![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
236 Cards in this Set
- Front
- Back
|
What is sexual reproduction? |
The process by which organisms produce offspring by making germ cells called gametes.
|
|
|
Gametes |
In males the germ cell is the sperm. In females it is the secondary oocyte. |
|
|
What produces gametes and secretes hormones? |
Males= gonads Females= ovaries |
|
|
Scrotum |
The supporting structure for the testes, consists of loose skin and an underlying subcutaneous layer that hangs from the root (attached portion) of the penis.
|
|
|
Raphe |
A median ridge of skin on the external pouch of scrotum that separates it into lateral portions. |
|
|
Scrotal septum |
Divides the scrotum into two sacs, each
containing a single testis. |
|
|
What is the scrotal septum made up of? |
A subcutaneous layer and muscle tissue called the dartos muscle, which is composed of
bundles of smooth muscle fibers. The dartos muscle is also found in the subcutaneous layer of the scrotum. |
|
|
Cremaster muscle |
A series of small bands of skeletal muscle that descend as an extension of the internal oblique muscle through the spermatic cord to surround the testes.
|
|
|
Where do the testes develop? |
Near the kidneys, in the posterior portion of the abdomen, and they usually begin their descent into the scrotum through the inguinal canals during the latter half of the seventh month of
fetal development. |
|
|
Tunica vaginalis
|
A serous membrane, which is derived from the peritoneum and forms during the descent of the testes, partially covers the testes.
|
|
|
Tunica albuginea
|
Internal to the tunica vaginalis is a white fibrous capsule composed of dense irregular connective tissue.It extends inward, forming septa that
divide the testis into a series of internal compartments called lobules. |
|
|
Seminiferous tubules
|
Each 200-300 lobules contains one to three of these tightly coiled tubules where sperm are produced. |
|
|
Spermatogenesis
|
The process by which the seminiferous tubules of the testes produce sperm.
|
|
|
What are the two types of cells found within the seminiferous tubules? |
Spermatogenic cells and Sertoli cells
|
|
|
Spermatogonia |
Remain dormant during childhood and actively begin producing sperm at puberty
|
|
|
Toward the lumen of the seminiferous tubule are layers of progressively more mature cells. What are they?
|
Primary spermatocytes, secondary
spermatocytes, spermatids, and sperm cells. |
|
|
What happens to spermatozoon after it has formed? |
After a sperm cell has formed, it is released into the lumen of the seminiferous tubules. |
|
|
Spermatogenesis |
Spermatogonium (stem cell)-->primary spermatocyte--> secondary spermatocyte--> spermatid-->spermatozoon (sperm). |
|
|
What does the blood-tests-barrier prevent? |
By isolating the developing gametes from the blood, it prevents an immune response against the spermatogenic cell's surface antigens, which are recognized as “foreign” by the immune
system. |
|
|
How do serotli cells support and protect developing spermatogenic cells? |
- They nourish sperm cells
- Phagocytize excess spermatid cytoplasm - Control movements of spermatogenic cells and the release of sperm into the lumen of the seminiferous tubule. - Produce fluid for sperm transport - Secrete the hormone inhibin, and regulate testosterone and FSH |
|
|
Leydig (interstitial) cells
|
These cells secrete testosterone, the most prevalent androgen.
|
|

|
Leydig cell |
|
|
Androgen
|
Is a hormone that promotes the development of masculine characteristics. Testosterone also promotes a man's libido (sexual drive).
|
|
|
Cryptorchidism
|
The condition in which the testes do not descend into the scrotum. Results in sterility because the cells involved in the initial stages of spermatogenesis are destroyed by the higher temperature of the pelvic cavity.
|
|
|
How many days does spermatogenesis take? |
65-75 |
|
|
Spermatogonia are types of stem cells that undergo what? |
Mitosis, some spermatogonia remain near the basement membrane of the seminiferous tubule in an undifferentiated state to serve as a
reservoir of cells for future cell division and subsequent sperm production. |
|
|
Diploid |
(2n)- that is, they have 46 chromosomes. i.e. spermatogonia & primary spermatocytes |
|
|
What are the events of spermatogenesis |
Mitosis, meiosis i, meiosis ii, spermiogenesis |
|
|
What happens during mitosis (males)? |
Some spermatogonia are pushed away from basement membrane (remember, some stay back). That spermatogonia (2n) differentiates and becomes a primary spermatocyte. |
|
|
What happens during meiosis I (males)? |
Primary spermatocyte replicates its DNA and forms two cells that become secondary spermatocytes.Each secondary spermatocyte has 23 chromosomes, the haploid number (n). Each chromosome within a secondary spermatocyte, however, is made up of two chromatids (two copies of the DNA) still attached by a centromere. |
|
|
What happens during meiosis II (males)? |
The chromosomes line up in single file along the metaphase plate, and the two chromatids of each chromosome separate. The four haploid cells resulting from meiosis II are called
spermatids (n). |
|
|
What are the four haploid cells resulting from meiosis II (males)? |
Spermatids (n).
|
|
|
What is the final stage of spermatogenesis? |
Spermiogenesis, is the development of haploid spermatids into sperm. No cell division occurs in spermiogenesis; each spermatid becomes a
single sperm cell. |
|
|
What is spermiation? |
When sperm are released from their connections to Sertoli cells. |
|
|
What enzymes are found in the acrosome? |
- Hyaluronidase
- Proteases |
|
|
What does the middle piece of the sperm tail contain? |
Mitochondria arranged in a spiral, which provide the energy (ATP) for locomotion of sperm to the site of fertilization and for sperm metabolism.
|
|
|
What hormones controls the testes? |
Gonadotropin‐releasing hormone (GnRH). This hormone in turn stimulates gonadotrophs in the anterior pituitary to increase their secretion of the two gonadotropins, luteinizing hormone and follicle‐stimulating hormone (FSH).
|
|
|
LH stimulates what (in males)? |
Leydig cells, which are located between seminiferous tubules, to secrete the hormone testosterone. This steroid hormone is synthesized from cholesterol in the testes and is the principal androgen. It is lipid‐soluble and readily diffuses out of Leydig cells into the interstitial fluid and then into blood.
|
|
|
What is DHT? |
In some target cells, such as those in the external genitals and prostate, the enzyme 5 alpha‐reductase converts testosterone to another
androgen called dihydrotestosterone. |
|
|
What does FSH do (in males)? |
Acts indirectly to stimulate spermatogenesis.
Together with testosterone, it acts synergistically on the Sertoli cells to stimulate secretion of androgen‐binding protein (ABP) into the lumen of the seminiferous tubules and into the interstitial fluid around the spermatogenic cells. |
|
|
What does ABP do? |
Binds to testosterone, keeping its concentration high. Testosterone stimulates the final steps of spermatogenesis in the seminiferous tubules.
|
|
|
What role does inhibin play (in males)? |
Once the degree of spermatogenesis required for male reproductive functions has been achieved, it is released by Sertoli cells. A protein hormone named for its role in inhibiting FSH
secretion by the anterior pituitary. |
|
|
What role does DHT play in prenatal development? |
Stimulates development of the external genitals.
|
|
|
How do sperm flow through the ducts of the testes? |
Pressure generated by the fluid secreted by Sertoli cells pushes sperm and fluid along the lumen of seminiferous tubules and then into straight tubules. The straight tubules lead to the rete testis . From the rete testis, sperm move into coiled efferent ducts in the
epididymis that empty into a single tube called the ductus epididymis. |
|
|
What happens at the distal end of the epididymis? |
The tail continues as the ductus (vas) deferens.
|
|
|
Stereocilia
|
Are long, branching microvilli (not cilia) that increase the surface area for the reabsorption of degenerated sperm.
|
|
|
Functionally, what does the epididymus do? |
Is the site of sperm maturation, the process by which sperm acquire motility and the ability to fertilize an ovum.
|
|
|
What happens to the epididymus during sex? |
Helps propel sperm into the ductus (vas) deferens during sexual arousal by peristaltic contraction of its smooth muscle.
|
|
|
What is the ampulla? |
The dilated terminal portion of the ductus
deferens. |
|
|
Spermatic cord
|
Is a supporting structure that ascends out of the scrotum. Consists of the ductus (vas) deferens, the testicular artery, veins that drain the testes and carry testosterone into circulation (the pampiniform plexus), autonomic nerves,
lymphatic vessels, and the cremaster muscle. |
|
|
Inguinal canal
|
An oblique passageway in the anterior abdominal wall just superior and parallel to the medial half of the inguinal ligament. Originates at the deep (abdominal) inguinal ring, a slitlike opening in the aponeurosis of the transversus abdominis muscle. Ends at the superficial (subcutaneous) inguinal ring a somewhat triangular opening in the aponeurosis of the external oblique muscle.
|
|
|
Varicocele
|
Refers to a swelling in the scrotum due to a dilation of the veins that drain the testes. It's like vericose veins in your balls.
|
|
|
Accessory sex glands (male)
|
Secrete most of the liquid portion of semen.
Include the seminal vesicles, the prostate, and the bulbourethral glands. |
|
|
Seminal vesicles
|
Seminal glands are convoluted pouch like structures. They secrete an alkaline, viscous fluid that contains fructose, prostaglandins, and clotting proteins. The alkaline nature of the seminal fluid helps to neutralize the acidic environment of the male urethra and female reproductive tract. The fructose is used for ATP production by sperm.
|
|
|
What do prostaglandins contribute?
|
Sperm motility and viability. Also may stimulate smooth muscle contractions within the
female reproductive tract. The clotting proteins help semen coagulate after ejaculation. Fluid secreted by the seminal vesicles normally constitutes about 60% of the volume of semen. |
|
|
Prostate
|
A doughnut‐shaped gland about the size of a golf ball. It is inferior to the urinary bladder and surrounds the prostatic urethra. The prostate slowly increases in size from birth to puberty. It then expands rapidly until about age 30, after which time its size typically remains stable until about age 45, when further enlargement may
occur. |
|
|
What does prostate secrete? |
A milky, slightly acidic fluid (pH about 6.5) that contains several substances.
|
|
|
What is contained in the milky substance secreted by the prostate? |
(1) Citric acid (2) Several proteolytic enzymes, such as prostate‐specific antigen (PSA)
(3) The function of the acid phosphatase secreted by the prostate is unknown. (4) Seminalplasmin. |
|
|
What does the citric acid in prostate secretion do? |
Is used by sperm for ATP production via the Krebs cycle.
|
|
|
What does the proteolytic enzymes, such as prostate‐specific antigen (PSA) do? |
Pepsinogen, lysozyme, amylase, and hyaluronidase, eventually break down the clotting proteins from the seminal vesicles.
|
|
|
What does seminalplasmin in prostatic fluid do? |
Is an antibiotic that can destroy bacteria. Seminalplasmin may help decrease the number of naturally occurring bacteria in semen and in the lower female reproductive tract.
|
|
|
Bulbourethral glands
|
Cowper's glands, are about the size of peas. They are located inferior to the prostate on either side of the membranous urethra within the deep muscles of the perineum, and their ducts open into the spongy urethra.
|
|
|
What do the Cowper's glands during sexual arousal? |
Secrete an alkaline fluid into the urethra that protects the passing sperm by neutralizing acids from urine in the urethra. They also secrete mucus that lubricates the end of the penis and the lining of the urethra, decreasing the number of sperm damaged during ejaculation.
|
|
|
Semen
|
A mixture of sperm and seminal fluid, a liquid that consists of the secretions of the seminiferous tubules, seminal vesicles, prostate, and bulbourethral glands.
|
|
|
The volume of semen? |
In a typical ejaculation is 2.5–5 milliliters (mL), with 50–150 million sperm per mL. When the number falls below 20 million/mL, the male is likely to be infertile.
|
|
|
What does seminal fluid do? |
Provides sperm with a transportation medium, nutrients, and protection from the hostile acidic environment of the male's urethra and the female's vagina.
|
|
|
Hemospermia
|
Presence of blood in semen-- in most cases, it is caused by inflammation of the blood vessels lining the seminal vesicles; it is usually treated with antibiotics.
|
|
|
Penis
|
Contains the urethra and is a passageway for the ejaculation of semen and the excretion of urine.
|
|
|
Body of the penis
|
Is composed of three cylindrical masses of tissue, each surrounded by fibrous tissue called the tunica albuginea.
|
|
|
Corpora cavernosa penis
|
Two dorsolateral masses.
|
|

|
Corpora cavernosa penis |
|
|
Corpus spongiosum penis
|
Contains the spongy urethra and keeps it open during ejaculation.
|
|

|
Corpus spongiosum penis |
|

|
Corona Glans Penis Prepuce (foreskin) External Urethra |
|
|
Priapism
|
Refers to a persistent and usually painful erection of the penis that does not involve sexual desire or excitement. The condition may last up to several hours and is accompanied by pain and tenderness. It results from abnormalities of blood vessels and nerves, usually in response to medication used to produce erections in males who otherwise cannot attain them.
|
|
|
Ejaculation
|
Is a sympathetic reflex coordinated by the
lumbar portion of the spinal cord. The smooth muscle sphincter at the base of the urinary bladder closes, preventing urine from being expelled during ejaculation. Peristaltic contractions in the epididymis, ductus (vas) deferens, seminal vesicles, ejaculatory ducts, and prostate propel semen into the spongy urethra. |
|
|
Emission
|
The discharge of a small volume of semen before ejaculation.
AKA- prejac |
|
|
Female reproductive system
|
Include the ovaries (female gonads); the uterine (fallopian) tubes, or oviducts; the uterus; the vagina; and external organs, which are
collectively called the vulva, or pudendum. The mammary glands are considered part of both the integumentary system and the female reproductive system. |
|
|
Ovaries
|
Are the female gonads, are paired glands that
resemble unshelled almonds in size and shape; they are homologous to the testes. (Here homologous means that two organs have the same embryonic origin.) |
|
|
What do the ovaries produce? |
(1) gametes, secondary oocytes that develop into mature ova (eggs) after fertilization, and (2)
hormones, including progesterone and estrogens (the female sex hormones), inhibin, and relaxin. |
|
|
Broad ligament
|
Part of the uterus, which is a fold of the parietal peritoneum, attaches to the ovaries by a
double‐layered fold of peritoneum called the mesovarium. |
|
|
Ovarian ligament
|
Anchors the ovaries to the uterus.
|
|
|
Suspensory ligament
|
Attaches ovaries to the pelvic wall.
|
|
|
Hilum
|
Hilus, the point of entrance and exit for blood vessels and nerves along which the mesovarium is attached.
|
|
|
What does each ovary consist of? |
Germinal epithelium, tunica albuginea, ovarian cortex, ovarian medulla, Ovarian follicles,
mature (graafian) follicle, and corpus luteum. |
|
|
Germinal epithelium
|
Is a layer of simple epithelium (low cuboidal or squamous) that covers the surface of the ovary.
|
|
|
Tunica albuginea
|
Is a whitish capsule of dense irregular connective tissue located immediately deep to the germinal epithelium.
|
|
|
Ovarian cortex
|
Is a region just deep to the tunica albuginea. It consists of ovarian follicles surrounded by dense irregular connective tissue that contains collagen fibers and fibroblast‐like cells called stromal cells.
|
|
|
Ovarian medulla
|
Is deep to the ovarian cortex. The border between the cortex and medulla is indistinct, but the medulla consists of more loosely arranged connective tissue and contains blood vessels, lymphatic vessels, and nerves.
|
|
|
Ovarian follicles
|
Are in the cortex and consist of oocytes in various stages of development, plus the cells surrounding them.When the surrounding cells form a single layer, they are called follicular cells; later in development, when they form several layers, they are referred to as granulosa cells.
|
|
|
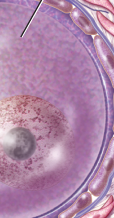
Mature (graafian) follicle
|
Is a large, fluid‐filled follicle that is ready to rupture and expel its secondary oocyte, a process known as ovulation.
|
|
|
Corpus luteum
|
Contains the remnants of a mature follicle after ovulation. The corpus luteum produces progesterone, estrogens, relaxin, and inhibin until it
degenerates into fibrous scar tissue called the corpus albicans. |
|

|
Primary follicle |
|

|
Secondary follicle |
|

|
Mature follicle |
|

|
Corpus luteum & blood clot |
|
|
Oogenesis
|
Formation of gametes in the ovaries. Begins in females before they are even born.
|
|
|
Oogonia
|
Are diploid (2n) stem cells that divide mitotically to produce millions of germ cells. Develop into larger cells called primary oocytes that enter prophase of meiosis I during fetal development but do not complete that phase until after
puberty. |
|
|
Primordial follicle
|
A primary oocyte is surrounded by a single layer of flat follicular cells.
|
|
|
How many primary oocytes will mature over a woman's life time? |
400 will mature and ovulate during a woman's reproductive lifetime. The remainder of the primary oocytes undergo atresia.
|
|
|
Primary ooctye |
|

|
Follicular cells |
|

|
Zona pellucida |
|

|
Stromal cells |
|

|
Primary oocyte |
|
|
What temperature do sperm require within the scrotum? |
2-3 degrees below body temperature. |
|
|
What is the sperm pathway? |
Seminiferous tubules, straight tubules, rete testis, epididymis, vas deferens, ejaculatory ducts, urethra.
|
|
|
What is contained within the spermatic chord? |
Testicular artery, a vein, nerves, lymphatic vessels and the vas deferens.
|
|
|
Where do seminal vesicles lie? |
Posterior to the base of the urinary bladder and anterior to the rectum.
|
|
|
What do seminal vesicles produce? |
An alkaline fluid containing fructose, prostaglandins, and clotting proteins.
|
|
|
What does the prostate surround? What does it secrete? |
The prostatic urethra and secretes a slightly acidic fluid containing citric acid and enzymes.
|
|
|
What do the bulbourethral glands secrete? |
An alkaline fluid into the urethra that protects sperm by neutralizing acids in urine.
|
|
|
In men, what functions in both the urinary and reproductive systems? |
Urethra |
|
|
The portion of the penis that surrounds the urethra is? |
The corpus spongiosum
|
|
|
The fructose in semen is secreted by |
The seminal vesicles
|
|
|
In males, FSH does? |
Acts indirectly with testosterone to stimulate spermatogenesis.
|
|
|
The cells in the testes responsible for producing testosterone are? |
Leydig cells
|
|
|
The testes are covered by a dense white fibrous capsule called the?
|
Tunica albuginea
|
|
|
Which of the following cells lies next to the
basement membrane of the seminiferous tubules? |
Spermatogonia
|
|
|
The cells formed by meiosis II are called?
|
Spermatids
|
|
|
The daily production of sperm in the testes is about?
|
300 million |
|
|
Which of the hormones produced in the male directly stimulates testosterone secretion?
|
LH |
|
|
In the male, the protein hormone inhibin is
produced by the _____ and inhibits secretion of _____. |
Sertoli cells; FSH
|
|
|
The longest duct of the male reproductive tract, passing from the scrotum into the pelvic cavity, is the?
|
Ductus deferens |
|
|
The ejaculatory duct attaches to the urethra in a region surrounded by the?
|
Prostate gland
|
|
|
The bulb of the penis is located at the base of the?
|
Corpus spongiosum
|
|
|
What holds the ovaries in position in the pelvic cavity? |
The broad, ovarian, and suspensory ligaments. |
|
|
The principle parts of the uterus are? |
The funds which is superior to uterine tubes, the body which is the central portion, and the cervix which opens into the vagina. |
|
|
What do the broad ligaments attach to? |
The uterus on either side of the pelvic cavity. |
|
|
Where do the uterosacral ligaments lie? |
On either side of the rectum and connect the uterus to the sacrum. |
|
|
The round ligaments |
Extend from the uterus to the labium majora. |
|
|
The perimetrium (female) |
Is composed of simple squamous epithelium and areolar tissue. |
|
|
The myometrium (female) |
Consists of three layers of smooth muscle. |
|
|
What is important to supporting regrowth of the stratum functionalism after menstruation? |
The extensive blood supply of the uterus. |
|
|
The mucosa of the vagina contains? |
Dendritic cells and large stores of glycogen which can break down to form organic acids which retard microbial growth. |
|
|
The muscularis (female) contains? |
An outer circular and inner longitudinal layer that allows stretch during sexual intercourse and childbirth. |
|
|
The mons pubis |
An elevation of adipose tissue covered by skin and hair that cushions the pubic symphysis. |
|
|
The labia majora |
Are homologous to the scrotum. |
|
|
The labia minora |
Are homologous to the spongy urethra and contain a large # of sebaceous glands. |
|
|
Each breast is? |
A mammary gland or modified sudoriferous gland that produces milk. |
|
|
Pathway of breast milk? |
Alveoli--> secondary tubules--> mammary ducts --> lactiferous sinuses--> lactiferous duct--> nipple. |
|
|
Portion of the ovary that contains the ovarian follicles? |
Cortex |
|
|
Which female reproductive structure is located between the urinary bladder and the rectum? |
Uterus |
|
|
The perimetrium or series is part of the? |
Visceral peritoneum |
|
|
In the ovary, oocytes begin meiosis I? |
During fetal development |
|
|
Infundibulum |
The open, funnel-shaped portion of a uterine tube. |
|
|
Fertilization of the oocyte by a sperm usually occurs in the? |
Ampulla of the oviduct |
|
|
Anteflexion |
The normal flexure of the uterus, projecting it anteriorly and superiorly over the vagina. |
|
|
The stratum basalis of the uterus? |
Repeatedly give rise to new stratum functionalism after each menstruation. |
|
|
The acidity of the vagina is due to? |
Breakdown of glycogen that produces organic acids. |
|
|
The milk secreting glands in the breast are called? |
Alveoli |
|
|
In which stage of meiosis is the secondary oocytes arrested unless fertilized? |
Meiosis II metaphase |
|
|
GnRH (females) does what? |
Is secreted by the hypothalamus and controls the ovarian and uterine cycles by stimulating release of FSH and LH. |
|
|
FSH (females) does what? |
Initiates follicular growth |
|
|
LH (females) does? |
Stimulates more development of ovarian follicles. Stimulates ovulation, corpus luteum formation and secretion of estrogen and progesterone by the corpus luteum. |
|
|
Inhibin (females) |
Secreted by the granulosa cells of the growing follicles and by the corpus luteum, inhibits secretion of FSH and LH. |
|
|
What happens during menstrual phase? |
FSH stimulates development of secondary follicles in the ovaries and prostaglandins cause loss of the stratum functionalis. |
|
|
What happens during the preovulatory phase? |
Secondary follicles start to secrete estrogens and inhibin. One becomes a dominant follicle and secretes estrogens and inhibin causing decreased FSH secretion leading to atresia of less developed follicles. In the uterus, the endometrium undergoes repair under the influence of estrogens. |
|
|
During ovulation what happens? |
Release of LH causes the release of the secondary oocyte. |
|
|
During postovulatory phase what happens? |
Progesterone and estrogens are secreted by the corpus luteum promoting the thickening of the endometrium preparing for implantation. If no pregnancy occurs, progesterone and estrogen levels drop and menstruation occurs. |
|
|
Corpus luteum secretes? |
Progesterone and estrogens |
|
|
Which hormones have the greatest direct control over the changes in the uterus? |
Estrogens and progesterone |
|
|
After ovulation the _____ becomes the _____.
|
Marutre (Graafian) follicle, corpus luteum |
|
|
The principal estrogen hormone in a non-pregnant woman is? |
Beta-estradiol |
|
|
Which hormone has effects on general metabolism to increase protein production and reduce cholesterol production as well as controlling the reproductive cycle in women? |
Estrogens. |
|
|
What increases the flexibility of the pubic symphysis at the end of pregnancy? |
Relaxin |
|
|
The mature (Graafin) follicle continues to enlarge and increase its estrogen production during what phase? |
Preovulatory phase |
|
|
What hormone does an over-the-counter ovulation test measure? |
LH |
|
|
Low levels of progesterone cause? |
Menstruation (hormone related) |
|
|
Which hormones are primarily responsible for ovulation? |
LH and estrogen (diagram). |
|
|
Which hormones maintain the uterine lining during the first trimester of pregnancy? |
Estrogen and progesterone (diagram) |
|
|
Oral contraceptives pills contain estrogens and progestins that? |
Inhibit the release of FSH and LH |
|
|
Sympto-thermal |
The birth control method that is based on knowledge of certain physiological changes that occur during the menstrual cycle. |
|
|
In males, what hormones stimulate development of gonads and external genitals? |
Testosterone and dihydrotestosterone. |
|
|
The epididymis and ductus deferent develop from the embryonic? |
Mesonephric duct |
|
|
Somatic cells are "diploid" what does that mean? |
Each cell nucleus contains two complete copies of the DNA that came into being in the zygote. |
|
|
Sex cell (gametes) are what? |
Haploid, meaning that each cell nucleus contains one copy of the DNA of the mother (somatic) cell. |
|
|
What happens when to gametes fuse to form the zygote? |
Each contributes its DNA to the new zygote, therefore making it diploid. |
|
|
How is meiosis different from mitosis? |
In mitosis, the mother cell is diploid, and both daughter cells are also diploid, each having one complete and identical copy of the mother cell's genome. Meiosis results in four haploid daughter cells and the four haploid genomes are all different. |
|
|
What is contained within an ovum? |
A haploid nucleus, ample cytoplasm, and all the organelles usually found in the somatic cell, all within a plasma membrane. |
|
|
What protects the zygote and pre-embryo until implantation? |
The zona pellucida- a glycoprotein membrane. |
|
|
What is oogenesis? |
The development of the ova. In humans begins in embryonic and fetal development with specialized somatic cells called "oogonia". |
|
|
What happens to oogonia? |
Some of these cells head down the path of meiosis, producing cells called "primary oocytes". However, this meiosis is suspended at the prophase I point until the female reaches puberty. |
|
|
What happens when the primary oocyte does undergo meiosis I? |
It produces two cells: - Secondary oocyte - First polar body |
|
|
What happens to the first polar body cells? |
Most of the primary oocyte's cytoplasm moves to the secondary oocyte. The first polar body undergoes meiosis II, and it's daughter cell degenerate. |
|
|
What happens to the secondary oocyte? |
It is the cell released from the ovary at ovulation. If it is not fertilized, it degenerates. |
|
|
What happens if the secondary oocyte is fertilized? |
The secondary oocyte immediately undergoes meiosis II, producing the ovum (plus a polar body that degenerates). |
|
|
What process is responsible for spermatogenesis? |
Specialized cells called spermatogonia divide by mitosis to produce another generation of spermatogonia. |
|
|
What are mature spermatogonia called? |
Primary spermatocytes. |
|
|
How do primary spermatocytes divide? |
By meiosis producing four haploid gametes. |
|
|
Pituitary gland secretes two gonadotropin hormones what are they? |
Follicle stimulating hormone and luteinizing hormone. |
|
|
FSH does what to men? |
Causes the testes to produce sperm |
|
|
FSH does what to women? |
Stimulates the growth of an ovarian follicle and the follicle cells to secrete estrogen |
|
|
What does the word "tropic" mean? |
To affect |
|
|
What does LH do to men? |
Causes the testes to secrete testosterone |
|
|
What does LH do to women? |
Causes ovulation and causes the follicle cells in the corpus luteum to secrete progesterone. |
|
|
GnRH stimulates what first? |
The hypothalamus that then stimulates the pituitary gland to release LH and FSH. |
|
|
FSH stimulates what in women? |
a) Growing follicles b) ovaries |
|
|
LH in women stimulates what? |
a) Ovulation b) corpus luteum |
|
|
What does corpus lutuem release? |
a) estrogens, b) progesterone, c) relaxin, d) inhibin |
|
|
Inhibits contractions of uterine smooth muscle. During labor, increases flexibility of pubic
symphysis and dilates uterine cervix. |
What is relaxin (female)? |
|
|
Inhibits release of FSH and, to a lesser extent, LH.
|
What is inhibin (female)? |
|
|
Works with estrogens to prepare endometrium for implantation. Prepares mammary glands to secrete milk. Inhibits release of GnRH and LH.
|
What is progesterone ? |
|
|
•Promote development and maintenance of
female reproductive structures, feminine secondary sex characteristics, and breasts. Increase protein anabolism. Lower blood cholesterol. Moderate levels inhibit releaseof GnRH, FSH, and LH. |
What is estrogen? |
|
|
Is the time between the end of menstruation and ovulation. Is more variable in length than the other phases and ac-counts for most of the differences in length of the cycle. It lasts from days 6 to 13 in a 28-day cycle.
|
What is the preovulatory phase? |
|
|
During preovulatory phase, by about day 6, a single secondary follicle in one of the two ovaries has out- grown all the others.
|
What is the dominant follicle? |
|
|
The one dominant secondary follicle becomes the_________________, which continues to enlarge until it is more than 20 mm in diameter and ready for ovulation
|
Mature (graafian) follicle |
|
|
The menstrual and preovulatory phases
together are termed the ___________________. |
Follicular phase |
|
|
Estrogens liberated into the blood by growing ovarian follicles stimulate the repair of the
endometrium; cells of the stratum basalis undergo mitosis and produce a new stratum functionalis. |
What is the proliferation phase? *Part of the preovulatory phase |
|
|
The rupture of the mature (graafian) follicle and the release of the secondary oocyte into the pelvic cavity, usually occurs on day 14 in a 28-day cycle.
|
What is ovulation? |
|
|
What is the first step that triggers ovulation? |
High levels of estrogens from almost mature
follicle stimulate release of more GnRH and LH. |
|
|
What is the second step involved with ovulation? |
GnRH promotes release of FSH and more LH.
|
|
|
The third step involved with ovulation? |
LH surge brings aboutovulation
|
|
|
Is the time between ovulation and onset of the next menses. In duration, it is the most constant part of the female reproductive cycle. It lasts for 14 days in a 28-day cycle, from day 15 to day 28.
|
What is the post ovulation phase? |
|
|
blood clot forms from minor bleeding of the ruptured follicle, the follicle becomes
the _____________________. |
Corpus hemorrhagicum *(happens in post ovulation phase) |
|
|
Theca interna cells mix with the granulosa cells as they all become transformed into _____________ cells under the influence of LH.
|
Corpus luteum *Post ovulation phase |
|
|
Post ovulation phase is also called? |
The luteal phase |
|
|
The cap over the distal end of the penis. |
What is the glans? |
|
|
From each primary spermatocyte, __________ sperm cell(s) is (are) produced; from each
primary oocyte, __________ secondary oocyte(s) is (are) produced. |
4, 1 |
|
|
Erectile columns that form the dorsal surface and sides of the penis.
|
What are the corpora cavernosa? |
|
|
__________ , which is secreted by the placenta, stimulates the synthesis and secretion of
testosterone before birth. |
HCG |
|
|
Testosterone has a negative feedback effect on? |
Not only on GnRH secretion, but also on FSH and LH secretion.
|
|
|
In the male, the process in which sperm cells, secretions of the prostate, and secretions of the seminal vesicles accumulate in the prostatic
urethra. |
What is emission? |
|
|
At birth, a girl has in her ovaries many __________ that have started meiosis but stopped at prophase I.
|
Primary oocytes |
|
|
A primary oocyte divides to produce a(n)?
|
Secondary oocyte and polar body |
|
|
The layer of clear, viscous fluid that is deposited around a primary oocyte.
|
What is the zona pellucida? |
|
|
he innermost cells of the cumulus mass.
|
What are the corona radiata? |
|
|
In the process of oogenesis, a polar body....
|
a) Is formed before fertilization and b) formed after fertilization |
|
|
The funnel-shaped end of the uterine tube
(fallopian tube). |
What is the infundibulum? |
|
|
The superior, domed portion of the vagina is called the?
|
Fornix
|
|
|
In the female, erectile tissue that corresponds to the corpus spongiosum in the male is the?
|
Bulb of the vestibule
|
|
|
During the menstrual cycle, the time between the ending of menses and ovulation is called the?
|
Follicular phase |
|
|
In the menstrual cycle, progesterone levels are highest during?
|
The secretory phase
|
|
|
A woman with a typical 28-day menstrual cycle is most likely to become pregnant from sexual
intercourse occurring on days? |
9-14 |
|
|
While the follicle is developing, a positive-
feedback loop occurs in which __________ stimulates the follicle, which increases the secretion of __________, which stimulates GnRH secretion. |
FSH, estrogen |
|
|
After fertilization, development of a full-term
fetus depends upon |
Release of HCG by the trophoblast to maintain the corpus luteum
|

