pulsus paradoxus, abdominal effusion, crackles/increased lung sounds Giving fluid to a cardiogenic shock patient can kill the patient! |
|
|
When considering what type of fluid you should give to a shock patient, what types of things do you want to think about? |
1. Cause of edema 2. Electrolyte status 3. [Hgb]/PCV 4. [albumin] 5. Other concurrent diseases |
|
|
What are the types of crystalloid fluids that are available? What kind of situation can you use them? |
LRS, Normosol-R or 0.9% NaCl Safe to use them in any hypovolemic patient, no matter what caused the hypovolemia |
|
|
What is the blood volume of a dog? Cat? Why do we give the whole blood volume in fluids to a shock patient? With what percentage of fluid loss do we start to see clinical signs? Hypovolemia? Death? |
90mL/Kg- dog, 66mL/Kg- cat We give the whole amount because only 1/4 of what you give will stay in the vasculature and the rest will end up in the ISF 10-15% loss = minimal clinical signs 20-25% loss = hypovolemic shock >40% = fatal without therapy |
|
|
With colloids, what is the rate at which we give them? Why is it this number? What are some advantages and disadvantages to using colloids? |
Expansion rate of 20mL/Kg is the same as giving 90mL/Kg of crystalloids (get rapid volume expansion) It stays in the vasculature better They are expensive, cause some hemostatic abnormalities and can cause acute kidney injury. Generally, they are not used. |
|
|
When giving blood, what PCV do you want to be at before you start administering? While you are administering, what should the PCV be at What is the general rule between volume of blood and anemia? |
You don't want to wait for the PCV to drop, give when needed, not when PCV says to give it. Animal can die from blood loss and still have normal PCV. Keep it at 20-25% PCV Better to be euvolemic and anemic rather than hypovolemic and anemic. |
|
|
When having a 23% hypertonic saline solution, what level of dilution do you want it to be at before you administer it? What is the rate at which you give it? What are some advantages/disadvantages of using these? |
<7.5% Dose is 5mL/Kg given at a max rate of 1mL/Kg/min You get rapid volume expansion but given too fast and you can get reflex bradycardia and hypernatremia |
|
|
What is the definition of cardiogenic shock? |
Decreased DO2 due to cardiac disease |
|
|
What are the signs on physical exam that would be consistent with cardiogenic shock and pericardial effusion? |
Distended jugulars Muffled heart sounds Pulsus paradoxus Abdominal effusion |
|
|
What are your causes of right sided cardiogenic shock? |
Pericardial Effusion Caval Syndrome PTE Pulmonic Stenosis Cardiac Arrhythmias |
|
|
What are your causes of left sided cardiogenic shock? |
Severe mitral regurgitation DCM Sub-aortic stenosis HCM Cardiac Arrhythmias |
|
|
What is pulsus paradoxus? What is the pathophysiology behind it? |
Where the pulse gets weaker on inspiration and stronger on expiration It is caused when the pressure in the heart decreases, increasing the filling of the R heart. Then, the septum moves to the left and the stroke volume on the right side of the heart goes up, changing the pulse |
|
|
What is one treatment that is always therapeutic, no matter what cause of cardiogenic shock? |
Oxygen therapy |
|
|
If you had cardiogenic shock due to a pericardial effusion, what would your treatment be? |
Pericadiocentesis |
|
|
If you had cardiogenic shock due to heartworm caval syndrome, what would your treatment be? |
Removal, adulticides |
|
|
If you had cardiogenic shock due to a bradyarryhthmia, what would your treatment be? |
Anticholinergics first (atropine, glycopyrrolate) Then beta-agonists if that doesn't work (dobutamine) Pacemaker if severe enoug |
|
|
If you had cardiogenic shock due to a tachyarrhythmia, what would your treatment be? |
(decreased diastolic filling time with a heart rate of >180bpm) Diltiazam Beta blockers (Amiodorone) |
|
|
If you had cardiogenic shock with normotension and pulmonary edema from CHF, what would your treatment be? |
Diuretics (decrease the preload, decrease the pressure in the vasculature) Veno/mixed vasodilators- Nitroglycerine/Nitroprusside |
|
|
Before giving venodilators, what do you want to make sure of? |
Normal BP (systolic >100mmHg) |
|
|
How does dobutamine work as a cardiac drug? What precautions do you want to take with it? |
It is a beta-1 agonist mostly (some Beta-2 activity) Improves contractility in dogs Can cause seizures in cats |
|
|
What is SIRS and how do you define it? |
Systemic inflammatory response system If a canine meets 2 or more criteria, it meets SIRS criteria HR > 180bpm, HR <40, PaCO2 <30mmHg, Temp <100.4 or >104, Leukogram <5,000/microliter or >18,000WBC/microliter |
|
|
Define: Sepsis Severe Sepsis Septic Shock |
Sepsis = SIRS + Infection Severe sepsis = Sepsis + Organ dysfunction, hypoperfusion, hypotension Septic shock = sepsis + arterial hypotension (sys < 90mmHg, MAP < 60mmHg) |
|
|
What are the two categorical causes of septic shock? |
Cardiogenic or hypovolemic Decreased VO2 with adequate DO2 |
|
|
What are the early and late clinical signs associated with septic shock? |
Early- red mm, increased CRT, HR, Pulse pressure and decreased mentation Late- pale mm, Decreased CRT, pulse pressure, mentation with increased HR |
|
|
What are the four causes of septic shock in veterinary medicine? |
Septic Peritonitis Pneumonia Pyothorax Urogenital Infection |
|
|
What are the goals and treatments associated with septic shock? |
1. Increase CaO2 with oxygen therapy or blood transfusion if needed 2. Increase Cardiac output with volume expansion (first) then pressor therapy (second) 3. EARLY AGGRESSIVE ANTIBIOTICS 4. Maintain normoglycemia 5. Nutrition as soon as hemodynamically stable 6. Treat coagulation insufficiencies 7. Corticosteroids if unresponsive to pressors 8. TREAT UNDERLYING CONDITIONS |
|
|
After giving therapy, what kind of responses are you looking for? |
Normalization of BP, urine output (1mL/Kg/Hr), PCV/TS, Lactate, pH, Bicarbonate, arterial blood gas SpO2 > 95% |
|
|
What electrolyte imbalances and acid base status would a patient with a high GI obstruction present with? |
Hypochloremia Hypokalemia Metabolic Acidosis |
|
|
What electrolyte imbalances would an animal with addison's disease have? |
Hyponatremia Hyperkalemia |
|
|
With hypvolemia and hypercalcemia, what fluid choice would you use? Why? |
0.9% saline, promotes calciuresis |
|
|
How would you resuscitate a hypovolemic head patient? |
Never volume resuscitate a head patient. Just don't |
|
|
If you have too much or not enough [H+], what kinds of change can occur in the body? What level of [H+] is compatible with life? pH compatible with life? how is H+ excreted? |
You can get a change in proteins- their charge conformation and function. You can also get a change in cellular and organ function as a result. [H+] = 12-160nEq/L (50-100mEq made every day with metabolism, a lot has to get excreted) pH= 6.8-7.8 Excreted by the kidneys |
|
|
How is CO2 excreted in the body? What is TCO2 representative of? |
Through respiratory excretion TCO2 is related to [HCO3-], not PaCO2 |
|
|
HCO3- is inversely related to what? What is the definition of a base excess? How do you 'calculate' it? |
Inversely related to [H+] Base excess is how much excess base (or deficit of base) there is in the animal Conceptually it is Patient HCO3- - Normal HCO3- |
|
|
What is the normal... PaCO2? HCO3-? pH? |
PaCO2- 35mmHg HCO3-: 22mEq/L pH: 7.4 |
|
|
In regards to speed, how long does respiratory compensation take? Metabolic compensation? |
Respiratory- takes only minutes Metabolic partial compensation happens in 24 hours, full compensation takes 2-3 days |
|
|
Compare an ABG and a VBG in terms of: What sides of an A/B problem you can evaluate If compensation can be calculated What other things you can tell How easy it is to get a sample |
Both is good to evaluate the metabolic side, only the ABG is good for evaluating the respiratory side ABG is better for calculating compensation, VBG you can only get a minimum PaCO2 (about 5 lower than ABG but that can't be concluded definitively) ABG can be used to look for hypovolemia and you can calculate an A-a gradient VBG is easier to obtain |
|
|
What changes in pH, PaCO2 and HCO3- would you expect to see in metabolic acidosis? What is the reason for the changes seen in each? What compensation equation would you use for metabolic acidosis? |
pH would go down (increased acid in body) HCO3- would go down (suggests acidosis) PRIMARY PaCO2 would go down to compensate (suggests primary alkalosis, SECONDARY) in order to blow off more acid (CO2) Exp CO2 = 35 - ([22-[HCO3-]] x 0.7) +/- 3 |
|
|
What are the 4 causes of metabolic acidosis? How do you treat these? |
Lactic acidosis (increased lactate due to increased anaerobic glycolysis) Diabetic Ketoacidosis (DKA) Failure to excrete excess [H+] (renal failure) Increased exogenous acids (ethylene glycol) In severe cases you can give bicarbonate but in most cases, treating the underlying cause will result in rapid resolution of the acidosis |
|
|
What kinds of effects does metabolic acidosis have on the body? |
Decreased CO, MAP, hepatic/renal blood flow, contractility Venous constriction Ventricular arrhythmias Hyperkalemia |
|
|
Describe a situation in which lactate levels can be prognostic? |
In GDV, if you have less Lactate at time of presentation, you are more likely to have a better prognosis |
|
|
What changes in pH, PaCO2 and HCO3- would you expect to see in metabolic alkalosis? What is the reason for the changes seen in each? What compensation equation would you use for metabolic alkalosis? |
You would expect pH to go up (decreased acid) As a primary change, you would expect HCO3- to go up because less is needed as a buffer As a secondary change, you would expect PaCO2 to go up because the animal is hypoventilating to compensate. Expected CO2= 35 + ([HCO3-] x 0.7) +/-2 |
|
|
What are the 4 causes of metabolic alkalosis? |
High GI obstruction Loop diuretic therapy (ex. Furosemide) Gastric Suctioning Vomitting |
|
|
What is the pathophysiology of metabolic alkalosis caused by high GI obstruction? What other CBC findings would be supportive of a high GI obstruction? |
The obstruction causes a loss of HCl, leading to the body retaining HCO3- to replace the Cl lost. Hypochloremia, Hyperkalemia, Hyperaldosterone |
|
|
What changes in pH, PaCO2 and HCO3- would you expect to see in respiratory acidosis? What is the reason for the changes seen in each? What compensation equation would you use for respiratory acidosis? |
pH would be down (excess acid) PaCO2 would go up because they are not breathing enough of the excess CO2 off HCO3- would go up in order to buffer the excess acid (suggests alkalosis) HCO3- = 22 + [(PaCO2) - 35) x 0.15 +/- 2 mEq/L |
|
|
What are the causes for respiratory acidosis? Is this a life threatening problem? How do you fix this imbalance? |
Upper airway obstruction Severe primary pulmonary conditions Decreased CNS drive Neuromuscular conditions Bellows Disease Pleural space disease it is life threatening but will take 12-15 minutes to die of this. Most animals will die of hypoxia first which only takes a few minutes. Treat the underlying cause, DON'T give bicarb |
|
|
What changes in pH, PaCO2 and HCO3- would you expect to see in respiratory alkalosis ? What is the reason for the changes seen in each? What compensation equation would you use for respiratory alkalosis? |
pH would go up (reduced amount of acid) PaCO2 would do down as the primary cause, blowing off too much acid HCO3- as a secondary cause would go down because the buffer is decreasing in order to preserve acid HCO3- = 22 - [35-(PaCO2)] x .25 +/-2 mEq/L |
|
|
What are the causes of respiratory alkalosis? |
Hypoxemia Pulmonary disease Overzealous ventilation CNS derived hyperventilation |
|
|
When a dog comes in with GDV, what kind of Acid/Base disturbance do you expect to see? |
Can have any blood-gas abnormality, mixed is often common |
|
|
What percentage of body weight is total body water? ICF? ECF?- what things make up the ECF? What kind of things can affect the normal amount of water in a particular patient? |
60% of total BW is water 40% of BW is ICF 20% of BW is ECF (plasma, interstitial, lymph, transcellular fluids) body water decreases as age increases and fat content increases |
|
|
What is the normal blood volume for a dog? Cat? |
Dog- 90mL/Kg Cat- 66mL/Kg |
|
|
What are some of the sources of water intake? what are some of the source of output? What other changes in a CBC would you expect to see from decreased intake or increased output? |
Intake- food, free water, byproducts from metabolism Output- urinary, fecal, insensible (respiratory/skin losses) Decreased intake (fasting/dehydration)- Decrease in K and P Increased output (from vomiting)- decrease in H2O, H, Cl, Na, K and HCO3- |
|
|
What are some examples of the following categories of water loss? Isotonic Hypertonic Hypotonic |
Isotonic- vomiting, diarrhea, blood loss, third space loss Hypertonic- loop diuretics, Addison's Hypotonic- Renal loss, Respiratory loss, burns |
|
|
What is the normal urine output for an animal? |
1mL/Kg/Hr |
|
|
What is the rate for surgical fluid maintenance? |
10-20mL/Kg/Hr |
|
|
What is the difference between hypovolemia and dehydration? how should each situation be treated with fluids? |
Hypovolemia is the acute loss of fluids and the fluids need to be replaced as quickly as possible Dehydration is the chronic loss of fluids and the fluids are usually replaced over a 24-36 hour period (any faster and just urine output increases) |
|
|
What are some of the clinical signs that would point to hypovolemia in a patient? |
Dogs would be tachycardic (HR >140) Cats would be bradycardic (or "normal", HR <140) Tacky mm increased respiratory rate Depressed mentation Normal heart RHYTHM |
|
|
What are the normal TPRs for a dog and a cat? |
Dog: HR- 60-120bpm RR-10-30bpm, T-100.5-102.5 Cat: HR- 160-220bpm RR-10-30bpm, T-100.5-102.5 |
|
|
if a patient is 5% dehydration, what clinical signs would you see? 8%? 10%? |
5%- (mild)- loss of skin pliability, tacky mm 8%- (moderate)- dry mm, sunken eyes, mental depression 10%- (severe)- shock, altered mentation, sunken and dull eyes |
|
|
What are some of the reasons that evaluation of dehydration by just physical exam is difficult to do? |
Fat animals appear to be less dehydrated than they are Emaciated animals appear to be more dehydrated than they are Individual animal/breed variety Observer variation |
|
|
What are some of the other parameters you can use to monitor hydration status? |
Body weight PCV/TS Urine Output/Specific gravity BUN, Creatinine Na concentration |
|
|
How often should body weight be checked if you are using this to monitor hydration status? Can you use this as an initial fluid therapy plan? What about PCV/TS? |
Monitor body weight daily. It can only be used as part of your original fluid configuration only if the pre-dehydration weight is known. PCV/TS should only be used as a serial monitor after therapy as most of the time the pre-therapy numbers are not known |
|
|
What is the urine specific gravity of a patient that is dehydrated? |
>1040 |
|
|
If fluids are given that should have been accurate but still no urine is being produced, what value should you check? How is this measured and what does it tell you? |
Check a CVP (central venous pressure) CVP is a measurement of right atrial pressure and preload To measure, put a catheter in the jugular with the tip cranial to the right atrium, the stopcock should remain at the level of the right atrium and then the pressure is measured using a pressure transducer. Normal should be 0-5cmH2O and the pressure normally fluctuates with respiration. |
|
|
How does the CVP change in each of these situations? Shock Overhydration CHF Cardiac Tamponade |
Shock < (or equal to) 0 Overhydration 8-12 CHF 18-20 Cardiac Tamponade 22-25 |
|
|
Describe how you would perform a "poorman's CVP" |
Tip the animal's head back and look at the jugular Measure the distance from the thoracic inlet until it disappears. If the length is lengthened, you have a distended jugular and a increased CVP |
|
|
How do you distinguish between pre-renal azotemia and renal azotemia when considering hydration status? |
Pre-renal azotemia will go away with fluid therapy Renal azotemia will persist after fluid therapy |
|
|
How do you calculate a dog's fluid loss over a 24 hour period? |
Deficit + Maintenance + Ongoing losses = total needed/24 hours Deficit = BW x % dehydrated = X (mL) Maintenance = 60mL/kg/day (dog) or 48mL/Kg/day (cat) Ongoing losses (estimated) |
|
|
When is using oral fluids a good choice? |
When fluid needs are not immediate, dehydration is not severe and when there is no GI disease present that would reduce the effectiveness of the fluids. |
|
|
In what type of situations would you want to use IV fluids? |
When the need is immediate, precise control is needed, parenteral nutrition *the fluid must be sterile! |
|
|
In what type of situations would you want to use subcutaneous fluids? |
When there is mild dehydration, rapid disease resolution is expected, hospitalization is not needed/can't be done *fluids must be isotonic and sterile |
|
|
Compare Replacement fluids and Maintenance fluids: What kind of fluids do they replace in the body? What kinds of electrolyte concentrations do they have? Which can be used for fluid boluses? Types? |
Replacement- replaced deficits, has a Na concentration similar to that of plasma LRS, Normasol-R, Plasmalyte-A, 0.9% saline Maintenance- meet ongoing losses, has lower NaCl and is hypotonic (focus is to replace free water) NEVER used as fluid boluses! D5W, Plasmalyte-56, Normasol-M, 5% Dextrose |
|
|
If you were looking for a balance, isotonic crystalloid, what fluids can you use? What is an unbalanced, isotonic crystalloid that you can use? Hypertonic crystalloid? |
Balanced, Isotonic- LRS, Normosol-R, Plasmalyte-A Unbalanced, isotonic- 0.9% saline Hypertonic- hypertonic saline |
|
|
What types of situations can you use 0.9% saline for? |
Metabolic alkalosis Hypochloremia Hyponatremia Hyperkalemia Hypercalcemia |
|
|
What type of situations would you use a hypertonic saline? |
Rapid ECF expansion, when small volume resuscitation is needed |
|
|
Define: Hydrostatic pressure Colloid Oncotic pressure |
Hydrostatic- pressure exerted by fluid itself Colloid oncotic pressure- osmotic pressure exerted by large molecules (proteins) |
|
|
Define: A balanced fluid An isotonic fluid A buffered solution |
Balanced: similar CONCENTRATION to plasma Isotonic: similar NUMBER OF PARTICLES to plasma Buffered- lactate/acetate turns it into HCO3- |
|
|
What are the daily requirements for: H20 Na K Calories (in a dog) |
H20- 625-720cc Na- 20mEq K-17mEq Calories-700-800 |
|
|
What is a colloid? When are they theoretically used? What kind of disadvantages do they come with? |
Colloid is a synthetic/natural fluid with large particles (Plasma, hetastarch) They are usually used when plasma oncotic pressure is low However, they cause dilutional coagulopathy, platelet coating and acute renal failure They should not be used |
|
|
What advantage does giving plasma do for the patient? |
Supplies clotting factors |
|
|
What is oxyglobin? |
they are colloids that have oxygen carrying capacity (currently not on the market but may be a new product coming out) |
|
|
When is a blood transfusion warranted? |
When O2 carrying capacity is low (PCV of 20% in a pre-surgical patient) When anemia is getting worse |
|
|
No matter what, when is the endpoint for fluid therapy? |
Adequate perfusion and hemodynamically stable |
|
|
Can you give fluids too fast in dogs? How about in cats? |
In dogs- no. All signs of overhydration will subside with no longterm effects In cats, the lung is the shock organ and overload can lead to pulmonary edema. Be careful not to do this, bolus cats at a rate of 10mL/Kg first then reassess. |
|
|
Define: Oliguria Anuria Until proven otherwise, these are what type of renal disorder? |
Oliguria- Decreased urine output Anuria- No urine output Pre-renal dysfunction until proven otherwise |
|
|
What are the three thoughts that can cause oliguria/anuria after fluid therapy? |
Not enough fluids Acute renal failure Urinary tract rupture/block |
|
|
Before making the diagnosis of acute oliguric renal failure, what things must you check first? |
1. Make sure enough fluids have been given, by looking at PE, BW, CVP 2. Assess adequate renal perfusion (arterial blood pressure, Cardiac output) |
|
|
When you have an oliguric patient, what is your plan? |
1. Identify underlying cause 2. Discontinue all nephrotoxic drugs 3. Assess volume status 4. Replace volume deficits rapidly 5. Treat hyperkalemia and acidosis 6. Assess urine output 7. Measure CVP, weight (with a CVP of <8, give more fluids) |
|
|
What things can you use to stimulate urine production? If you have a patient that was oliguric and then suddenly starts producing urine again, why do they then become polyuric? |
Furosemide, Mannitol, Dialysis They become polyuric for a short while because the tubular epithelium has to replicate and become new again, increase fluids during this time and when urine output normalizes, then you can wean off of fluids. |
|
|
What is the normal Potassium requirement of an animal/day? What are the causes and clinical signs of hypokalemia? |
1+ mEq/Kg/day Anorexia, vomitting, diarrhea, alkalosis, fluid therapy, diuresis Muscle weakness and cardiac arrhythmias |
|
|
What is the maximum rate at which you can supplement potassium? If you have a patient with normal potassium rates, what types of situations would you still want to give potassium? At what rate would you give it? |
MAX of 0.5mEq/Kg/Hr If a patient has ongoing losses or will be on fluid for a long time, supplement with potassium at a rate of 20mEq/L *make sure the rate is safe at all times |
|
|
What situations would you want to be cautious when using fluids? |
Heart disease Unknown cause respiratory disease Anuria with volume overload Head trauma Pulmonary contusion |
|
|
What are the associated terminology associated with cleaning inanimate objects? Living tissue? |
Inanimate- sterilized and disinfected with a disinfectant (disinfectants kill microbes) Living tissue- treated with antiseptics to kill microbes, can be given antibiotics to alter microbial activity |
|
|
Where does endogenous bacteria come from? Exogenous? |
Endogenous- normal flora of skin, oropharynx and GI tract Exogenous- from environment |
|
|
Which is better for instrument disinfection, physical or chemical disinfection? |
Physical |
|
|
How does steam sterilization work? What is the time needed to sterilize instruments? What does the indicator indicate? |
Transfers heat by condensation, must touch all of the surfaces to whatever is being sterilized The amount of time needed to kill Bacillus Stearothermophilus >10 to the 6th Indicators change when exposed to steam |
|
|
Compare how each of the three types of steam autoclaves work. Gravity displacement Prevacuum Steam Sterilizers Steam Pulsing system |
Gravity- gravity pushes out the air out of the bottom, slower sterilization Prevacuum- air is vacuumed out before steam is introduced, flash sterilization but expensive Steam Pulsing- pulse at high pressure then venting is repeated, middle in time and cost |
|
|
How does Ethylene Oxide Sterilization work, what are its downfalls? |
Cyclic ether gas cycle, gas concentration, temp, exposure time, humidity all changes its effectiveness. This is VERY toxic, needs to aerate for 8-72hours in order to allow gas to dissipate Ineffective in presence of water or organic debris |
|
|
What are the advantages of using H2O2 gas plasma sterilization? |
No toxic gases, low temp sterilization, only takes 1 hour |
|
|
What are the downsides to cold sterilization? |
Not everything is destroyed, cannot be used for anything that penetrates the skin |
|
|
What are the steps you want to take in clipping a patient before surgery? |
Clip wide (use 40# blade or 10# for a heavy coat) Clip right before surgery Vacuum up the hair Clip in a separate room from where the surgery will take place |
|
|
What are some of the steps you want to take before scrubbing but after clipping (most of these are surgery dependent) |
Wrap/hand distal limb Flush prepuce Lubricate eyes Anal purse string/express bladder |
|
|
What is the function of the dirty skin scrub? Final scrub? What cleaning solution is typically preferred? why? |
Dirty scrub moves gross debris Final scrub is aseptic, move from center to periphery Chlorhexidine is usually preferred. It is broad spectrum, works with the presence of organic material, minimal toxicity, look for alcohol based |
|
|
What are the best drapes for surgery? |
Can be economical, sterilized, impermeable
Reusable or disposable (Disposable, Nonwoven drapes are preferred) |
|
|
What are the steps in getting the surgeon ready for surgery? |
Scrubs- just surgery, not worn from home, top tucked in Footwear- closed toe, clean, comfortable Head cover- worn by all, cover/contain all hair Masks- worn always if sterile pack is open Hands/nail care- short nail, no polish, no jewelry, no open wounds, generally clean Hand scrub- aqueous (chlorhexidine > povidine-iodine- 6 min scrub, 3-5 min after that, more expensive) alcohol- no water needed,faster, cheaper, better CONTACT TIME is very important Gloves- they can break or get punctured, double-gloved if needed |
|
|
What are halsted's principles? |
Gentle tissue handling Aseptic technique Sharp dissection Careful hemostasis Obliterate dead tissues Avoid tension Rest |
|
|
What are some of the things you want to have in a surgical suite? |
Positive air pressure from the ceiling to the floor Nonporous operating surfaces |
|
|
What are the role of the following in wound healing: Growth factors Cytokines Chemokines |
Growth factors- activate cell proliferation/differentiation Cytokines- regulate/coordinate immune responses, secreted by leukocytes Chemokines- cytokines with a chemotactic function |
|
|
How long does the inflammatory phase of wound healing typically last? What important events happen during this phase? |
T0 - 5 days after wound is made Hemostasis, platelet aggregation/degranulation, neutrophil and monocyte chemotaxis |
|
|
What are the functions of neutrophils in wound healing? Are these a sign of infection? |
Kill bacteria, breakdown ECM, phagocytosis, further cytokine release This is NOT a sign of wound infection, this is a normal part of healing! |
|
|
What are the functions of the monocytes in wound healing? What are these ESSENTIAL for? |
Monocytes migrate into a wound area, become macrophages *become the primary leukocyte by 48-96 hours Phagocytosis, proteolysis, removal of bacteria Essential for further signaling molecules and for wound healing |
|
|
How long does the proliferation phase of wound healing last? What is the function of this phase and what cells are at play? |
Day 4-12+ (depending on wound location, size, patient age/health) Fibroblasts, endothelium, epithhelium Wound closure, lost tissue replacement (angiogenesis, fibroplasia, contraction, epithilization) |
|
|
What is angiogenesis? how long does it take to see angiogenesis in a wound? |
Capillaries sprout from existing vasculature You can see angiogenesis 4 days after a wound is created |
|
|
What is fibroplasia? What is the function of the fibroblast? What is the function of TGF-beta? |
Fibroplasia is the proliferation of fibroblasts so they can lay down type 3 collagen TGF-beta lays down Type 1 collagen, they peak at day 7-14 of wound healing |
|
|
Angiogenesis + Fibroplasia = ? |
Granulation tissue |
|
|
How is contraction accomplished in wound healing? When does contraction stop? |
Contraction is when the anchored myofibroblasts pull the wound edges closer together, after granulation tissue has filled the wound. It ends when the wound edges have been brought together or when the myofibroblasts have reached their max stretch capacity |
|
|
How does epithelization happen and when does it stop? How can you tell a wound closed by epithilization and not contraction? |
The epithelial cells proliferate, they migrate across the granulation tissue as a monolayer Continues until the wound edges meet Epitelization brings no hair follicles with it so a wound closed by this method will have no hair |
|
|
What events happen in the maturation phase of wound healing? |
Decrease in granulation tissue, increase in mature scar tissue The time until the scar is at its maximum strength depends on the loading, depends on the tissue |
|
|
What are some of the general characteristics of a wound or patient that affects the rate of healing? |
Infection Hypoxia Cancer Blockage of inflammation Tension Patient health/age |
|
|
Describe how the gut usually heals: What is the most important layer? Why? What is meant by the lag phase? What kinds of things can affect the rate of healing? |
The gut heals by epithelization, going through all of the phases of healing but smooth muscle can make collagen, types 1,3 and 5 The submucosa is the most important layer because of the nerves blood supply and lymph in this layer. The lag phase is the phase 3-5 days after surgery in which the animal is most prone to leakage due to collagen breakdown Intraop hypotension, early feeding, bacteria/infection, apposition, NSAIDS can either increase or decrease gut healing. |
|
|
What are the differences in bone healing when compared to gut healing? |
BMP is stimulated in bone healing which helps stimulate bone progenitor cells |
|
|
How long does it take each of these to reach full strength? Skin Colon Stomach Bladder Fascia |
Skin- 3mo. Colon- 28 days Stomach and bladder- 21 fascia- 6 months *bladder will be the only one to improve to its original strength, all others will be forever weaker than its original strength |
|
|
What is different about the way that horses heal? Cats? |
Horses- make exuberant granulation tissue Cats- wound strength, granulation speed and increased amount of subcutaneous tissues all mean that healing is slower |
|
|
What are all of the different absorbable suture options available? |
Synthetic rapidly absorbable- monofilament (monocryl) and multifilament (vicryl) Synthetic prolonged absorbable- multifilament (vicryl) Natural rapidly absorbable (chromic gut) |
|
|
What are all of the different nonabsorbable suture categories available? |
Synthetic monofilament (nylon, propylene) or multifilament (braunamid) Natural multifilament (silk) |
|
|
What are the different ways you can chose to allow a wound to heal? |
primary/1st intention- sew it up right away Delayed 1st intention- closure within 3-5 days of the wounding 2nd intention- leave open, allow to heal by contraction/epithelization 3rd intention- close after a granulation bed has been established |
|
|
What are the 4 ways you classify a wound? Describe each classification. |
Clean- aseptic, no infection, not into tubular organ Clean contaminated- aseptic, no infection, into a tubular organ Contaminated- not aseptic (or breach in asepsis), no infection, fresh (5-8 hours) Dirty- not aseptic, infection present or older, over 8 hours old |
|
|
What is the definition of prophylactic antibiotic use? When do you give them? |
Given during the procedure only (and then stopped after surgery UNLESS infection was present) Give when you have a clean-contaminated procedure, implant placed, longer procedure, infection would be deadly or the health/age of the patient indicates them |
|
|
When do you give therapeutic antibiotics? |
Treat likely/existing infection- dirty/contaminated, they are continued after the surgery |
|
|
What are the expected flora seen in a surgical procedure? |
Staph aureus and epidermidis (normal skin flora) *colon, expect anaerobes and colliforms- plan for bacteria based on location of surgery |
|
|
When do you want to close a wound? |
Clean, clean contaminated or contaminated wound with drainage When the tension on the wound is manageable or you can use a skin flap to close it |
|
|
That are the 4 tenets of wound care? |
Cleanse Debride Lavage Dress |
|
|
What are the things you want to consider when cleaning a wound? What can you use? What steps do you take? |
Cover wound with lube or something to cover the wound Clip generously around the wound Scrub with chlorhexidine Cleanse actual wound with 0.5% CHG, 0.1% povodine-iodine, or 0.01%-0.02% Dakin's solution |
|
|
What are the different ways you can debride a wound? |
Chemical Biologic (maggots) Mechanical (surgery) |
|
|
How long do you want to lavage out a wound? At what pressure? What can you use? What can't you use? |
5-10 minutes, at a high pressure (about 8psi) Can use tap water, saline, 0.5% CHG, 0.1% povodine-iodine, 0.01%-0.02% Dakin's solution DONT use- hydrogen peroxide, detergents, concentrated antiseptics, alcohol |
|
|
What are your goals for your primary layer of wound dressing? What are your options? |
Plan for any drainage, tissue necrosis or epithelization that may happen Options include Wet to dry/Dry to dry, alignates, silastic foam, hydrogel/hydrocolloids, petrolatum-impregnated gauze or tefla "nonadherent" dressings |
|
|
Describe how a wet to dry bandage works and what advantages it has How is this different from a dry to dry bandage? |
Wet dry is soaked with saline before placed on. This saline will draw water out of the wound and adhere to the open wound. Then, when the bandage is changed, it has to be ripped off and this provides mechanical debridement of the wound Dry to dry does the same thing but it is dry when put on (better for more exudative wounds) |
|
|
How do alignates work? What phases of wound healing can you use them in? |
They are algae that turn into a gel when put on the wound. This causes autolytic debridement. Safe to use in infection and can be used in the inflammatory and proliferative phases |
|
|
How does silastic foam work? Hydrogel/hydrocolloids? |
Silastic foam is a nonadherent, absorptive, autolytic debridement, can be used in inflammatory and proliferative phase Hydrogels/Hydrocolloids provide moisture (not for use in exudative wounds), causes autolytic debridement and promotes granulation tissue |
|
|
What is petrolatum-impregnated gauze? |
A gauze used that is good for 2nd intention healing, may mildly depress epithelization though |
|
|
What is tefla "nonabsorbant" dressing? |
Absorbent material between porous film Provides a medical layer that can be used to cover sutures |
|
|
What does negative pressure therapy do for wound management? |
Can be continuous or intermittent Stimulates cell proliferation and reduced edema Can treat for days before wound closure |
|
|
What are the principles of managing an infected wound? |
Drainage Source control Implant removal Culture-based antibiotics |

