![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
149 Cards in this Set
- Front
- Back
|
Metabolism
- definition - 2 types |
Sum of all of the reactions that happen in the body
* catabolic : complex -> simple - release/produce/provide energy - proteins, carbs into amino acids or glucose * anabolic : simple -> complex - use/consume/burn energy |
|
|
Three major destinations for principle nutrients (carbs, proteins, fats, minerals, and vitamins)
|
energy for active processes, synthesis into structural or functional molecules, storage as fat or glycogen for later use as energy
|
|
|
Feeding (hunger) center and Satiety center
- how do they affect each other? - what are other stimuli they affect them? |
located in the hypothalamus, related to the regulation of food intake. The feeding center is constantly active but may be inhibited by the satiety center.
Stimuli that affect the two centers are: glucose, amino acids, lipids, body temperature, distention of the GI tract, and cholecystokinin (CCK). |
|
|
Basal Metabolic Rate (BMR) - simple definition
|
measurement of the metabolic rate under basal conditions
|
|
|
Conditions for BMR
|
* no exercise for 30-60 minutes prior
* comfortable air temp * fasting for at least 12 hours * normal body temperature |
|
|
What does BMR measure
|
it is a measure of the rate at which the quiet, resting, fasting body breaks down nutrients to liberate energy.
BMR is ALSO A MEASURE OF HOW MUCH THYROXINE THE THYROID GLAND IS PRODUCING, since thyroxine regulates the rate of ATP use and is not a controllable factor under basal conditions |
|
|
How is BMR most often measured
|
indirectly by measuring oxygen consumption using a respirometer. It is usually expressed in kilocalories per square meter of body area per hour (kcal/M2/hr)
consuming more 02 = higher BMR (all things being equal) |
|
|
Constant core temperature
|
98.6 degrees F or 37 degrees C - regulated by the hypothalamus
|
|
|
Core temperature vs shell temperature
|
Core temperature refers to the body's temperature in the body structures below the skin and subcutaneous tissue. More specifically it refers to the temperatures of the abdominal, thoracic and cranial cavities.
Shell temperature refers to the body's temperature at the surface, that is the skin, the muscle, and the subcutaneous tissue Too high a core temperature kills by denaturing body proteins, while too low a core temperature causes cardiac arrhythmias |
|
|
Heat conservation mechanisms
|
vasoconstriction, sympathetic stimulation, skeletal muscle contraction (shivering), and thyroid hormone production
|
|
|
Mechanisms of heat loss
|
vasodilation, decreased metabolic rate, decreased skeletal muscle contraction, and perspiration
|
|
|
Radiation, Conduction, Convection, and Evaporation
|
Radiation - warm -> cool object, without contact
Conduction - BODY heat -> substance/object (ex: chairs, clothing, jewelry, air, water) Convection - BODY -> liquid/gas (contact of air or water w/ body results in heat transfer by both conduction (3%) and convection (12%)) Evaporation - liquid -> vapor, requires a great deal of heat, rate of evaporation is inversely related to relative humidity |
|
|
Fever
- definition - most common reason - fever producing substance |
an abnormally high body temperature most probably caused by prostaglandins with interleukin-1 and mediators.
The most common reason for fever is infection from bacteria (and their toxins) and viruses. A fever-producing substance is called a pyrogen |
|
|
Cost/Benefits of a Fever
|
- Up to a point, fever is beneficial in helping to fight infection and increase rate of tissue repair during the course of a disease
- alerts us that there is in fact something wrong with the body - Problem: fever, dehydration, acidosis, permanent brain damage, denaturation of proteins/enzymes |
|
|
Hypothermia
|
refers to a lowering of body temperature to 35 degrees C (95 degrees F) or below. It may be caused by an overwhelming cold stress, metabolic diseases, drugs, burns, malnutrition, transection of the cervical spinal cord, and lowering of body temperature for surgery
|
|
|
Oxidation
|
Removal of electron or hydrogen or addition of and oxygen.
|
|
|
Reduction
|
Removal of an oxygen or addition of an electron or hydrogen
|
|
|
Glycogenesis
- what is it - stimulated by - storage potential |
Conversion of glucose to glycogen for storage in the liver and skeletal muscle
* stimulated by insulin * the body can store about 500g (1.1lb) of glycogen, about 25% in the liver and 75% in the skeletal muscles |
|
|
Glycogenolysis
- what is it - when does it occur - stimulated by |
Conversion of glycogen back to glucose
* occurs between meals * stimulated by glucagon and epinephrine |
|
|
Gluconeogenesis
- how does it work - stimulated by |
Conversion of protein or fat molecules into glucose
* glycerol may be converted to glyceraldehydes 3 phosphate * some amino acids may be converted to pyruvic acid * both of these compounds may enter the Krebs cycle to provide energy Gluconeogenesis is stimulated by: cortisol, thyroid hormone, epinephrine, glucagon, and human growth hormone (hGH) |
|
|
Glycolysis
|
Breakdown of glucose into CO2 (carbon dioxide) and H20 (water) --> release a lot of energy, almost 38 ATP
|
|
|
Fate of Carbohydrates - what do we do with our glucose?
|
Store it, burn it, or change it
|
|
|
Lipogenesis
|
If glycogen storage areas are filled up, liver cells and fat cells can convert glucose to glycerol and fatty acids that can be used for synthesis of tryglycerides (neutral fats)
|
|
|
What sometimes happens to excess glucose, particularly in diabetics?
|
it is excreted through the urine
|
|
|
Glucose Oxidation
- alternative name - where and why does it occur - process |
aka cellular respiration. occurs in every cell of the body except RBCs which lack mitochondria and provides the cell's chief source of energy
the complete oxidation of glucose to CO2 and H2O produces large amounts of energy and occurs in four successive stages: glycolysis, formation of acetyl coA, the Krebs cycle, and the electron transport chain |
|
|
Glycolysis
-where does it occur - structure - net ATP gain - aerobic vs anaerobic |
Occurs in the Cytoplasm (NO MITOCHONDRIA!!)
refers to the breakdown of glucose: C6H1206 into 2 pyruvic acids (C3H6O3) produce 4 ATP - consume 2 ATP = net gain 2 ATP When oxygen is in short supply (anaerobic) , pyruvic acid is reduced to lactic acid under aerobic conditions: pyruvic acid is converted to acetyl coenzyme A and enters the Krebs cycle |
|
|
Formation of Acetyl CoA
|
Pyruvic Acid is prepared for entrance into the Krebs cycle by conversion to a two carbon compound (acetyl group) followed by the addition of coenzyme A (CoA) to form coenzyme A (acetyl coA)
CoA is derived from pantothenic acid, a B vitamin |
|
|
Krebs Cycle
- alternative names - where does it occur - what does it produce (end product): molecules? ATP? |
aka citric acid cycle or tricarboxylic acid (TCA)
occurs in the matrix (center) of the mitochondria step three of glucose oxidation produces 3 CO2, 4 NADH + H+, 1 FADH2, 1 GTP = 2 ATP (0 ATP consumed) |
|
|
Electron Transport Chain
- where does it occur - final electron receptor - ATP yield |
occurs in the inner mitochondrial membrane
aerobic - last electron receptor of the chain is Oxygen (O2) --> final oxidation is irreversible most productive step - yields 32 to 36 ATP (only net gain, we do not consume) and several molecules of H2O |
|
|
Complete oxidation of glucose yields?
|
C6H12O6 + 6O2 -> 36 or 38 ATP + 6CO2 + 6H2O
|
|
|
Flavin mononucleotide (FMN), cytochromes, iron-sulfur (Fe-S) centers, copper atoms, and ubiquinones (also coenzyme Q, or just Q)
|
During Electron Transport chain there are other substances that help with energy production, without which the process cannot occur
Sometimes if you have poisoning, then you will not have energy production |
|
|
Chemiosmosis
|
H+ is expelled from within the inner mitochondrial matrix, creating an electrochemical gradient.
ATP synthesis then occurs as H+ diffuses back into the mitochondrial matrix through a special type of H+ channel (pore) in the inner membrane. |
|
|
Can cells perform their activities for the body sufficiently without oxygen?
|
Can they perform them - yes, for a few minutes
Sufficiently - no |
|
|
Fate of Lipids
|
oxidized to produce ATP
stored in adipose tissue used as structural molecules or to synthesize essential molecules such as phospholipids of plasma membranes; lipoproteins that transport cholesterol; thromboplastin for blood clotting; and cholesterol used to synthesize bile salts and steroid hormones |
|
|
Insulin vs Glucagon vs Epinephrine and its effects on fat
|
Insulin --> lipogenesis
Epinephrine/Adrenaline/Glucagon --> lipolysis (produce more energy) |
|
|
Ketogenesis vs Ketosis (or diabetic ketoacidosis)
|
when body can't absorb blood glucose, breaks down fat for energy , releases ketones as byproduct --> acidosis
|
|
|
Where are amino acids absorbed?
|
capillaries of villi and enter the liver via the hepatic portal vein
|
|
|
Fate of proteins
|
Amino acids, under the influence of human growth hormone (hGH) and insulin, enter body cells by active transport.
Inside cells, amino acids are synthesized into proteins that function as: enzymes, transport molecules, antibodies, clotting chemicals, hormones, contractile elements in muscle fibers, and structural elements. They may also be stored as fat or glycogen or used for energy |
|
|
What kind of hormone is insulin?
|
anabolic - helps make more storage
|
|
|
Protein Synthesis
- stimulated by - where is it carried out? by? |
* human growth hormone, thyroxine, and insulin
* ribosomes (basically every cell) --> DNA and RNA |
|
|
Amino Acids
- How many in the body - Essential - Nonessential |
* 20
* 10 - cannot be synthesized by molecules present within the body - plants or bacteria - "essential" for human growth and must be part of diet * can be synthesized by process called transamination Once all 20 are present, protein synthesis occurs rapidly |
|
|
Absorptive (Fed) State
|
Ingested nutrients enter the blood and lymph from the GI tract, and glucose is readily available for ATP production
*average meal requires 4 hours for complete absorption * body spends avg. 12 hours in this state * soon after eating, gastric inhibitory peptide (GIP) and the rise in blood glucose concentration stimulate insulin release form pancreatic beta cells. In several ways, insulin stimulates absorptive state metabolism. |
|
|
Post-absorptive (fasting) state
|
Absorption is complete, and the energy needs of the body must be satisfied by nutrients already present in the body
* major concern: maintain normal BGL: 70-110 mg/100ml of blood * glycerol --> glucose (hydrolysis of triglycerides in adipose) * during prolonged fasting, large amounts of amino acids from tissue breakdown (primarily from skeletal muscle) are released to be converted to glucose in the liver by gluconeogenesis |
|
|
As long as water is consumed, what happens if a person tries to fast long term?
|
the most important molecule is fat, the body will start burning fat for glucose. The glucose level will not drop more than 25% from its normal range
|
|
|
Hormones that stimulate metabolism in the post-abosorptive state
|
Sometimes called anti-insulin hormones because they counter the insulin effects that dominate the fed state. The most important anti-insulin hormone is glucagon
|
|
|
Calorie Requirements
- women and older people - active women and most men - ten bodys and active men |
- 1600 calories
- 2200 calories - 2800 calories |
|
|
Minerals
|
inorganic substances that help regulate body processes
* known to perform essential functions include: calcium (bone, muscle, heart, nerve, blood vessels) phosphorus (ATP, DNA/RNA, bone) sodium and chlorine (outside cells) potassium (inside cells) magnesium (heart) iron, sulfur, iodine (thyroid), manganese, cobalt, copper, zinc, selenium, and chromium |
|
|
Vitamins
|
organic nutrients that maintain growth and normal metabolism. Many function in enzyme systems as coenzymes
* most cannot be synthesized by the body * fat soluble: emulsified into micelles and absorbed along with ingested dietary fats by the small intestine. K= hemostasis, E = skin, allergies, immunity. D = calcium absorption. A = vision. * Water Soluble: absorbed along with water in the GI tract and dissolve in body fluids. B vitamins = energy, electron transport chain/Krebs and vitamin C= immunity |
|
|
Obesity
|
body weight
|
|
|
Morbid Obesity
|
refers to obese people who weigh twice their ideal weight or more. The condition is so named because it is associated with serious and life threatening conditions; surgery may be indicated to control weight
|
|
|
Malnutrition
|
refers to a state of bad or poor nutrition.
* causes include fasting, anorexia nervosa, deprivation, cancer, gastrointestinal obstructions, inability to swallow, renal disease and poor dentition * imbalance of nutrients, malabsorption of nutrients, improper distribution of nutrients, inability to nutrients, increased nutrient requirements , increased nutrient losses ; and over nutrition * loss of energy stores in form of glycogen, fats, and proteins is referred to as starvation |
|
|
Kwashiorkor vs marasmus
|
Kwashiorkor - results from a deficient protein intake despite normal or nearly normal intake (form of edema)
Marasmus - inadequate of both protein and calories |
|
|
Phenylketonuria (PKU)
|
genetic error of metabolism characterized by elevation of phenylalanine in the blood.
Child born with PKU cannot metabolize the amino acid properly and it may build up to toxic levels in the blood, causing damage to the nervous system. If diagnosed early, can prevent such damage with dietary restrictions -> test is routinely done on infants |
|
|
Primary function of the urinary system
|
help maintain homeostasis by controlling the composition, volume, and pressure of the blood
what is now urine, was blood only moments ago |
|
|
The organs of the urinary system:
|
kidneys - ureters - bladder - urethra
|
|
|
Three layers of tissue surround each kidney
|
inner most Renal capsule, adipose capsule, and outer renal fascia
|
|
|
Nephrotosis
|
floating kidney - downward displacement or dropping of the kidney. Thin persons are most susceptible because their adipose capsule or renal fascia may be deficient, allowing slippage. Dangerous because ureter may kink
|
|

|
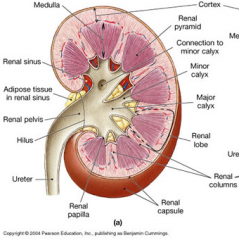
until your kidney has failed like 70/80% you do not need
Blood enters the kidney through the renal artery and exits through the renal vein |
|
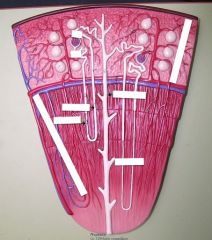
Nephron
|
* renal corpuscle - where fluid is filtered
* renal tubule - in which filtered fluid passes * nephron performs 3 basic functions: glomerular filtration (everything will be filtered out except large proteins like albumin and cells) , tubular reabsorption, and tubular secretion |
|

Renal Corpuscle
|
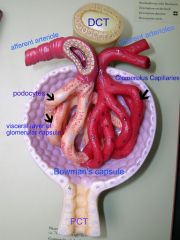
* Glomerulus surrounded by Bowman's capsule lined by podocytes
|
|
|
Renal Tubule
|
PCT = proximal convoluted tubule
* descending limb of loop of henle * Loop of henle * ascending limb of loop of henle DCT = distal convoluted tubule * collecting duct * papillary duct |
|
|
Cortical nephron vs Juxtamedullary nephron
|
Cortical (closer or primarily in the cortex): usually has its glomerulus in the outer portion of the cortex and a short loop of henle that penetrates only into the outer region of the medulla
Juxtamedullary: usually has its glomerulus deep in the cortex close to the medulla; its long loop of henle stretches through the medulla and almost reaches the renal papilla |
|
|
Juxtaglomerular apparatus (JGA)
|
juxtaglomerular cells of an afferent arteriole + macula densa cells
helps regulate blood pressure and rate of blood filtration by the kidneys If dehydrated --> will dilate to allow more fluid in to glomerulus |
|
|
Renal Tubule is lined with what kind of cells?
|
epithelial cells: simple cuboidal
|
|
|
Loop of Henle
|
reabsorption of water and electrolytes
|
|
|
Glomerular Blood Hydrostatic Pressure
|
when blood enters the glomerulus, the blood pressure forces water and dissolved blood components forward through the membrane
resulting fluid = glomerular filtrate filtration fraction = % of plasma entering the kidneys that becomes glomerular filtrate most solutes in blood plasma (except proteins) enter filtrate, normally blood cells and proteins are not filtered |
|
|
Net filtration pressure (NFP)
|
Filtration of blood is promoted by Glomerular Blood Hydrostatic Pressure (GBHP) and is opposed by Capsular Hydrostatic Pressure (CHP) and Blood Colloid Osmotic Pressure (BCOP).
The net filtration pressure = 10 mmHg |
|
|
Glomerular filtration rate (GFR)
|
amount of filtrate formed in both kidneys per minute; in the normal adult, it is about 125 ml/min. or 180 l/day or 50 gallons/day.
this means that blood is cleaned approximately 30-40 times in one day |
|
|
Anuria
|
production of less than 50 ml/day of urine.
if glomerular blood hydrostatic pressure falls to 45 mmHg (normal 55mHg), filtration ceases because because the glomerular the glomerular blood hydrostatic pressure exactly equals opposing pressures |
|
|
Harmful side effects of kidney disease(s) --> plasma proteins enter the filtrate
|
damaged glomerular capillaries become so permeable that plasma proteins enter the filtrate, causing an increase in net filtration pressure (NFP) and glomerular filtration rate (GFR) and a decrease in blood colloid osmotic pressure (BCOP) --> swelling and edema
|
|
|
Glomerular blood flow depends on?
|
* Renal autoregulation(Juxtaglomerular cells)
* Hormonal regulation - angiotensin II (vasoconstrictor) - atrial natriuretic peptide (less pressure) * neural regulation (sympathetic: increase BP, adrenaline) |
|
|
Sodium Reabsorption
|
Reabsorption of sodium ions is especially important because more of them pass the glomerular filter than any other substance except water.
They are reabsorbed in each portion of the renal tubule Active transport of Na+ promotes reabsorption of water by osmosis |
|
|
Where does most reabsorption occur
|
approximately 65% of reabsorption occurs in the PCT (proximal convoluted tubule)
|
|
|
Transport Maximum of Glucose
|
normally all filtered glucose and amino acids are reabsorbed in the PCT by Na+ symporters. each type of symporter has an upper limit on how fast it can work, called Tmax (Tm).
If the blood concentration of glucose is above normal or if there is a malfunction in the tubular carrier mechanism, all of the glucose cannot be reabsorbed; the excess remains in the urine --> glycosuria glucose is transported via facilitated diffusion |
|
|
Loop of Henle reabsorbs filtered solutes.
- via what process - what solutes - how is it regulated |
- osmosis
- 30% K+, 20% Na+, 35% Cl-, 15% water - independent regulation of both your total body water and tonicity of body fluids |
|
|
Two hormones that regulate reabsorption in the final portion of the DCT and collecting ducts
|
aldosterone and antidiuretic hormone (ADH)
|
|
|
Obligatory water reabsorption vs Facultative water reabsorption
|
90% of total water reabsorption occurs via osmosis, accompanying reabsorption of solutes such as sodium and glucose.
Regulated by ADH - this 10% is important because when you're cycling 30-40 times a day, this equals a significant amount of blood. In a few days, if you were to continuously let this amount go, in a few days you would die |
|
|
Normal ions in the urine
|
potassium, hydrogen, ammonium, urea, creatinine --> at any level in the urine = good
urea and creatinine in the blood = bad |
|
|
Tubular secretion has two principal effects
|
it rids the body of certain materials
helps control blood pH by secreting H+ and increasing or decreasing HCO3- production how we compensate for acidosis/alkalosis |
|
|
When ADH level is low
- what disease is associated with this? |
the kidneys produce dilute urine and excrete excess water, in other words, renal tubules absorb more solutes than water
urinate more diabetes insipidus |
|
|
Diuretics
|
drugs that increase urine flow rate.
Work by a variety of mechanisms, most potent ones are loop diuretics, such as furosemide which inhibits the symporters in the thick ascending limb of the loop of Henle |
|
|
Screening tests for kidney function
|
Blood urea nitrogen (BUN) - measures the level of nitrogen in the blood that is part of urea
Another test is a measurement of plasma creatinine Renal plasma clearance: how effectively kidneys remove clear substance from plasma * inulin (dye) gives glomerular filtration rate * para-aminohippuric acid (PAHA) gives rate of renal plasma flow |
|
|
Hemodialysis
CAPD |
filter blood through artificial kidney to remove wastes and add nutrients
portable method of dialysis: continuous peritoneal dialysis (CAPD) |
|
|
Ureters
|
retroperitoneal - consist of a mucosa, muscular is, and fibrous coat
transport urine from the renal pelvis to the urinary bladder, primarily by peristalsis, but hydrostatic pressure and gravity also contribute occasionally the crystals of salts present in urine may solidify into insoluble stones called renal calculi (kidney stones/calcium stones/phosphate stones) |
|
|
Urinary Bladder
|
located in the pelvic cavity and functions to store urine before micturition (urination)
floor of the bladder, smooth triangular area = trigone. * ureters enter @ posterior points in the triangle * urethra drains @ anterior point of the triangle consists of a mucosa (with rugae), lamina propria, muscularis (detrusor muscle), and serous coat (serosa) * internal urethral sphincter (circular fibers of muscularis) * below internal, external urethral sphincter (skeletal, voluntary muscle) |
|
|
Micturition/Urination/Voiding
|
When the volume of urine in the bladder reaches a certain amount (usually 200-400 ml), stretch receptors in the bladder wall transmit impulses that initiate spinal micturition reflex
A lack of voluntary control over urination is referred to a incontinence Failure to void urine completely or normally is termed retention |
|
|
Urethra
|
a tube leading from the flood of bladder to the exterior
wall of urethra consists of three coats in females, or two coats in males Function: discharge urine from the body. Male urethra also serves as the duct for ejaculation of semen (reproductive fluid) |
|
|
Urinalysis
- what typically varies in a healthy person - what physical characteristics are evaluated - what is the chemical makeup |
the by-product of the kidneys activities is urine. In a healthy person, urine volume, pH and solute concentration vary with the needs of the internal environment
Physical characteristics evaluated: volume, color, turbidity, odor, pH, and specific gravity Chemically, normal urine contains about 95% water and 5% solutes. The solutes are both organic and inorganic. The are derived from cellular metabolism and outside sources such as drugs |
|
|
Gonads
|
testes and ovaries - produce gametes
|
|
|
The ducts in order
|
ductus Epididymis, Ductus (vas) deferens, ejaculatory duct, urethra
|
|
|
Scrotum
|
cutaneous out pouching of the abdomen that supports the testes
production and survival of spermatozoa require a temperature that is lower than normal core body temperature (regulated by cremaster muscle) |
|
|
Testes
1. failure to descend 2. seminiferous tubules 3. sustentacular cells 4. interstitial endocrincytes |
1. cryptorchidism (one or both)
2. sperm cells are made 3. aka sertoli cells (helper cells: movement) - support and protect developing spermatogenic cells 4. aka insterstitial cells of Leydig - produce male sex hormone -> testosterone |
|
|
Spermatogenesis
1. Mitosis 2. Meiosis Results |
occurs in the testes
1. Identical cell division: somatic cells - each daughter cell receives the full complement of 23 chromosome pairs (46 chromosomes) --> diploid (2n) 2. germ cells - pairs of chromosomes are so that the gamete has only 23 chromosomes --> haploid (n). * Results = four haploid spermatozoa from each primary spermatocyte * immature spermatogonia develop into mature spermatozoa. The spermatogenesis sequence includes: reduction division (meiosis I), equatorial division (meiosis II), and spermatogenesis |
|
|
Mature Sperm
- appearance - life expectancy and amt. - function |
consist of a head, mid piece, and tail
produced at a rate of 300 million/day and once ejaculated have a life expectancy of 48 hrs within the female reproductive tract Function: fertilize secondary oocyte |
|
|
Puberty and Hormones
- where do they come from - what do they stimulate - what do their stimulations secrete These secretions initiate what process and stimulate the production of what hormone? |
Gonadotropin releasing hormone (GnRH) - from the hypothalamus stimulates the anterior pituitary to secrete follicle stimulating hormone (FSH) and Luteinizing hormone (LH).
FSH initiates spermatogenesis and LH assists spermatogenesis and stimulates production of testosterone |
|
|
Testosterone
|
controls the growth, development, functioning, and maintenance of sex organs
Stimulates bone growth, protein anabolism, and sperm maturation Stimulates development of male secondary sex characteristics Negative feedback systems regulate production |
|
|
Inhibin
|
produced by sustentacular (sertoli) cells.
Inhibition of FSH by inhibit helps to regulate the rate of spermatogenesis |
|
|
Accessory Sex Glands
|
Seminal vesicles, Prostate gland, Bulbourethral (cowpers) gland, and several supporting structures including the penis
|
|
|
Testes
- where do they develop - passage - two types of hernia |
- testes start at abdominal wall and move through inguinal canal into scrotum
- indirect hernia: intestine goes through inguinal canal through testes - direct hernia: weakness in belly, intestine bulges out |
|
|
Duct system of the testes
|
Seminiferous tubules, straight tubules, rete testis
|
|
|
Spermatic Cord
|
ductus (vas) deferens, testicular artery, autonomic nerves, testicular vein, lymphatic vessels, cremaster muscle
|
|
|
Inguinal canal
|
represents a weak spot in the abdominal wall - frequently a site of inguinal hernia (Females less often have hernias here)
|
|
|
Penile Urethra is also known as (2 other names)
|
spongy or cavernous
|
|
|
Accessory Sex Glands
- Seminal Vesicles - Prostate Gland |
- secrete an alkaline, viscous fluid that constitutes about 60% of the volume of semen and contributes to sperm motility and viability
- slightly acidic fluid that constitutes 13-33% of the volume of semen and contributes to sperm motility and viability * often enlarges beyond normal size attained at maturity after 45 |
|
|
Two tests for prostate cancer
|
Prostatic Acid Phosphatase (PS)
Prostate - Specific Antigen (PSA) |
|
|
Bulbourethral (Cowper's) gland
|
secretes mucus for lubrication and an alkaline substance that neutralizes acid - helps in changing the pH
|
|
|
Semen
|
(seminal fluid) mixture of spermatozoa and accessory sex gland secretions that provides the fluid in which spermatozoa are transported, provides nutrients, and neutralizes the acidity of the male urethra and female vagina
* contains antibiotic: seminal plasmin * contains prostatic enzymes that coagulate and then liquefy semen to aid in its movement through the uterine cervix |
|
|
Female organs of reproduction
|
ovaries (gonads), uterine (Fallopian) tubes, uterus, vagina, and vulva
|
|
|
Ovaries
- what cells do they produce and then discharge? - what hormones do they secrete? |
produce secondary oocytes, discharge secondary oocytes (ovulation)
secrete estrogens, progesterone, inhibin, and relaxin |
|
|
Oogenesis
|
Meiosis (46--> 23 and 23 --> 23 (egg) + 3 polar bodies w/ no cytoplasm)
reduction division (meiosis I), equatorial division (meiosis II), and maturation |
|
|
Uterine (fallopian) tubes
|
transport ova from ovaries to uterus and are the normal sites of fertilization
ciliated cells and peristaltic contractions help move a secondary oocyte towards the uterus |
|
|
Cervical Cancer
- What is the initial test - What is the most definitive test |
- pap smear
- biopsy |
|
|
Vulva
|
aka pudendum - refers to the external genitalia of the female
consists of: mons pubis, labia majora, labia minora, clitoris, vestibule, vaginal and urethral orifices, hymen, bulb of the vestibule, and the paraurethral (Skene's), greater vestibular (Bartholin's), and lesser vestibular glands |
|
|
Mammary glands
|
modified sudoriferous (sweat) glands that lie over the pectorals major and serratus anterior muscles
mammary gland development depends on estrogens and progesterone Essential function: lactation - secretion and ejection of milk |
|
|
Prolactin (PRL) and Oxytocin (OT)
|
PRL: milk secretion
OT: milk ejection, which is released from the posterior pituitary gland in response to suckling |
|
|
Risk factors associated with breast cancer
|
1. family history
2. never having a child, having a first child after 34 3. previous cancer in one breast 4. exposure to ionizing radiation such a x-rays 5. excessive fat and alcohol intake |
|
|
Treatment for breast cancer
|
1. hormone therapy
2. chemotherapy 3. radiation therapy 4. lumpectomy 5. modified or radical mastectomy (breast tissue/pectoral muscles/axillary lymph nodes) |
|
|
Female Reproductive Cycle
|
ovarian (maturation of an ovum) and uterine cycles (menstrual cycle - changes in the endometrium to prepare for the reception of a fertilized ovum
|
|
|
Hormonal Regulation
|
The menstrual and ovarian cycles are controlled by GnRH from the hypothalamus, which stimulates the release of FSH and LH by the anterior pituitary gland
FSH stimulates the initial development of ovarian follicles, ovulation, and the secretion of estrogens by the ovaries LH stimulates further development of ovarian follicles, ovulation, and the secretion of estrogens and progesterone by the ovaries |
|
|
Three man functions of estrogen
|
1. development and maintenance of female reproductive structures, secondary sex characteristics, and the breasts
2. regulation of fluid and electrolyte balance 3. stimulation of protein synthesis - why women have estrogen therapy after menopause |
|
|
How does birth control work?
|
By negative feedback mechanisms: moderate levels of estrogens in the blood inhibit the release of GnRH by the hypothalamus and secretion of LH and FSH by the anterior pituitary gland
No egg is descended to meet with sperm |
|
|
What is the purpose of progesterone
|
progesterone works with estrogens to prepare the endometrium for implantation and the mammary glands for milk synthesis
|
|
|
In the female reproductive cycle, what is the purpose of:
- inhibin - relaxin |
- inhibin: inhibits secretion of FSH and GnRH and, to a lesser extent, LH: it might be important in decreasing secretion of FSH and LH toward the end of the uterine cycle
- relaxin: relaxes the pubic symphysis and helps dilate the uterine cervix to facilitate delivery, and increases sperm motility |
|
|
Female reproductive cycle may be divided into three phases
|
Menstrual Phase aka menses or menstruation
Preovulatory phase aka proliferative phase Postovulatory phase |
|
|
Menstrual Phase
- what is it? - how long does it last (typically) - when does it start - what is the variance of follicles along phase |
stratum functionalis layer of endometrium is shed, discharging blood, tissue fluid, mucus, and epithelial cells
lasts roughly first 5 days of the cycle cycle starts = when bleeding starts early part - 20 to 25 primary follicles produce low levels of estrogens. toward the end (days 4/5), about 20 of the primary follicles develop into secondary follicles |
|
|
At birth, each ovary contains approximately how many primordial follicles?
- Each consists of ? |
200,000 primordial follicles in each ovary
- each consisting of a primary oocyte (potential ovum), surrounded by a single flattened layer of epithelial (follicular) cells |
|
|
Preovulatory Phase
- when is it (how long?) - dominant hormone - dominant GnRH (early and late) |
time between menstruation and ovulation - more variable in length than the other phases, lasting from days 6-13 (in a 28 day cycle)
endometrial repair occurs primary follicle --> secondary follicle (single secondary, someones more than one develops into a vesicular ovarian/graafian/mature follicle). Estrogen = dominant hormone in this phase early in this phase = FSH is dominant close to ovulation = LH secretion increases |
|
|
Ovulation
- what happens - when does it happen - what happens with hormones/GnRH |
rupture of the vesicular ovarian (Graafian) follicle with release of the secondary oocyte into the pelvic cavity
day 14 of 28-day cycle just before - high level of estrogens that developed during the latter part of preovulatory phase exerts --> positive feedback on both LH and GnRH --> LH surge |
|
|
Signs of ovulation
|
increased basal body temperature; clear, stretchy cervical mucus; changes in the uterine cervix; and ovarian pain
|
|
|
Directly following ovulation
|
the vesicular (Graafian) follicle collapses - blood forms within a clot --> corpus hemorrhagicum
clot is absorbed by remaining follicular cells under the influence of LH, follicular cells enlarge, change character, form --> corpus luteum (yellow body) * secretes estrogens and progesterone * performs the necessary tasks needed to ready the body for the placenta if the egg were fertilized (with secretions) - if not fertilized, the secretions will drop down and menstruation will occur |
|
|
Postovulatory Phase
- with reference to the uterus - with reference to the ovaries |
most constant in duration and lasts from days 15- 28, between ovulation and onset of next
- uterus: also called the secretory phase --> secretory activity of the endometrial glands as the endometrium thickens in anticipation of implantation - ovaries: also called luteal phase --> during which both estrogen and progesterone are secreted in large quantities by the corpus luteum |
|
|
If fertilization and implantation do not occur
|
the corpus luteum degenerates and becomes corpus albicans, or white body
The decreased secretion of progesterone and estrogens then initiates another menstrual phase (uterine and ovarian cycle) |
|
|
If fertilization and implantation do occur
|
the corpus luteum is maintained until the placenta takes over its hormone producing functions
during this time, the corpus luteum, maintained by human chorionic gonadotropin (hCG) from the developing placenta, secretes estrogens and progesterone to support pregnancy and breast development for lactation |
|
|
Four stages of human sexual response
|
arousal - parasympathetic impulses pass through the sacral region to cause vasoconstriction and secretion
plateau - "sexual flush" due to cutaneous vasodilation orgasm - sympathetic nervous stimulation of the whole body, in addition to rhythmic somatic and smooth muscle contractions resolution - occurs as the aroused systems relax |
|
|
Birth Control Methods
|
1. sterilization (vasectomy, tubal ligation)
2. hormonal (the pill, norplant - subcutaneous) 3. Intrauterine devices 4. Barriers (condom, vaginal pouch, diaphragm, cervical cap) 5. Chemical birth control (spermicides, contraceptive sponge) 6. physiological (rhythm, sympto-thermal) 7. induced abortion (RU 486, mifepristone) |
|
|
Gonads develop from what germ layer?
- external genitalia develop from what? |
intermediate mesoderm - differentiated into ovaries or testes by seventh week of fetal development
external genitalia develop from the genital tubercle |
|
|
Gonorrhea
- target areas of infection - men - women - babies - treatment |
aka The "clap"
affects primarily the mucus membrane of the urogenital tract, the rectum, and occasionally the eyes caused by: Neisseria gonorrhoeae males = inflammation of urethra with pus and painful urination females = urethra, vagina, and cervix, possible discharge of pus. HOWEVER often asymptomatic until advanced. --> pelvic inflammation could cause sterility and peritonitis newborn - possible blindness (administer silver nitrate) Treatment - penicillin or tetracycline in the past, more recently --> ceftriaxone since 1984 |
|
|
Syphilis
- bacteria - method of transmission - stages - treatment - diagnosis |
Treponema pallidum
sexual contact or placenta to fetus several stages: primary, secondary, latent, and tertiary treatment: antibiotics (usually penicillin) during all stages except tertiary Symptoms: do not always appear during first 2 stages - usually diagnosed through a blood test |
|
|
Genital Herpes
- treatment/cure - presentation - pregnancy |
Incurable at present time
genital blisters, high rate of recurrence of symptoms pregnant women: at time of delivery, c section usually will prevent complications --> asymptomatic infection to CNS damage to death |
|
|
Chlamydia
- bacteria - prevalence - men - women - pregnancy - treatment |
bacteria chlamydia trachomatis
most prevalent and most damaging STDs males = urethritis females = urethritis, can spread through reproductive tract and develop into inflammation of uterine (fallopian) tubes, which increases risk of ectopic pregnancy and sterility May be passed from mother to infant during childbirth, infecting eyes Treatment - tetracycline or doxycycline |
|
|
Trichomoniasis
- caused by - presentation - men - women |
Trichomonas Vaginalis - flagellated protozoan (one-celled animal)
women = causes an inflammation of the mucous membrane of the vagina in females men = causes an inflammation of the mucous membrane of the urethra in males |
|
|
Genital Warts
|
an infectious disease caused by human papilloma virus (HPV)
no cure treatment = cryotherapy with liquid nitrogen, electrocautery, excision, laser surgery, alpha interferon, and topical application of podophyillin in tincture of benzoin |
|
|
Testicular cancer
|
originates in sperm - producing cells
early sign is mass in testis most common in young men between the ages of 15-34 |
|
|
Conditions that affect the prostate gland
|
acute and prostatitis
benign prostatic hyperplasia (BPH) * size of the prostate gland increase 2-4 times larger than normal; this condition occurs in approximately 1/3 of all males over age 60 * corrected via transurethral resection of the prostate (TURP) * detection is usually possible by a digital rectal exam cancer * PSA = prostate specific antigen * prostatic acid phosphatase |
|
|
Impotence vs Infertility
|
Impotence = inability of an adult male to attain or hold an erection long enough for sexual intercourse
Infertility (male) = inability to fertilize a secondary oocyte. it does not imply impotence. * male fertility requires production of adequate quantities of viable, normal spermatozoa by the testes - analysis can be performed |
|
|
Menstrual abnormalities
|
Amenorrhea = absence of menstruation
Dysmenorrhea = painful menstruation abnormal uterine bleeding - changes in duration, amount, or frequency of flow Premenstrual syndrome (PMS) - severe physical and emotional distress in the late postovulatory phase often overlapping with the time of menstruation |
|
|
Toxic Shock Syndrome
|
widespread homeostatic imbalances and is a reaction to toxins produced by certain strains of bacteria
typically associated with tampon used |
|
|
Ovarian cysts
|
fluid containing sacs within ovary
|
|
|
Endometriosis
|
growth of endometrial tissue outside the uterus
tissue enters the pelvic cavity via the open uterine tubes and may be found in any of several sites --> ovaries, sigmoid colon, pelvic and abdominal lymph nodes, cervix, abdominal all, kidneys, urinary bladder common in women 25-40 who have not had children. symptoms include: premenstrual pain or unusual menstrual pain |

