![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
Where are the baroreceptors and the chemoreceptors of the carotid artery?
|
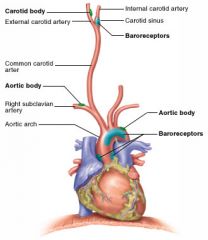
Baroreceptors - in the carotid sinus, a swelling at the base of the internal carotid
Chemoreceptors - in the carotid body, a small cluster of cells at the bifurcation of the carotid (into internal and external) |
|
|
How does the carotid artery get into the skull?
|
Leaves the neck via the carotid canal and enters the skull through the foramen lacerum
|
|
|
What do you do if there is an aneurysm in the middle cerebral artery? Why is it treatment done in this way?
|
Clamp the internal carotid to lower the amount of blood and thus the pressure in the MCA. To ensure pt has adequate collateral circulation you have to close the clamp gradually and watch for neurological deficits.
|
|
|
TIA's:
- 3 symptoms? - Major cause? Source of this cause (3) - Treatment? (3) |
Symptoms: sudden loss of vision, unilateral weakness, vertigo
Cause: emboli from heart, cardiac valves or carotids (esp. at bifurcations) Treatment: Endarterectomy, aspirin, anticoagulants |
|
|
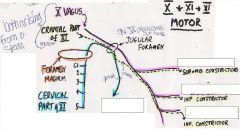
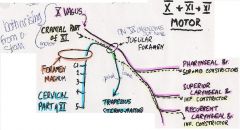
The Constrictor muscles extend from where to where? The top one is continuous with what other muscle?
|
Superior Middle and Inferior
From base of skull to esophagus Superior is continuous with the buccinator |
|
|
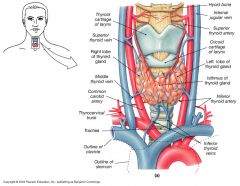
The thyroid receives blood from what? (2 arteries + their sources)
Which 3 veins drain the thyroid and what do they each drain into? |
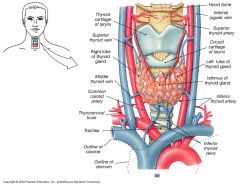
The superior thyroid arteries from the external carotids. Inferior thyroid arteries from subclavian arteries.
Superior and middle thyroid veins drain to internal jugular. Inferior thyroid vein drains to LBCephalic vein ** Some people have a Thyroidea IMA artery branching up from the aorta |
|
Name the branches of each of the following nerves
|
|
|
|
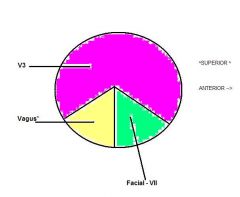
Which nerve supplies sensory information to each area:
- nasopharynx - oropharynx - laryngopharynx What supplies the glands in the area? |
- V2 (maxillary)
- Glossopharyngeal - Vagus The parasympathetics |
|
|
What would happen if a person got a hypogloassal nerve lesion? How would you tell if they instead had generalized neurodegeneration?
|
Atrophy of the tongue on one side.
Atrophy of the tongue on both sides |
|
|
When removing a tongue tumor, what tissues do you take out?
How would you compensate for this loss of tissue in the mouth? |
The tongue, a piece of the madible, the internal jugular and the sternocleidomastoid.
- Can replace with a flap of the pec major, a rib and some skin for the mouth |
|
|
What is the main action of the:
1. lateral pterygoid 2. medial pterygoid |
1. lateral - protrudes jaw & opens it at which point it is ++ vulnerable to dislocation
2. medial - mastication and sliding jaw from side to side |
|
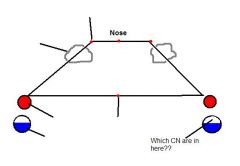
Identify the boundaries of the npharynx
|
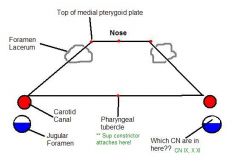
|
|
|
The npharynx will drain to which lymph nodes?
|
the deep cervical and the retropharyngeal nodes of rouviere
|
|
|
what could cause a horner's sydrome of the eye only (ie no skin involvement)
|
In the sympathetic nerve fibers of the carotid were involved
|
|
|
The palatine tonsil lays between which two muscles?
|
The palatoglossus and the palatopharyngeal
|
|
|
The tonsilar artery is a branch of _______ which is a branch of ________
|
Facial artery
external carotid |
|
|
If an infected tonsil is left on it's own what will happen?
|
The infection will spread to the soft palate forming an abscess known as a Quincy
|
|
|
Describe the flow of lymph in the tonsils, the adenoids, and soft palate
|
They all serve as origins of lymph vessels - none of them receive lymph but rather drain to the nodes in the head and neck
|
|
|
Explain the 80-20 rule about neck lumps?
|
In kids:
80% of neck lumps = bening 20% of neck lumps = malignant In adults: 80% of neck lumps = malignant 20% of neck lumps = bening |
|
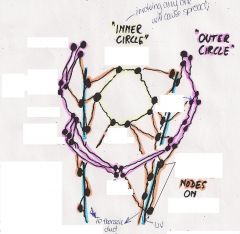
Label the lymph nodes of the inner and outer circles in the head and neck. Why are these nodes significant?
|
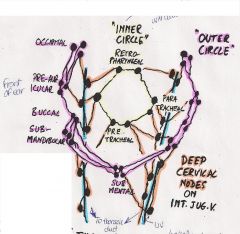
Involvement of any one node will cause spreading to the others! Lymph can flow in any direction!!
|
|
|
What procedure is the major cause of hoarseness? why (ie damage to what causes what)?
|
Thyroid surgery with subsequent damage to the recurrent laryngeal nerve.
Hoarseness typically occurs b/c the fibers that go to the posterior cricoarytenoid muscles lie along the periphery of the recurrent laryngeal. So if the nerve is man-handled these are the first to be damaged! |
|
|
If there's no external ear then there's no ________?
What type of tissues cover the external and middle ears? |
tympanic membrane
Skin, and mucous membrane (the secretions of which are drained by the eustation tube) |
|

Label the nerves that innervate each portion of the tympani membrane. Which nerve does the medial side?
|
The medial side is supplied by CN IX thus there are 4 CN in all!
* Stimulating the vagus can cause bradycardia and/or vomitting reflexes. |
|
|
How could you tell (with an otoscope) if someone had otitis externa?
|
The cone of light (usually anterior and inferior) would be reflected all over as the tympanic membrane would now be convex (bulging out)
|
|
|
What are 5 outside ear sources of an earache?
|
Sinusitis
TM joint - V3 Rotten teeth - V2,3 Tonsilitis - IX Ca of the tongue - IX V3 |
|
|
Give 3 reasons why children are prone to Otitis Media.
|
1. There is often a function obstruction of the E tube
2. The stiffness of the pharyngotympanic cartilage is insufficient 3. Tensor veli pallatini is inefficient before puberty Combined these will increase the chances that nasopharynx mucous is aspirated into the middle ear, and/or that middle ear secretions cannot get out. |
|
|
Which nerve controls a muscle that helps us accommodate for loud sounds. What does the muscle do?
Where is tensor tympani attached to? |
The facial nerve controls the stapedius muscle, which when contracted will rotate the stapes, thus decreasing it's ability to transmit sound.
T. Tympani - the handle of the malleus. |
|
|
What happens in otosclerosis? What are the symptoms and how is it treated?
|
When the stapes re-joins the petrous bone, thereby becoming immobilized and no longer able to transmit sound (ie person becomes deaf)
Can do a stapedectomy with prosthetic replacement. |
|
|
If a middle ear infection is chronic, the infection can spread to the surrounding ______ bone. If this happens the infection can now cause what 2 things? If it gains vascular access (most likely thru what?) it can cause what 2 other things?
|
Spreads to the petrous bone, and can cause meningitis or an extradural abscess. The abscess can get into the blood (via cavernous sinus?) and thus cause a cerebellar or temporal abscess.
To tx --> must remove petrous bone w/o removing the facial nerve. |
|
|
What are the 4 ganglia of the head and what does each contain?
|
Ciliary, pterygopalatine, submandibular and otic. Each has a branch of the trigeminal, a parasympathetic fiber from the B stem (that will synapse in the ganglia) and a postganglionic sympathetic fiber.
|
|
|
The thyroid gland develops as an endodermal downgrowth from which pharyngeal pouches?
The site from which it originates persists as the _____ ____ at the base of the tongue. |
2nd & 3rd
Foramen Cecum ** The path that the gland takes may result in thyroglossal remnants (cysts) or ectopic thyroid tissue |
|
|
Where does TSH come from?
|
Anterior pituitary
It stimulates both thyroid growth and the production & function of thyroid cells |
|
|
The thyroid isthmus is situated immediately cephaled/caudal to the cricoid cartilate?
|
Caudal! (Below)
|
|
|
In subacute thyroiditis.. what is the TSH? Radioactive Iodine uptake scan?
Explain? |
Low serum TSH and low uptake on the scan
The thyroid leaks T3/T4 which suppresses serum TSH and thus iodine uptake |
|
|
What is the TSH and RAI scan results in Graves disease? Explain
|
increased TSH - immunoglobulin levels that increase uptake on a scan despite low serum TSH levels
|
|
|
What are some causes of HYPER-thyroid?
(list the 2 most common first) |
1. Grave's disx (TSH Ig's)
2. Pummer disx (nodular toxic goiter) 3. amiodarone toxicity 4. TSH-secreting ant. pituitary tumors 5. hCG secreting tumors 6. Subacute thyroiditis 7. Cancer mets from thyroid |
|
|
What are the 3 treatment options for hyperthyroidism, how does each work and when are they used?
|
1. Antithyroid drugs:
Propylthiouracil (300-1000mg/day), prevents the binding of iodine. Good for pre-op, or for reliable pts with small goitres. Get less rebound hypothyroid and 30% will get remission of Graves with this. 2. Radioactive iodine: Can be given safely after the above. Great for old ppl (>40yo) and those who aren't good surgical candidates. Radiation will not increase risk of leukemia or congenital anomalies but will increase risk of benign thyroid tumors 3. SURGERY! Rapid disease control and less HYPO. Usually spare ~5gm of tissue; only do a total for pt's with Graves Ophthalmopathy Death <0.1% Recurrent Laryngeal nerve injury: < 2% |
|
|
What are some indications for surgical management of hyperthyroidism (6)?
|
1. Large or multinodular goiter
2. Current or desired pregnancy in 1yr 3. Ophthalmopathy 4. Amiodarone induced 5. Suspicion of malignancy 6. pts who would be unable to participate in long-term f/u |
|
|
Describe the three treatments for thyroid storm:
1. 2. 3. |
1. Lugol: to prevent the release of pre-formed thyroid hormone
2. Propanolol: to antagonize the peripheral effects of thyroid hormone 3. Propylthiouracil: decreases thyroid hormone production and extra-thyroidal conversion of T4 -->3 |

