![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
134 Cards in this Set
- Front
- Back
|
Clinical Anatomy of the Hepatobiliary System |
Clinical Anatomy of the Hepatobiliary System |
|
|
Liver - how many lobes and segments |
4 Lobes 2 anatomical · Left · Right (larger) 2 accessory · Quadrate
· Caudate |
|
|
What are the boundaries of callots triangle |
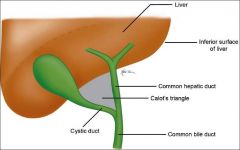
It is usually the right hepatic artery that is in danger during surgery and must be located before ligating the cystic artery. Contents: Lunds node + cycstic artery. Can also contain R. Hepatic artery and this is were complications can arise |
|
|
Path of bile from liver |
Bile canaliculi > Right and left hepatic duct > common hepatic duct (joins with cystic duct) > forms the common bile duct > Joins with pancreatic duct > enters into the duodenum through the hepatopancreatic ampulla |
|
|
Blocking the bile tree at different levels |
cystic duct : Gallblader inflammation + collic pain
Common hepatic: liver inflammation + jaundice
Common bile: the above two
Hepatopancratic ampula (narrowest part): pancretitis + all the above |
|
|
Consquences of pancreatic inflammation |
Jaundice (because the common bile duct passes through it)
Haemorrhage from erosions into the splenic artery and vein
thrombosis of the splenic vein SMV and portal veins |
|
|
Boundaries of the omental foramen |
Anteriorly: the hepatoduodenal ligament (free edge of lesser omentum), containing the hepatic portal vein, hepatic artery, and bile duct Posteriorly: the IVC and a muscular band, the right crus of the diaphragm, covered anteriorly with parietal peritoneum.(They are retroperitoneal.) Superiorly: the liver, covered with visceral peritoneum
Inferiorly: the superior or first part of the duodenum.
Leads into lesser sac |
|
|
Clinical significance of the boundaries of the omental foramen |
Although uncommon, a loop of small intestine may pass through the omental foramen into the omental bursa and be strangulated by the edges of the foramen. As none of the boundaries of the foramen can be incised because each contains blood vessels, the swollen intestine must be decompressed using a needle so it can be returned to the greater sac of the peritoneal cavity through the omental foramen. |
|
|
Clinical anatomy of the eye |
Clinical anatomy of the eye |
|
|
Damage to CNIII |
Eye lid drop (controls Levator palpebrae) Papillary reflex lost on side of lesion Eyeball movement disorders (eyeball will be turned lateral) |
|
|
Damage to CNIV |
Trochlear nerve Inability to look down when the eye is adducted |
|
|
Damage to CNVI |
Abducents nerve
Controls lateral rectus only |
|
|
What happens in horners syndrome |
Constriction of pupil (parasympathetic is unoppsoed) Anhydrosis Drooping superior eyelid Redness and increased temp of skin (vasodilation by parasympathetics) |
|
|
What is Argyll-Roberston pupil? |
Pupils that constrict when they accomodate but dont constrict to light.
Lesion to rostural midbrain which damages Edinger-Westphal nucleous but spares accomadation fibers which lie more ventrally.
Highly specific sign of neruosyphilis and maybe diabetic neuropathy |
|
|
Mechanism of papilledema |
Increased ICP leads to an increase in CSF presure in the extension of the subarachnoid space around the optic nerve. This causes the nerve fibers to buldge as cyotoplasm in the neruons pools.
Also decreased venous return from retina |
|
|
Muscles in blinking |
g |
|
|
Clinical anatomy of the breast |
Clinical anatomy of the breast |
|
|
Anatomical basis of clinical features of breast cancer |
Change in breast size/contours - mass effect of large tumour
Larger dimples - cancerous invasion of the glandular tissue and fibrosis which causes a tug on the suspensory ligaments, hence crfeating a dimple
Retraction of nipple - same as above
Skin changes - Lymphedema > Peau d'orange: puffy skin between dimpled pores (i.e hair pores) |
|
|
How does breast cancer spread ? |
1. Lymphatics: Axilla, Cervical, parasternal, Supraclavicular (and even abdoman)
2. Venous system: Posterior intercostals drain into azygos. these them communicate with the internal vertbral plexus surroudning the spinal cord. this is how breast cancer spreads directly to spinal vertabra and even CNS
3. Direct invasion |
|
|
Clinical anatomy of major vessels |
Clinical anatomy of major vessels |
|
|
Main ways arteries are damaged |
Stenosis Atherosclerosis Emoblism Infection Trauma |
|
|
Sites of arterial puncutre |
1. Radial 2. Brachial 3. Femoral 4. Dorsalis pedis |
|
|
Sites of venepuncture |
1. Median cubital 2. Cephalic 3. Basilic |
|
|
Mechanism of varicose veins |
2. Walls of the veins lose their elasticity and become weak. the vein dilates under the pressure of supporting a column of blood against gravity.
1.Imcompetent valves thus the column of blood ascending toward the heart is unbroken placing pressure on the weakend walls |
|
|
Clinical anatomy of the peritoneum |
Clinical anatomy of the peritoneum |
|
|
Greater Sac |
Cavity the is inside the peritoneum but outside of the lesser sac
Connected to the lesser sac via the omental foramen |
|
|
Lesser sac |
Formed by the lesser omentum. Behind the stomach and liver |
|
|
Mesentary |
Double layer of of visceral peritoneum
Most important on is the one that attaches the small intestine to the posterior wall |
|
|
Omentum |
Double layer of peritoneum that connects to either side of the tummy;
Greater Omentum - hangs down from the greater cuvature of the tummy like an aporon and comes back up and attaches to the transverse colon
Lesser Omentum - Lesser curvature of the tummy to the liver |
|
|
Congential abnormalities that result in intestinal obstruction |
Volvulus - Incorrect twisting of the gut
COngential bands - any of the left over things from the foetus that are supposed to go away can fibros and form bands that can trap the small intestine
Meckels diverticulum |
|
|
Charateristics of visceral pain |
Organs highly sensitive to stretch, ishcemia and inflammation Relativly insenstive to burring and cutting Diffuse and difficult to locate Can often be referred to other sites Can be accompanied by nausea and vomitting Described as sickening, deep, squeezing and dull |
|
|
Charaterisitcs of visceral pain |
Superfical structures and some deep structures such as muscles and ligamnets Responds well to temp and cutting Sharp and more intense Well defined and easy to locate
|
|
|
Paracentesis site |

Want to avoid epigastic arteries hence 1. 5cm below belly button 2. 3cm medial of ASIS then 3cm superior
|
|
|
Clinical anatomy of the brain and spinal cord |
Clinical anatomy of the brain and spinal cord |
|
|
What causes hydrocephalus ? |
Overproduction of CSF
Obstruction of CSF outflow - most common. occurs in bloackage to the cerebral aqueduct or in interventicular foramen
Interference with CSF absorbtion |
|
|
Aqueductal stenosis |
Aqueduct is narrowed. Caused by;
Tumor in midbrain Cellular debris following intraventricular hemorrhage Bacterial and fungal infections of the central nervous system. |
|
|
What are the two types of pain caused by a prolased disc? |
Localized back pain - results from presure on the longitudinal ligaments and from local inflamm caused by chemical irritation by siubstances from the ruptured nucleus pulposus
Chronic pain - Resulting fromcompression of the spinal nerve roots by the hernitated disc is usually referred pain, perceived as coming from the area (dermatome) supplied by that nerve. |
|
|
Which is the narrowest intervertebral foramen? |
the one between L5-sacrum.
Unfortuantly this one also has the largest nerve root and so is often a nerve that gets compressed. |
|
|
What is anaethetised with spinal anaesthesia? |
Injected into subarachnoid space at L3-L4. Produces comlete anaesthesia inferior to the waist. Sensation + motor are eliminated
Patient must stay inclinded as drug is heavier then CSF and hence sinks to the bottem of spinal cannal.
Hard/impossible to re-administer |
|
|
Caudal blocks |
delivered via indwelling catheter into the sacral canal. more can be delivered if needed
Areas anathetised: S2-S4 - Cervix, superior vagina, pudendal nerve. Entire birthcanal, pelvic floor and majority of perineum are anethestized but the lower limbs are not usually affected. |
|
|
Clinical anatomy of the thorax and medistinum |
Clinical anatomy of the thorax and medistinum |
|
|
What are the layers peirced for drainage of plueral effusions |
Skin SCT Muscle fascia External intercostals Internal intercostals Parietal pleura |
|
|
Where do you insert a needle in the ribs? |
Just above the superior border of the rib |
|
|
Which ribs are most commonly and lest commonly fraqctured? |
Less common = 1st rib
Most common = middle ribs
Weakest part of rib is just anterior to its angle |
|
|
Why is the apical section of lung more vulnerable to inhuries |
Because it is outside of the rib cage and sits in the supraclavular fossa |
|
|
Congential diaphragmatic hernia |
allways on the left due to the liver on the right.
one lung normally does not develop as a consquence |
|
|
Clinical anatomy of the ENT |
Clinical anatomy of the ENT |
|
|
spread of larynx cancer above and bloew the vocal folds |
Above - Superior deep cervicval lymph nodes
Below - Pretracheal or paratracheal lymph nodes which then drain into the inferior deep cervical lymph nodes |
|
|
5 arteries in Kiesselbach area |
Branch of sphenopalatine Posterior ethmoidal arteries anterior ethmoidal arteries Greater palatine artery Superior labial artery |
|
|
Why does the maxillary sinous get easily infected? |
the drinage orifice lies near the roof of the sinus and so the maxillary sinus does not drain well and infection develops more easily |
|
|
Piriform fossa |
depressions on either side of the larngeal inlet.
It is a mucus membrane and below it lies branches of the internal laryngeal nerve and recurrent laryngeal nerve.
Food can get caughty here and things like fish bones can peirce it and damage the nerves |
|
|
What does the superior laryngeal nerve supply ? |
Internal laryngeal nerve - Sensory to the mucosa External laryngeal nerve - Motor to cricothyroid |
|
|
Recurrent laryngeal nerve |
Motor to all the remaining internal muscles and sensation to the larynx below the vocal cords |
|
|
Unilateral damage of recurrent laryngeal nerve |
Hoarsness for a few weeks but then the other side compensates |
|
|
Bilateral damage of recurrent laryngeal nerve |
Loss of voice + stridor/respirotry distress |
|
|
damage to internal laryngeal nerve |
loss of senation and hence things can more easily enter the trachea |
|
|
damage to external laryngeal nerve |
paraylisis of cricothyroid hence unable to vary the length and tension of the vocal fold >>> loss of phonation. may not be noticed by normal people but would be critcal to a singer or public speaker. |
|
|
Clinical anatomy of the lower GIT |
CLinical anatomy of the lower GIT |
|
|
Explain the following types of feeding tubes Nasogastric Nasojejunal Gastric feeding Gastrojejunostomy Jejunostomy |
Nasogastric - nose to tummy. short term low invasive Nasojejunal - nose to jejunum. for those who cant tolerate food in tummy Gastric feeding - through wall of abdoman. people with high risk of aspiration Gastrojejunostomy - same as above but with another tube to jejunum. stomach can be drained while food is pumped Jejunostomy - through abdomin wall into jejunum |
|
|
4 main anastomoses of the portal system |
Esophageal Reactal Paraumbilical Intrahepatic |
|
|
Where will bleeding in the GIT cause haematemesis and melaena? |
above the pyloric sphincter.
anything below this will come out the rectum as bright red blood |
|
|
Pain pathway of Cholecystitis |
Refered to right scapula (c6 7 8) |
|
|
Pain pathway of Pancreatits |
Radiates to back (T6-T9) |
|
|
Pain pathway of Peptic ulcer |
back T6-9 |
|
|
Pain pathway of Peritonitis |
noramlly in epigastric but will follow the pathway the crap takes in the abodmen |
|
|
Common examples of refered pain |
Kidney - groin Diagphram - shoulder Gall bladder - scapula |
|
|
Where will cancer of the stomach and oesophagus spread to? |
1. Abdominal lymph nodes and then the Virchows node
2. Liver due to portal system |
|
|
Meckel's diverticulum |
reminant of the embryonic omphaloenteric duct (also known as the Vitelline duct)(normally connects embryonic mid gut to yolk sack).
In meckels the duck does not fully disappear and hence is present as a diverticulum of varying lenght
Postion - anterior ileum |
|
|
Layers that must be cut to enter the adbomin |
Skin SCT Fascia Rectus abdominus External oblique Internal oblique Transverse abdominus Transversalis fascia Endoabdominal (extraperitoneal) fat Peritoeum
Depending where you cut you can skip some of these (e.g. lateral cut will miss rectus abdominus) |
|
|
Structures that may be damaged in spleenectomy |
Splenic vein/artery Stomach Pancrease Colon |
|
|
What artery is damaged in a posterior duodenal ulcer |
Gastroduodenal artery (lies posterior to the 1st part of the duodenum |
|
|
Clinical anatomy of lower GIT |
Clinical anatomy of lower GIT |
|
|
Neural pathway of defecation |
Rectum fills > strech receptors activated > reflex generated > smooth muscle contracts + internal spincter relaxes (relfex inhibits sympathetic from L1 and L2) > still need volantary relax external anal spincter (via pudenal nerve S2-4) + can also increase intraabdominal pressure to help > defecation |
|
|
What can be viewed in proctoscopy |
Ancal cannal, anal cavity and rectum |
|
|
What can be viewed in Sigmoidoscopy |
Everything all the way up the the sigmoid colon |
|
|
What is palpated in a rectal examination? |
Anal sphincter Rectal wall and mucosa Enlarged interal iliac lymph nodes Pelvic surfaces of the sacrum and coccyx
Male - prostate and seminal glands
Females - Cervix (anterior to rectum) |
|
|
Above the pectinate line |
Lymph - Deep inginal Artery - Superior rectal (from SMA) Vein - Superior rectal (drains into IMV and then protal system) Nerve - Inferior hypogastric plexus (visceral) Epithelium - Columnar Embryological origon - Endoderm |
|
|
Below the pectinate line |
Lymph - Superfical inginal Artery - Middle and inferior rectal Vein - Middle and inferior rectal Nerve - Inferior rectal nerve (somatic) Epithelium - Stratified squamous Embryological origon - ectoderm |
|
|
Spread of colon cancer |
Venous - Portal system to liver
Lymph - Closest mesenteric node > deep nodes on the aorta > Virchows node > left thoracic duct > systemic circulation (most go to brain and lungs) |
|
|
Clinicval anatomy neurology |
Clinical anatomy neruology |
|
|
What is an extra dural bleed? |
Bleeding between skull bone and periostial dura.
Always caused by arterial blood > torn middle meningeal artery |
|
|
Layers peirced in a burr hole |
Only skin and skull (to expose the dura) |
|
|
What do you need to fracture to get CSF from nose |
Only cribiform plate > results in direct communication.
Also, if the the tympanic membrane has not ruptured but your middle cranial fossa has broken and you meninges close to the ear have torn it can travel down the eustachoian tube and down the nose |
|
|
CSF leak from ears |
Need to fracture base of skull (Middle cranial fossa)
+
Tear meninges close to the ear
+
Rupture Tympanic membrane |
|
|
5 main arteries of the scalp |
Supra-orbial Supratrochlear Superfical temporal Posterior auricular Occipital |
|
|
Layers repaired in suturing a sclap laceration |
Skin Connective tissue Aponeurosis (broad tendons of the muscles) Loose connective tisue |
|
|
Site of inferior alveolar nerve block |
Insert the needle into the tempro-mandibular depression at the level of the coronid notch. THis is just above where the nerve enters the mandible |
|
|
Why does it also numb the anterior 2/3rds of the tounge? |
Because corda tympani (a nerve) hitch hikes on the lingual nerve and supplies sensory to the anterior 2/3rds of the tounge |
|
|
Clinical anatomy of the upper limb |
Clinical anatomy of the upper limb |
|
|
What do the muscles (trapezius, SCM, pec major) do in a clavical fracture? |
Sternoceidomastoid elevates the medical fragment of bone. Trapezius is then unable to hold the other half of the clavical up due to the weight of the arm hence you get shoulder drop.
The pectoral muscles can also start to pull the lateral part of the clavical inwards hence shorten its length when it heals
Due to fall onto outstreched hand or direct blow to clavical |
|
|
What nerve can be damaged in a surgical neck of humerous fracture? |
Auxillary.
Normally an impact fracture as the person lands on their outstreched hand and the force is transmitted upward. |
|
|
Most common complication of shaft of humerous fractor |
radial nerve injury
Due to direct blow to arm,Heals well because of strong muscles and periostum holding bone ion place |
|
|
What nerve is in danger in a supracondylar fracture of the humerous ? |
Median nerve - if near supracondylar
Auxillary - if near medial epicondyl
Due to fall onto elbow |
|
|
Lower end of radius fracture |
Most common arm fracture due to trying to protect ones self from falling on an outstreched hand.
Heals well.
Possible complication: Swollen arm caugin carple tunnel syndrome |
|
|
Injury to superior parts of the brachial plexus (C5 and 6) |
Results from increased angle between the neck and shoulder.
Causes paralysis of deltoid, biceps and brachialis
Clinical appearance: Adducted shoulder, medially rotated arm, extended elbow. The lateral aspect of the forearm also expereinces some loss of sensation |
|
|
Injury to inferior parts of the brachial plexus (C8 and T1) |
Much less common.
Occurs when the upper limb is suddenly pulled superiorly - e.g. trying to grab something to break a fall.
The short muscles of the hand are affected and a claw hand results. |
|
|
Intramuscular injection into the deltoid site |
2.5-5cm below the acrominal process (usually 3 finger breadths) at 90 degrees. |
|
|
Where inject for digital nerve blook |
Basically, inject each side of the digit
Palmar side only - index and rude finger
Both sides - thumb, ring and little finger |
|
|
Clinical anatomy of the lower limb |
Clinical anatomy of the lower limb |
|
|
Shaft of femur fracture complications and cause |
Cause: Direct impact, MVA
Complication: High blood loss due to large compartment of thigh and laceration of profunda femoris |
|
|
What is the most commonly fractured tarsel bone |
2nd because it is the longest and narrowest and has its base wedged between the cuneiform bones
Cause: Repeditive micro trauma |
|
|
Mechanism and diagnosis of congenital dislocation of the hip; |
Occurs when the femoral head is not properly located in the acetabulum. It can be diagnosed if the patient is unable to abduct the thigh |
|
|
Signs and causes of posterioly disloacted head of femour |
Limb adducted, internally rotated, flexed at hip and knee with knee resting on opposite thigh |
|
|
Normal locking of the knee |
When the knee is fully extended with the foot on the ground, the knee passively locks because of medial rotation of the femoral condyles on the tibial plateau (the screw-home mechanism). this position makes the lower limb a solid column and more adapted for weight-bearing. When the knee is "locked" the leg muscles can relax. |
|
|
How does the knee unlock |
Popliteus contracts, rotating the femur laterally about 5 degree on the tibial plateau so that flexion of the knee can occur |
|
|
Function of medial and lateral archs of the foot |
spread ground contact reaction forces over a longer time period and thus reduce the risk of muscolokseletal wear or damage.
They also store energy of the above forces returning it at the next step and thus reducing the cost of walking and partitcualy running, where vertical forces are higher.
Like a spring |
|
|
WHat will happen to a person with low heel archs ? |
They will walk and run with their feet slightly everted where the foot can roll inwards. this makes them more susecptable to heel pain, arch pain and plantar fasciitis. |
|
|
What will happen to people who have high heel archs> |
walk more inverted and foot rolls outwards
Both high and low archs increase the risk of shin splints as the anterior tibialis must woek harder to keep the foot from slapping the ground |
|
|
Whats unique about cervical vertabra? |
Transverse foramen
Bifid spinous process |
|
|
Whats unique about thoracic vertabra? |
Costal facets
Long sloping transverse process |
|
|
Whats unique about lumber vertabra? |
Massive kidney shaped body
Short, broad blunt spinous process |
|
|
Whats unique about Atlas? |
C1
Has no body
Has foramen for dens |
|
|
Whats unique about cervical Axis? |
Dens |
|
|
Movements of shoulder |
Flexion/extension add/ab duction medial/lateral rotation circumduction |
|
|
Hip movments |
Medial/lateral rotation Flexion/extension add/ab duct |
|
|
Knee movements |
Flexion/extension
medial/lateral rotation |
|
|
spine movments |
Extension/flexion
right/left rotation
Left/right bending |
|
|
Blood supply of bones |
Nutriant atery (passes perpandicular through the periostium)
Metaphysial and epiphysial arteries that arise mainly from the arteries that supply the joints
Periosteal arteries - supply compact bone |
|
|
Why does bone infection become chronic? |
Pus spreads into the bones blood vessels, imparing their flow, and area of infect bone with reduced blood flow, known as sequestra, form the basis of a chronic infection |
|
|
Sites of infection |
Metaphyseal plates in children
In adults the metaphyseal vessels cross the epiphyeal plate and infection can cpread there |
|
|
CLinical anatomy of the inguinal region and male pelvis |
CLinical anatomy of the inguinal region and male pelvis |
|
|
Indirect hernia |
Occures because the processus vaginalis fails to close during infancy. The hernia travels in the spermatic cord hence it passes through both the superfical and deep inguinal rings |
|
|
direct hernia |
Bulge directly through the abdominal wall medial to the inferior epigastic artery |
|
|
Retractile testicle |
a testical that may move back and forth between the scrotum and the groin easily. caused by an overactive cremaster muscle |
|
|
Undescended testical |
Lies somewhere along its normal path of decent |
|
|
Ectopic testical |
A testicle that although not an undescended testicle, has taken a non-standard path through the body and ended up in an unusual location such as femoral canal, perineum ect |
|
|
Nerve supply of testes |
all from Testicular plexus of nerves that hitch hikes its way on the testicular artery; it carries > PNS from vagus > Sympathetic from T7 > Visceral sensory from T7 |
|
|
Lymphatic from Testes |
follows testicular artery and vein to Lumbar and preaortic lymph nodes |
|
|
Nerve supply of scrotum |
Anterior surface - Lumber plexus - genitofemoral nerve
Posterior and Inferior surfaces - Sacral plexus - Pudendal nerve |
|
|
Lymphatic drainage from scrotum |
Superfical inginual lymph nodes |
|
|
Bell-clapper deformity |
where the testis is inadequaetly affixed to the scrotum allowing it to move freely on its axis and susceptible to induced twisting of the cord and its vessels |
|
|
Layers peirced in draining of hydrocele |
Skin SCT Dartos muscle External spermatic fascia Cremaster muscle Cremaster fascia Internal spermatic fascia Tunica vaginalis |
|
|
Where are renal stones most likely to get logded |
1. Junction of the ureters and renal pelvis 2. Where the ureters cross the brim of the pelvis inlet 3. during their passage through the wall of the unrinary bladder |
|
|
Parts of the male urethra |
The vesicular part (in the bladder neck) The prostatic urethra The intermediate part (Membranous urethra) The spongy urethra |

