![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Analgesia |
Stage on anesthesia in which the patient is relaxed and conscious |
|
|
|
Anesthesia |
Temp loss of feeling or sensation |
|
|
|
Anesthetic |
Medication the produces temporary loss of feeling or sensation |
|
|
|
Aspirate |
To draw back or draw within |
|
|
|
Diffuse |
Spread from an area of high concentration to one of low concentration |
|
|
|
Duration |
Time |
|
|
|
Gauge |
Standard dimension or measurement of the thickness of an injected needle |
|
|
|
Induction |
Find from infection to effective anesthesia |
|
|
|
Innervation |
Supply or distribution of nerves to a specific body part |
|
|
|
Lumen |
Hollow center of the infection needle |
|
|
|
Oximetry |
Measurement of oxygen in the blood |
|
|
|
Permeate |
The spread of flow throughout |
|
|
|
Porous |
Describes an object with minute openings that allow the passage of gas or fluid |
|
|
|
Systemic toxity |
A harmful reaction to a drug that affects one or more moody systems |
|
|
|
Tidal volume |
Amount of air inhaled and exhaled with each breath |
|
|
|
Titrate |
Determine the effective dosage of analgesic by increasing the dosage until the desired effect is achieved |
|
|
|
Vasoconstrictor |
Type of that that constricts blood vessels used to prolong anesthetic action |
|
|
|
Types of anxiety and pain control medications |
Topical anesthesia Local anesthesia Inhalation sedation Anti anxiety agents Intravenous sedation General anesthesia Mind body medicine |
|
|
|
Topical |
Purpose in dentistry is to provide numbing effect in a specific area where an injection is to take place. Provide temp numbing effect on nerve endings located on the surface of the oral mucous. Chemicals include benzocaine or lidocaine and available in cream, liquids, slays and patches |
|
|
|
Local anesthesia |
Important role in reducing pain and discomfort during dental care. Used for pain control in dentistry and good for all forms Characteristics - nonirritating to tissues in the area of injection, associated with min toxicity, rapid onset, able to provide profound pain relief, sufficient duration, completely reversible, sterile or capable of being sterilized by head without deterioration |
|
|
|
Method of actions (Local) |
Local anesthesia is obtained by injecting a solution near the nerve where treatment is to take place. Temp blocks the ability of the nerve membrane to generate impulse After the injection is completed the anesthetic diffuses or spreads into the nerve and blocks it’s normal action. Nerve must permeated |
|
|
|
Chemical composition of anesthetics (local) |
Come under two chemical groups - amides metabolized by liver and esters metabolize by plasma. Each local anesthetic cartridge including a combo of: Local anesthetic drug - choice depends on procedure, health of patient, dentist presence Sodium chloride - makes solution isotonic with body tissues Distilled water - supplies and added volume of solution |
|
|
|
Time span of anesthetics |
Important consideration when selecting local is the time span of pain control required. Induction is then length of time it takes to work and duration is the length of time it works. A short acting local agent can last 30 mins Intermediate local agent lasts 60 mins Long acting lasts 90 min |
|
|
|
Vasoconstrictors |
Is an afternoon that when combine with anesthetic slows down the uptake of agent into the bloodstreams to increase the duration of action. Blood vessels to the site of admin are constricted, absorption into cardiovascular system is slowed, local toxicity is minimized due to lower blood level, prolonged anesthetic duration, bleeding at infection is deceased |
|
|
|
Contradictions to vasoconstrictors |
Because it may cause stain on the heart local is absorbed into the body, the use of an anesthetic solution without vasoconstrictors is recommended for patients with history of heart disease, may interact with certain drugs a patient is taken, use correct ratio |
|
|
|
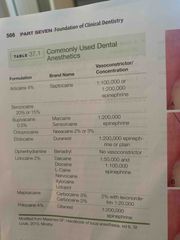
Commonly used dental anesthetics |
Articaine 4% - Septocaine - 1:100 000 or 1:200 000 epinephrine Benzocaine 20% or 15% Bupovacaine 0.5 % - Marciane Or sensorcaine 1:200 000 epinephrine Chloprocaine - Nesacaine 2% or 3% Etidocaine - Duranest - 1:200 000 epinephrine or plain Diphenhydramine - Benadryl - no vaso Lidocaine 2% - 1:50 000 and 1:100 000 epinephrine |
|
|
|
Infection techniques |
Location and the innervation of the tooth to be anaesthetized will determine with topical is place and type of infection to be given |
|
|
|
Maxillary anesthesia |
Porous nature of alveolar cancerous bone. allows the solution to diffuse through the bone and reach apices of teeth in a different manner 3 injection types Local infiltration - injection into a small isolated area Field block - infection near a large terminal nerve branch - when two ore more teeth are being restore Nerve block - occurs when anesthetic is deposited close to a main nerve trunk. This is indicated for quadrant dentistry (nasoplatine nerve block) |
|
|
|
Palatal anesthesia |
anterior or great palatine block which provides anesthesia in the posterior portion of the hard plane And the nasoplatine nerve block does the anterior hard palate |
|
|
|
Mandibular anesthesia |
Hard for solution to diffuse easily. Inferior alveolar block - often referred to as dibular nerve block is obtained by injected the anesthetic solution near but not into branches of the inferior alveolar nerve close to Mandibular forearm. Patient will experience numbness over half of the lower jaw including teeth, tongue and lips. Buccal nerve block - proves anesthetic to Buccal soft tissues close the Mandibular morals Incisive nerve block - is given only when Mandibular anterior teeth or premolars . |
|
|
|
Periodontal ligament infection |
Alternative infiltration technique that involves infection of the solution under pressure directly into the periodontal ligament and surrounding tissues. Generally adjunct (additional) to conventional techniques |
|
|
|
Local Anaesthesia set up - Syringe |
Anesthetic syringe is made up of the following parts Thumb ring,finger grip - allows dentist control the syringe firmly and aspirate effectively with one hand Harpoon - sharp hook that locks into the rubber stopper of cartridge so the stopper can be retracted by pulling back Posted rod - rod pushes the rubber stopper of the cartridge and forces solution out Barrel of the syringe - holds solution Threaded tip (needle adaptor) - hub of the needle is attached to the syringe |
|
|
|
Local Anaesthesia set up - Cartridges |
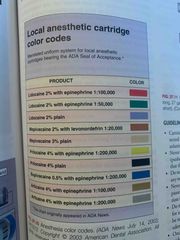
Solutions suppled in glass cartridges. These have rubber or silicone stopper at one end and an aluminum cap with rubber diaphragm at other end. Supplied in blister packs that have been sterilized and stored in sealed environment Color codling carriages - American dental association council of scientific affairs created a standardized for all injectable local products that chose to participate in system. For dentist to easily recognize different types of concentrations of anesthetic Guidelines for handling cartridges: Should be stored at room temp and out of sunlight, never use one that has been frozen, don’t use if cracked, don’t use it cloudy or discoloured, don’t leave syringe preloaded, one needle and syringe have been assembled discard the cartridge, never save for reuse |
|
|
|
Local Anaesthesia set up - color codes |
Back (Definition) |
|
|
|
Local Anaesthesia set up - disposable needle |
Sterile needle is used for injection is projected by a two part plastic covering. The needle should not be used if seal is broken. Cartridge end of needle is shorter end or the needle as it fits through the threaded tip of the syringe and punctures rubber diaphragm. Needle hub is the self the eating plastic or metal used to attach needle to syringe Injection end the end the punctures the skin. Short needle is 1inch and used for infiltration and long needle is 1 5/8 inch and used for block. The end of the needle beveled (angled) the beveled end should be toward the bone Lumen is the hollow centre or the needle where solution flows Gauge refers to the thickness of the needle. Larger the gauge thinner the needle and smaller the gauge thicker the needle. Most frequent gauge numbers are 25,27, 30 due to being longer needles they need more strength |
|
|
|
Complications and precautions |
Injecting into a blood vessel Infected areas Toxic reactions - localized/systemic Temp numbness Paresthesia - numbness lasts when it should have worn off due to contaminated solution, trauma to the nerve, hemorrhage. Temp or perm. If temp it can last up to 8 weeks |
|
|
|
Electronic anesthesia |
Innovative, noninvasive form. The system is designed to block pain electronically with the use of low current electricity Are is isolated and dried. Third pad is placed intraoral receptor attached to the lingual side 3-5mm above gingival margin. No needles, no post operative numbness or swelling, chemical free, no risk of cross contamination, reduces fear and anxiety, patient control |
|
|
|
Inhalation sedation |
Also referred to as nitrous oxide/oxygen (NO2/O2) May be the safest type of sedation is dentistry is used properly. Produces stage 1 anesthesia by using a combo of NO2 and O2 gases. The patient inhales has through nosepiece feeling effect almost instantly |
|
|
|
Advantages/Disadvantages of NO2 |
Advantages- admin is simple and easy managed, excellent safety record, pleasant and relaxing, patient is awake, recovery is rapid, used for all ages Disadvantages - some patients may experience nausea or vertigo, patients with behavioural challenges may react in an adverse way and act out |
|
|
|
Contradictions or N2O |
Pulmonary disorders Respiratory infections Pregnancy - no evidence it harms the bay though Psychiatric disorders Immune compromised MS Drug use. Middle ear blockage Apprehensive patient Alcoholic or recovering |
|
|
|
Chemical make up |
N20 chemical name dinitrogen monoixode is tasteless, ordorless, colourless has that is compressed into blue cylinders. 650-900lb per square inch |
|
|
|
Effects of nitrous oxide |
Toxic is used improperly - safest max allowance is 50 parts per million (ppm) used only during patient treatment and never used recreational. |
|
|
|
Equipment |
Gas cylinder - green is for often and blue for nitrous oxide and the gases are stored in the cylinder Control valves - used to control the flow of gas Flow meter - indicates rate of flow Reservoir bag is where the two gases composed Gas hose - carries the gas from the bag to noise peice Mask/nose piece |
|
|
|
Patient assessment and monitoring |
Always review patients medication and history incase there’s something that will cause and issue Check vitals |
|
|
|
Patient education |
Patient should be informed what to expect. Describe how gas is Amin, proper use of mask and nose piece, and sensations of warm and tingling patient will feel. |
|
|
|
Administration |
Should begin with admin of 100% oxygen. Start with pure oxygen while establishing patients tidal volume and then slowing titrate or determine N2O concentration until desired results are achieved. Then should end with oxygen for 3-5 minutes afterwards Patient should reframe from talking After patient feels normal post operative vital signs are checked and compared with before Don’t let patients drive home if you believe there is a risk |
|
|
|
Safety work practice for the clinical team N2O |
Scavenger system - reduces N2O released into treatment room Venting exhaust fumes outside Testing pressure connections Inspect equipment Properly fitting mask Limit talking Exposure assmentent |
|
|
|
Anti anxiety medications |
Amin for the relief of anxiety in larger doses these drugs can produce sleep, sedation, and anesthesia. Anti anxiety agents can be orally, IV, or inhaled. Sensations can be used for patients very nervous apprehensive to procedure, if procedure is difficult and long, mentally challenged patients, very young kids Most common method is use of short acting benzodiazepines (diazepam) either alone or with opid analgesic (morphine) Normally taken 30-60 mins prior |
|
|
|
IV sedation |
Baseline vitals and patients weight should be taken before dose determination IC conscious sedation results in minimally depressed level of consciousness. Patient maintains ability to keep an open airway and respond IV conscious - unconscious |
|
|
|
General anesthesia |
Another method to admin anti anxiety is through general. General is controlled state of unconsciousness characterized by loss of protective reflexes including the ability to maintain the airway independent and respond to psychical stimulation. It’s achieved by combo of gases and in agents. Admin in the hospital or surgical setting. Only special physicians can admin |
|
|
|
4 stages of anesthesia |
1 - patient is relaxed and fully conscious 2 less away of immediate surroundings 3 - general anesthesia- not awake Stage 4 respiratory failure or cardiac arrest |
|
|
|
Patient prep |
To use general patient must understand and sign consent form |
|
|
|
Patient recovery |
One procedure is done patient is monitored closely until normally reflexes return. Patient should respond to name and be able to move limbs and such. Well patient is waking up they should never be left alone |
|
|
|
Document |
Review of patients medical history Pre op and post op vitals Type of anesthesia used Tidal volume Time began and end Peak concentration admin Post op time Adverse events or complications |
|

