![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
487 Cards in this Set
- Front
- Back
|
Endocrine system deals with... |
-Slow and long term responses -maintenance of long term homeostasis |
|
|
What two systems have overlapping anatomy |
Endocrine and nervous system -the adrebal medulla is endocrine structure but activated via nervous system -hypothalamus is inside brain (nervous system) but is enodcrine structure |
|
|
In general what makes up the endocrine system |
All cells and tissues that secretr hormones |
|
|
Endocrine cells |
Grandular secretory cells that release hormones into interstitial fluids, lymphatic system, or blood stream |
|
|
Hormones |
-Chemical messangers that stimulate specific cells or tissues into action -regulate the metabolic operations of target cells |
|
|
What does the endocrine system release? |
Chemicals called hormones |
|
|
What produces hormones? |
Endocrine cells located in a gland or gland-like structure |
|
|
Endocrine system pathway of hormone |
-hormone enters blood stream -hormone travels to its target organ/tissue -hormone binds to specific target cells that have hormone receptors -hormone causes the targeted cell/tissue to respond |
|
|
Hormones can only trigger a reaction if... |
If the cell has the right receptors for the specific hormone |
|
|
Wide spread hormones |
Hormones that trigget receptors all throughout the body |
|
|
Localized hormones |
-trigger response in one area where receptors are located |
|
|
3 main classes of hormones |
-amino acid derivatives -peptide hormones -lipid derivatives |
|
|
Water soluble hormones fall under what class |
Amino acid derivatives |
|
|
Lipid soluble hormones fall under what class |
Iipid derivatives |
|
|
Peptide hormones |
-largest of the 3 main classes -water or lipid soluble -made up of chains of amino acids |
|
|
What do hormones do to cells? |
Alter activity of the cell by increasing or decreasing some of its functions to maintain homeostasis |
|
|
What is a hormone cascade? |
Hormones controlling other hormones which then lead to them controlling other hormones
*a hormone is released which triggers the release of another hormone which triggers the release of a 3rd hormone (and so on) *fight or flight* |
|
|
There are many organs with sencondary endocrine functions...such as |
The heart Thymus Digestive tract Adipose tissue Gonads Ovaries Kidneys |
|
|
What are Amino acid derivatives |
-small molecules similar to amino acids in structure |
|
|
What does increased glucose (hyperglycemia) do... |
-triggers pancreatic beta cells to release insulin -Insulin stimulates glycogenesis (turning glucose to glycogen) in liver and glucose uptake by cells
|
|
|
What does decreased glucose (hypoglycemia) do? |
-stimulates pancreatic alpha cells to release glucagon -glucagon triggers gluconeogenesis and glycogenolysis in liver and releases glucose into plasma |
|
|
Examples of amino acid derivatives |
-tyrosine derivatives -tryptophan derivatives |
|
|
Tyrosine derivatives |
-amino acid derivatives -thyroid hormones, catecholamines, epinephrine, norepinephrine, dopamine -released by adrenal medulla |
|
|
Tryptophan derivatives |
-amino acid derivatives -melatonin |
|
|
What releases melatonin |
The pineal gland |
|
|
Examples of peptide hormones |
-all hormones from the pituitary gland: growth hormone and thyroid stimulating hormone -insulin |
|
|
2 groups of lipid derivatives |
Eicosanoids Steroids |
|
|
What are Eicosanoids |
-derivative of arachidonic acids (fatty acid of cell membrane -associated with blood clotting -most cells release to coordinate function with neighboring cells |
|
|
What are Steroids |
-derived fron cholesterol |
|
|
Examples of steroids |
Estrogen, testosterone, and adrenal cortex hormones |
|
|
Most hormonal reponses rely on what type of feedback |
Negative feedback |
|
|
What is Negative feedback |
A response due to hormones downregulates hormone production (decrease hormone production) -maintains a set point |
|
|
What type of feedback response is rare? |
Positive feedback |
|
|
What is positive feedback |
-Response from hormone upregulates hormone production (increases it) -produces burst of response to rush completion |
|
|
Examples of positive feedback hormonal response |
-oxytocin for giving birth -luteinizing hormones for ovulation |
|
|
What is the hypothalamus to the endocrine system? |
Highest level of endocrine control |
|
|
What does the hypothalamus do in the endocrine system |
-integrates nervous and endocrine systems to help produce a coordinated response -controls anterior pituitary |
|
|
What 3 mechanisms does the hypothalamus use to combined the nervous and endocrine systems? |
-acts as endocrine organ -secretes regulatory hormones -contains autonomic nervous system centers |
|
|
Hypothalamus: acting as endocrine organ |
Releases antidiuretic hormones (ADH) and oxytocin (OXT) at posterior lobe of pituitary gland |
|
|
Hypothalamus: secretes regulatory hormones |
Controls activity of the anterior lone of the pituitary |
|
|
Hypothalamus: contains auntonomic nervous system centers |
Exerts control over the adrenal medulla |
|
|
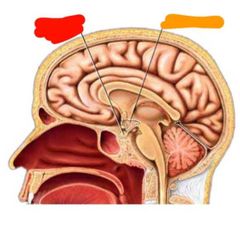
Red: pituitary gland Orange: hypothalamus |
|
|
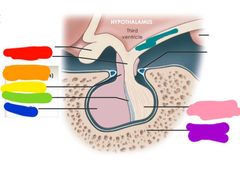
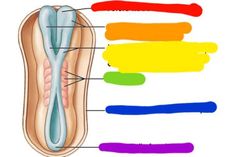
Red: infubdibulum Orange: anterior lobe (adenohypophysis) Yellow: pars tuberalis Green: pars intermedia Blue: pars distalis Purple: sella turcic of sphenoid Pink: posterior lobe (neurohypophysis) Teal: median eminence |
|
|
Whats the pituitary and where is it? |
-master gland or hypophysis -attached to hypothalamus via infundibulum -sits in hypophyseal fossa of sella turcica |
|
|
What are the two lobes of the pituitary gland |
-adenohypophysis (anterior lobe) -neurohypophysis (posterior lobe) |
|
|
How many hormones does the adenohypophysis lobe of the pituitary gland release |
7 peptide hormones |
|
|
How many hormones does the neurohypophysis of the pituitary gland release |
2 peptide hormones |
|
|
What makes up the anterior pituitary (adenohypophysis) |
-an extensive capillary network for releasing hormones |
|
|
What controls the anterior pituitary (adenohypophysis) |
Regulatory hormones secreted by the hypothalamus |
|
|
Pars distalis of the anterior pituitary (adenohypophysis) |
Secretes the majority of the hormones |
|
|
Pars intermedia of the anterior pituitary (adenohypophysis) |
Secretes melanocyte stimulating hormones |
|
|
Pars tuberalis of the anterior pituitary (adenohypophysis) |
Wraps around a portion of the infundibulum |
|
|
What hormones are released by the pars distalis of the anterior pituitary (adenohypophysis) |
-Thyroid stimulating hormone (TSH) -Adrenocorticotropic hormone (ACTH) -follicle stimulating hormone (FSH) -luteinizing hormone (LH) -prolactin (PRL) -growth hormone (GH) (somatotrpin) |
|
|
Hormones released by the pars intermedia of the anterior pituitary (adenohypophysis) |
Melanocyte stimulating hormone (MSH) |
|
|
What are the 5 cell types of the anterior pituitary (adenohypophysis) |
-thyrotropes -corticotropes -gonadotropes -lactotropes -somatotropes |
|
|
Thyrotropes |
anterior pituitary (adenohypophysis) cells that Release thyroid stimulating hormone (TSH) |
|
|
Corticotropes |
anterior pituitary (adenohypophysis) cells that release adrenocorticotropic hormone (ACTH) and melanocyte stimulating hormone (MSH) |
|
|
Gonadotropes |
anterior pituitary (adenohypophysis) cells that release follicle stimulating hormone (FSH) and luteinizing hormone (LH) |
|
|
Lactotropes |
anterior pituitary (adenohypophysis) cells that release prolactin (PRL) |
|
|
Somatotropes |
anterior pituitary (adenohypophysis) cells that release growth hormone (GH) also called somatotropi |
|
|
What innervates the posterior pituitary (neurohypophysis) |
- axons of the hypothalamic neurons |
|
|
The posterior pituitary (neurohypophysis) has no what |
Portal system |
|
|
What carries hormones out of the posterior pituitary (neurohypophysis) |
Hypophyseal veins |
|
|
What hormones are released by the posterior pituitary (neurohypophysis) |
Antidiuretic hormone (ADH) and oxytocin (OT) |
|
|
What is the hypophyseal portal system |
-system that distributes secretions to the adenohypophysis |
|
|
What are hypothalamic secretions |
-secretions released by the hypothalamus that are distributed to the adenohypophysis via the hypophyseal portal system -control hormones of adenohypophysis |
|
|
Primary plexus |
Plexus of capillaries found in the infundibulum thag connects the pituitary to the hypothalamus |
|
|
Pathway of hypothalamic secretions to the adenohypophysis |
-leave primary plexus -enter portal vessels -secretions arrive at secondary plexus |
|
|
Where is the secondary plexus |
Surrounding the 5 cell types of the adenohypophysis |
|
|
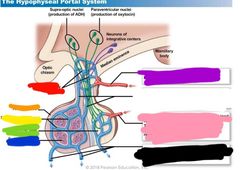
Red: primary plexus Orange: anterior lobe Yellow: secondary plexus Green: posterior lobe Blue: endocrine cells Purple: superior hypophyseal artery Pink: inferior hypophyseal artery Black: hypophyseal veins |
|
|
Thyroid stimulating hormone (TSH) targets |
The thyroid gland -stimulates production of T3 and T4 |
|
|
Adrenocorticotropic hormone (ACTH) targets |
The adrenal glands -stimulates glucocorticoid secretion |
|
|
Follicle stimulating hormone (FSH) targets |
The ovaries and nurse cells -stimulates estrogen secretion in females and sperm maturation in males |
|
|
Luteinizing hormone (LH) targets |
The testies and ovaries -stimulates ovulation, corpus luteum formation, and progesterone secretion |
|
|
Prolactin (PRL) targets |
The mammary glands -stimulates milk production |
|
|
Growth hormone (GH) targets |
The musculoskeletal system -stimulates growth, protein synthesis, lipid mobization, and catabolism |
|
|
Melanocyte stimulating hormone (MSH) targets |
Melanocytes -stimulates increased melanin production in epidermis |
|
|
Antidiuretic hormones (ADH) target |
The kidneys -promotes water reabsorption and elevation of blood volume and pressure |
|
|
Oxytocin (OXT) targets |
The uterus and mammary glands -causes labor contractions -and milk ejection Prostate and ductus deferens -contracts ductus deferens/prostate -and ejections of secretions |
|
|
Where is the thyroid located |
Anterior surface of the trachea and inferior to the larynx |
|
|
What is the thyroid made of.... |
2 lobes |
|
|
What connects the 2 lobes of the thyroid |
Thin isthmus connecting tissue |
|
|
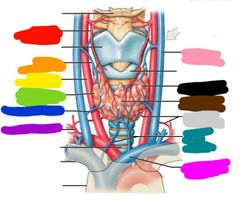
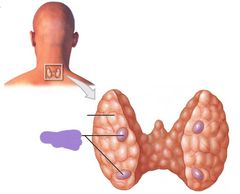
Red: superior thyroid artery Orange: superior thyroid vein Yellow: common carotid artery Green: right lobe of thyroid gland Blue: middle thyroid vein Purple: thyrocervical trunk Pink: internal jugular vein Black: left lobe of the thyroid gland Brown: isthmus of thyroid gland Gray: inferior thyroid artery Teal: inferior thyroid veins Hot pink: brachiocephalic vein |
|
|
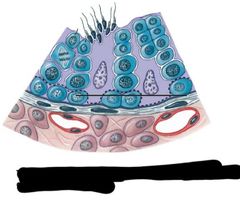
What do thyroid follicles do? |
Manufactures, stores, and secretes thyroid hormones |
|
|
What do C thyrocytes produce |
Calcitonin |
|
|
Functional unit of the thyroid is... |
The thyroid follicles |
|
|
Thyroid follicles are made of.. |
T thyrocytes Follicle cavity Colloid |
|
|
T thyrocytes |
-Line the follicle cavity of the thyroid follicle -they are simple cuboidal epithelium |
|
|
Follicle cavity of the thyroid follicle contain what |
Colloid (fluid) |
|
|
Where are C thyrocytes located |
In thyroid follicles inbetween T thyrocytes |
|
|
What surrounds each thyroid follicle? |
A capillary network |
|
|
What is the only endocrine gland that stores hormones externally? |
-thyroid (stores hormones extracellularly within the organ) |
|
|
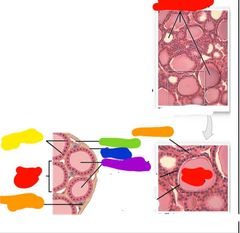
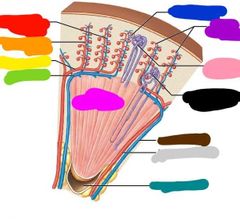
Red: thyroid follicle Orange: C thyrocyte Yellow: T thyrocyte Green: capillary Blue: capsule Purple: follicle cavity |
|
|
What are the 3 thyroid hormones |
T3 T4 calcitonin |
|
|
T3 does what |
Involved in metabolism -increases ATP use, O2 consumption, growth and development |
|
|
What does T4 do |
Involved in metabolism -increases ATP use, O2 consumption, growth and development |
|
|
What does calcitonin do? |
Decreases calcium ion concentration in bodily fluid. This helps with: -calcium uptake in bones during childhood -maintains bone mass in starvation -maintains bone mass in pregnancy |
|
|
What regulated thyroid secretion |
Anterior lobe of pituitary |
|
|
Parathyroid glands |
|
|
How many glands does the thyroid have and what are they called? |
4 Parathyroid glands |
|
|
Where are the parathyroid glands located |
On the posterior side of the thyroid gland |
|
|
What do the parathyroid glands produce? |
Parathyroid hormone |
|
|
What does parathyroid hormone do? |
-Increases Ca 2+ in the blood by reducing urinary excretion of calcium ions and stimulating the production of calcitriol in the kidneys -increases bone mass |
|
|
What does calcitriol do and where is it made |
-increases intestinal absorption of calcium ions -secreted by the kidneys |
|
|
Where is the thymus located |
Posterior to the sternum on the trachea -kinda sits in top of heart |
|
|
Talk about the thymuses size |
-it is large when you are young -shrinks after puberty |
|
|
Function of the thymus |
-mainly immune function -Maturation site for T cells
|
|
|
What does the thymus secrete |
Thymosin |
|
|
What is thymosin |
-a collection of hormones that aids in maturation of lymphocytes -secreted by the thymus |
|
|
T thyrocytes secrete |
T3 and T4 |
|
|
T3 and T4 target |
Most cells |
|
|
C thyrocytes secrete |
Calcitonin (CT) |
|
|
Calcitonin targets |
Bones and kidneys |
|
|
Parathyroid cells secrete |
Parathyroid hormone (PTH) |
|
|
Parathyroid homone targets |
Bones and kidneys |
|
|
Epithelial reticular cells secrete |
Thymosins |
|
|
Thymosins target |
Lymphocytes |
|
|
Adrenal glands are also called... |
Suprarenal glands |
|
This is the blood supply to what what glands? |
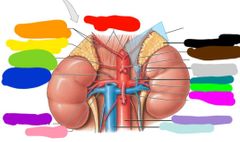
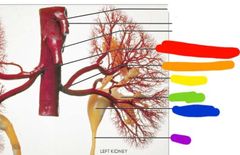
Adrenal glands Red: R/L inferior phrenic arteries Orange: right superior adrenal arteries Yellow: right adrenal gland Green: right middle adrenal artery Blue: right inferior adrenal artery Purple: right renal artery Pink: right renal vein Black: left adrenal gland Brown: left middle adrenal artery Gray: left inferior adrenal arteries Teal: left adrenal vein Lime green: left renal artery Hot pink: left renal vein Light purple: abdominal aorta Light blue: inferior vena cava |
|
|
What 2 parts make up the adrenal glands? |
Cortex and medulla |
|
|
How many hormones does the adrenal cortex produce? |
24+ -corticosteroids for metabolism |
|
|
What are the three parts of the adrenal cortex |
-zona glomerulosa -zona fasciculate -zona reticularis |
|
|
Whats the zona glomerulosa |
-outer most layer of adrenal cortex (15% of adrenal cortex) -makes: *mineralcoricoids that impact electrolyte composition *and aldosterone which conserves sodium and secretes potassium
|
|
|
What is the zona fasciculate |
-layer after the zona glomerulosa (80% of adrenal cortex) -makes: *glucocorticoids that impact glucose metabolism *and cortisol, cortisone, corticosterone which all speed up glucose/glycogen synthesis |
|
|
What is the zona reticularis |
-deepest zone of adrenal cortex -makes androgens |
|
|
Red: capsule Orange: cortex Yellow: medulla |
|

|
Red: zona glomerulosa Orange: zona fasciculate Yellow: zona reticularis Green: medulla |
|
|
What cells are inside the adrenal medulla |
Chromaffin cells |
|
|
What do chromaffin cells do |
They make catecholamines in the adrenal medulla -epinephrine (makes more of this) -norepinephrine |
|
|
What do catecholamines do? |
(This is epinephrine and norepinephrine) -they speed up use of energy and mobilization of energy reserves |
|
|
What cells are targeted by catecholamines |
Basically all cells -causes increase in cardiac activity -causes increased blood pressure -causes increase in glycogen breakdown -causes increase in muscular strength and endurance |
|
|
What is renin |
-An enzyme that converts angiotensin to angiotensin 1 and 2 -stimulates aldosterone (Made by kidney) |
|
|
What is erythropoietin |
A peptide hormone that stimulates erythrocyte production and is triggered by low O2 levels in the kidney (Made by kidney) |
|
|
What is calcitriol |
A steroid hormone that stimulates the absorption of calciun and phosphate along the digestive tract (Made by kidneys) |
|
|
What hormones are made by the kidneys |
Renin Erythropoietin Calcitriol |
|
|
What organd release opposing hormones to regulate blood pressure? |
The kidney and the heart |
|
|
What is atrial natriuretic peptide |
-A hormone released by the heart that is stimulated by high blood pressure/volume -opposes angiotensin 2 |
|
|
What does atrial natriuretic peptide do? |
-Inhibits renib, ADH, and aldosterone -increases water excretion in kidneys to decrease blood pressure/volume |
|
|
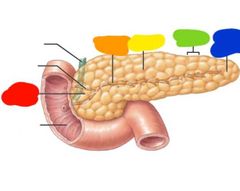
Pancreas Red: head Orange: pancreatic duct Yellow: body Green: lobule Blue: tail |
|
|
99 percent of the pancreas function is gastic...but 1 percent is what? |
Metabolic |
|
|
Where are the islets of langerhans located? |
In the pancreas |
|
|
What cells do the islets of langerhand contain |
Alpha cells and beta cells |
|
|
What do alpha cells produce in the islets if langerhans and what does it do |
-produces glucagon -which increases blood glucose through glycogen break down in the liver |
|
|
What do the beta cells in the islets of langerhans make and what does it do? |
-produces insulin -which decrease blood glucose by increasing cellular uptake and utilization -also signals storage |
|

|
Red: exocine cells Orange: islets of langerhans Yellow: alpha cells (glucagon) Green: beta cells (insulin) |
|
|
What is the male reproductive endocrine tissues |
Testes |
|
|
Interstitial cells in testes produce what |
Androgens |
|
|
What androgen do the testes produce |
Testosterone |
|
|
What does testosterone do |
-produces sperm -maintaibs secretory glands of male reproductive tract -responsible for secondary sex characteristics -stimulates skeletal muscle growth |
|
|
What is the female reproductive endocrine tissue |
Ovaries |
|
|
What hormones are produced by the ovaries |
Estrogen and progesterone |
|
|
What is the pineal gland |
-part of the epithalamus |
|
|
What does the pineal gland secrete |
Pinealocytes like melatonin |
|
|
What does the pineal gland control |
It releases melatonin which controls circadian rhythms |
|
|
When are the biggest changed in hormones as we age? |
-changes in hormones levels at puberty -decline in hormones during menopause |
|
|
Kidneys produce what |
Urine |
|
|
What structures are associated with the kidneys |
Nephrons |
|
|
What does the urinary tract do |
Transports and stores urine |
|
|
What structures are associated with the urinary tract |
Ureters Urinary bladder Urethra |
|
|
Where is urine stored until urination occurs |
The urinary bladder |
|
|
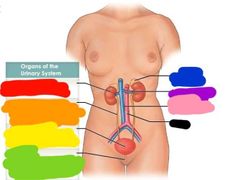
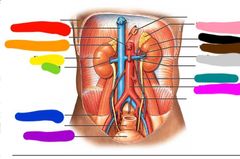
Red: kidney Orange: ureter Yellow: urinary bladder Green: urethra Blue: adrenal gland Purple: renal artery and vein Pink: inferior vena cava Black: aorta |
|
|
Functions of the urinary system |
-regulates plasma ion concentration -regulates blood volume and pressure (adjusts water loss in renin) -stabilizes blood pH -prevents loss of valuable nutrients -eliminates organic matter (nitrogeous waste) -synthesizes calcitriol (active vitamin D) -prevents dehydration -aids in liver function |
|
Are these organs retroperitoneal or peritoneal |
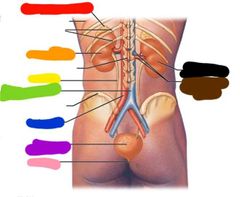
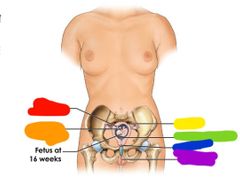
Retroperitoneal Red: adrenal gland Orange: left kidney Yellow: ureter Green: inferior vena cava Blue: aorta Purple: urinary bladder Pink: urethra Black: right kidney Brown: renal artery and vein |
|
|
What structures serve as renal support abd protection |
Fibrous capsule Perirenal/perinephric fat Renal fascia |
|
|
What does the renal fascia do |
Anchors kidneys to surrounding structures |
|
|
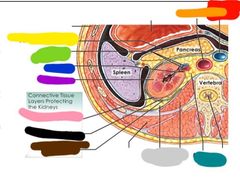
Red: inferior vena cava Orange: aorta Yellow: parietal peritoneum Green: renal vein and artery Blue: ureter Purple: left kidney Pink: fibrous capsule Black: perinephric fat Brown: renal fascia Gray: pararenal fat body Teal: adipose tissue |
|
|
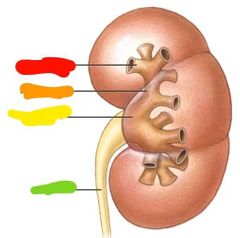
Red: minor calyx Orange: major calyx Yellow: renal pelvis Green: ureter |
|
|
What is a renal sinus |
-A cavity that holds renal pelvis and calyces |
|
|
What do renal sinuses do? |
Collect urine |
|
|
What are kidneys made of |
Arrangements of calyces and renal pelvis |
|
|
What goes through the renal hilum |
Ureter Artery Vein Nerve |
|

|
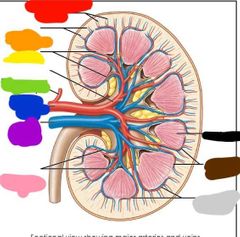
Red: cortex Orange: medulla Yellow: renal pyramid Green: connection to minor calyx Blue: minor calyx Purple: major calyx Pink: kidney lobe Black: renal columns Brown: outer layer of fibrous capsule Gray: ureter Teal: renal papilla Light blue: hilum Light green: renal pelvis Light purple: renal sinus Hot pink: inner layet of fibrous capsule |
|
|
The kidneys hold what percent of the bodies blood volume |
20% |
|
|
How much blood do the kidneys filter a day |
120-140 mL |
|
|
Blood enters the kidneys through |
The renal arteries |
|
|
Red: inferior vena cava Orange: right adrenal gland Yellow: right kidney Green: hilum Blue: peritoneum Purple: urinary bladder Pink: left adrenal gland Black: left kidney Brown: left renal artery Gray: left renal vein Teal: left ureter Hot pink: abdomibal aorta |
|
|
Describe blood flow through kidney |
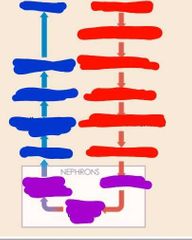
Renal artery Segmental arteries Interlobar arteries Arcuate arteries Cortical radiate arteries Afferent arteries *enter nephrons* Glomerulus Efferent arteriole Peritubular capillaries *left nephrons* Venules Cortical radiate veins Arcuate veins Interlobar veins Renal vein |
|
Starting from the red right column blood flow through kidney |
Renal artery Segmental arteries Interlobar arteries Arcuate arteries Cortical radiate arteries Afferent arterioles Glomerulus Efferent arteriole Peritubular capillaries Venules Cortical radiate veins Arcuate veins Interlobar veins Renal veins |
|
|
Red: cortical radiate veins Orange: cortical radiate arteries Yellow: interlobar arteries Green: segmental artery Blue: adrenal artery Purple: renal artery Pink: interlobar veins Black: medulla Brown: arcuate veins Gray: arcuate arteries |
|
|
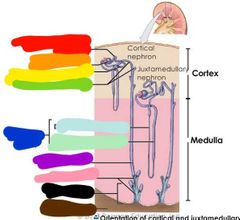
Red: cortical radiate veins Orange: cortical radiate arteries Yellow: arcuate artery Green: arcuate vein Blue: glomerulus Purple: afferent arterioles Pink: cortical nephrons Black: juxtamedullary nephron Brown: interlobar vein Gray: interlobaf artery Teal: minor calyx |
|
|
Red: right renal artery Orange: left renal artery Yellow: minor calyx Green: major calyx Blue: renal pelvis Purple: ureter |
|
|
What are nephrons |
-structural units of the kidneys that act as filtration and reabsorption apparatuses |
|
|
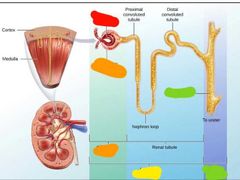
Red: proximal convoluted tubule Orange: renal corpuscle Yellow: distal convoluted tubule Green: connecting tubules Blue: nephron loop (descending thin limb and thick ascending limb) Purple: collecting duct Pink: papillary duct Black: renal papilla Brown: minor cortx |
|
|
Red: cortical nephron Blue: juxtamedullary nephron |
|
|
What is in the renal corpuscle |
The glomerulus |
|
|
What is the glomerulus? |
-Filtration site -afferent arteriole -efferent arteriole |
|
|
What is glomerular filtration |
Plasms is filtered across the walls of the glomerulus and into the capsular space |
|
|
How much blood flows through each kidney daily |
150L |
|
|
Renal corpuscles produce how much filtrate each |
95L |
|
|
How much filtrate produced by renal corpuscles is abosrbed by blood? |
2-3% |
|
|
Filtrate produced by the renal corpuscle is processed by what |
Tubules and collecting ducts to produce 1.5 L of urine |
|
|
Red: glomerulus Orange: glomerular capsule Yellow: nephron Green: collecting duct |
|
|
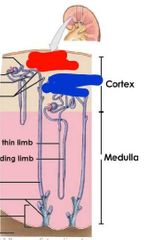
Right is: juxtamedullary nephron Left is: cortical nephron Red: efferent arteriole Orange: renal corpuscle Yellow: afferent arteriole Green: peritubulat capillaries Blue: glomerulus Purple: distal convoluted tubule Pink: collecting duct Black: peritubular capillaries Brown: nephron loop Gray: proximal convoluted tubule Teal: vasa recta |
|
|
Blood enters at where in a nephron |
Afferent arteriole |
|
|
Blood leaves where in a nephron |
Efferent arteriole |
|
|
What do nephrons regulate |
The concentration of water and solute in blood by: -filtering blood -reabsorbing soluted and water -and excreting waste |
|
|
Path of blood through a nephron |
Afferent arteriole Renal corpuscle Glomerulus Proximal convoluted tubule Nephron loop Distal convoluted tubule Collecting duct Out the body |
|
|
Renal corpuscle layers |
Endothelial surface layer Capillary endothelium Basement membrane Glomerular epithelium Subpodocyte space |
|
|
What does the endothelial surface layer of the renal corpuscle do |
Limits filtration of large plasma proteins |
|
|
What do the capillary endothelium of the renal corpuscle do |
Prevents filtration of red blood cells and allows soluted to filtrate |
|
|
What does the basement membrane of the renal corpuscle do |
Prevents large proteins from filtering while allows amino acids, glucose, and ions to filter |
|
|
What are the glomerular epithelium of the renal corpuscle and what do they do |
They are Filtrations slits that allow water with dissolved ions through |
|
|
What nephrons produce concentrated urine |
Juxtamedullary nephrons |
|
|
What are subpodcyte spaces of the renal corpuscle |
Filtration spaces |
|

|
Renal corpuscle Red: endothelial surface layer Orange: capillary endothelium Yellow: basement membrane Green: glomerular epithelium Blue: subpodocyte space |
|
|
What controls renal filtration |
Smooth musckle on the afferent/ efferent arterioles controls flow |
|
|
What is Bernoullis principle? |
-Small efferent arteriole = more pressure in glomersus which = more filtration -lare efferent arteriole = less pressure in glomerulus and less filtration |
|
|
Where does the efferent arteriole lead? |
The vasa recta also called the peritubular capillaries (this is a capillary bed) |
|
|
Components of the male and female repro system |
Gonads Reproductive tract Accessory glands External genitalia |
|
|
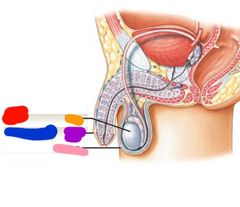
Red: gonads Orange: testis Blue: external genitalia Purple: penis Pink: scrotum |
|
|
What are the male gonads? |
The testes or testicles |
|
|
Location of testes |
Scrotum |
|
|
What happens to the tested during fetal development |
They descend from the abdominal cavity |
|
|
Function of the testes is... |
To produce sperm |
|
|
What does the gubernaculum testis do |
Anchors testes in place as body grows around it (does not elongate as fetus elongates) |
|
|
Describe the fetal descent of the testes |
-gubernaculum testis anchors testes to the babies body -the baby grows but the gubernaculum does not so the testes get pulled down -at 7 months of development gubernaculum testis muscle contract and pull testes through inguinal canal into scrotum |
|
|
What are the spermatic cords |
Layers of fascia and muscle that enclose everything that needs to travel between testes and rest of the body |
|
|
What make up the spermatic cords |
Nerves Arteries Veins Ducts |
|
|
Nerves of the spermatic cords |
Genitofemoral |
|
|
Arteries of the spermatic cords |
Deferential and testicular |
|
|
Veins of the spermatic cords |
Pampiniform plexus of testicular vein |
|
|
Ducts of the spermatic cords |
Ductus deferens |
|
|
What is located in the inguinal canal of males? |
Spermatic cords: Nerves Arteries Veins Ducts |
|
|
What is the scrotum |
-thin layer of skin and superficial fascia that holds the testes |
|
|
How many chambers does the scrotum have |
2 |
|
|
What divides the 2 halves or chambers of the scrotum |
Raphe |
|
|
What links the scrotal cavities (the 2 chambers of the scrotum) |
Tunica vaginalis |
|
|
What is the tunica vaginalis? Where is it located? What does it do? |
-serous membrane lining -lines the scrotal cavity -reduces friction |
|
|
What are the 2 muscles of the scrotum |
Dartos and cremaster |
|
|
What is Dartos and what does it do? |
-superficial scrotum muscle -gives the scrotum its resting tone and its wrinkly appearance |
|
|
What is the cremaster and what does it do? |
-deep scrotum muscle -tenses scrotum, pulls testes closer to body, responds to temperature and sexual arousal |
|
|
What covers the testes |
Tunica albuginea |
|
|
What is tunica albuginea? |
Fibrous connective tissue that is deep to the tunica vaginalis and lines the testes |
|
|
What partitions the testes internally |
Septa testis |
|
|
Where does the septa testis converge |
Mediastinum |
|
|
What occurs in the seminiferous tubules |
Sperm production |
|
|
What does the septa testis divide the tested into internally? |
Lobules |
|
|
Where do seminiferous tubules distribute sperm? |
Into the lobules of the testicles |
|
|
How long are the seminiferous tubules |
0.5 miles long coiled in each testicle |
|
|
What do the seminiferous tubules converge into |
Straight tubules Rete testis Efferent ductules Epididymis |
|
|
Describe the structure of the testes |
-seminiferous tubules surrounded by a capsule with loose connective tissue inbetween lobules -with blood vessels thrown in |
|
|
What interstitial endocrine cells make up the testes |
Leydig cells |
|
|
What do leydig cells produce? |
Androgens like testosterone |
|
|
What does the androgen testosterone do? |
-stimulates spermatogenesis -promotes the physical and functional maturation of sperm -maintains accessory organs of the male reproductive tract -causes development of secondary sexual characteristics -stimulates growth, metabolism, and muscle formation -influences brain development -sex drive -sexual development |
|
|
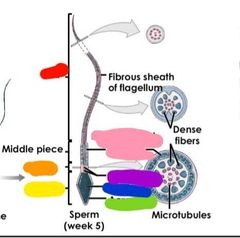
Steps of spermatogenesis |
Mitosis Meiosis I Meiosis II |
|
|
What stimulates spermatogenesis |
Testosterone |
|
|
What is spermatogenesis? |
The process of taking a stem cell and turning it into sperm |
|
|
What is spermiogenesis |
The process of maturing sperm |
|
|
During fetal development what stem cells are made |
Dormant spermatogonia |
|
|
What happens to spermatogenia during puberty? |
They begin to divide and continue to divide for the rest of the males life |
|
|
During mitosis of the spermarogenesis what happens |
-one spermatogonium splits into 2 -1 of these two stays a stem cell and the other becomes a primary spermatocyte (which moves onto meiosis) |
|
|
What 2 cells are formed during mitosis in spermatogenesis |
-stem cell -primary spermatocyte |
|
|
What happens during meiosis I of spermatogenesis |
-the primary spermatocyte duplicates genome (4N diploid) -dividing it into 2 secondary spermatocytes (2N)
|
|
|
What happens duing meiosis II of spermatogenesis |
-the secondary spermatocytes divide again to become spermatids (N) |
|
|
What happens after meiosis II of spermatogenesis? |
Spermiogenesis begins (spermatids mature) |
|
|
During spermiogenesis spermatids mature into |
Sperm |
|
|
How long does spermiogenesis take |
9 weeks for sperm to mature |
|
|
During spermiogenesis spermatids embed where? |
The cytoplasm of nurse cells (which are located as basal lamina) |
|
|
Where do sperm go once matured? |
They detach from nurse cells into lumen of seminiferous tubule |
|
|
What does the blood testis barrier do |
Separates stem cells from androgens and cells that are actively turning into mature sperm |
|
|
What is in the head of the sperm |
-densely packed with chromosomes -acrosome: compartment with enzymes for fertilization |
|
|
What is an Acrosome |
A compartment in the head of the sperm that contains enzymes for fertilization |
|
|
What does the neck of the sperm do |
-Attaches to the middle piece -centrioles |
|
|
Whats thr middle piece of the sperm contain? |
Mitochondria |
|
|
What is the tail of the sperm? |
Flagellum (only human cell with flagellum) |
|
|
Do sperm have energy reserves |
No |
|
|
What is the pathway sperm takes from testes to outside |
Testes Epididymis Ductus deferens Urethra *obtains bulking agents as it travels this pathway from accessory glands to create semen* |
|
|
What is the male reproductive tract |
Pathway from tests to outside body |
|
|
What is the epididymis |
Posterior border of testis |
|
|
Sperm in the epididymis are incapable of what... |
Movement or fertilization |
|
|
How long is the epididymis |
-7m long -coiled and twisted into 7cm of space |
|
|
What are the divisions of the epididymis |
Head Body Tail |
|
|
What does the head of the epididymis get |
-receives sperm from efferent ducts |
|
|
Where is the body of the epididymis |
Extends along posterior testis |
|
|
Describe the tail of the epididymus |
-less convoluted -stereocilia decline -tissue becomes similar to ductus deferens |
|
|
Whats the function of the epididymis |
-monitors and adjusts composition of fluid in seminiferous tubules -recycles damaged sperm through reabsorption -stores spermatozoa and facilitates functional maturation |
|
|
Whats going on with sperm leaving the epididymis? |
They are functionally mature but imobile |
|
|
What is capacitation |
The process by which sperm become fully mature and mobile |
|
|
When do sperm become mobile? |
When mixed with secretions from seminal glands |
|
|
When are sperm capable of fertilization |
When exposed to conditions inside the female reproductive tract |
|
|
What prevents premature capacitation in male reproductive tract |
Epididymis secretions |
|
|
How long is the ductus deferens |
40-50 cm |
|
|
Where does the ductus deferens go to and from |
From epididymis to urethra |
|
|
Where does the ductus deferens end |
Just before the prostaric urethra, at the ampulla |
|
|
What is the purpose of the ductus deferens |
-transports sperm -stores sperm for several months in semidormant state -joins with excretory duct from seminal gland to start ejaculatory duct |
|
|
Where does the urethra go and how long is it |
-from bladder to tip of penis -15-20 cm |
|
|
What are the three regions of the urethra |
Prostatic Membranous Spongy |
|
|
Where does the urethra feed into |
The ejaculatory duct |
|
|
What do accessory glands do |
-add fluid to sperm to make semen -actives sperm -provides bulk of semen -provides sperm with nutrients for mobility -producea buffer to counter act acidity of urethra and vagina |
|
|
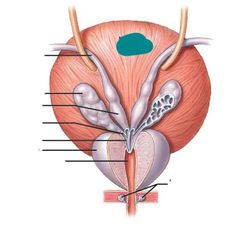
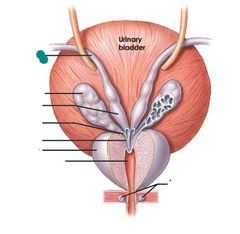
What are the accessory glands for the male reproductive system |
Seminal glands Prostate Bulbo-urethral glands |
|
|
Where are the seminal glands located |
Between the posterior bladder and anterior rectum |
|
|
How much of the semen volume do the seminal glands provide |
60% |
|
|
What componets do the seminal glands provide for the sperm in the semen |
-prostaglandins -clotting proteins -fructose |
|
|
When are the contents produced by the seminal glands introduced to sperm |
During ejaculation *allows sperm to be mobile* |
|
|
Where is the prostate located |
Encircles prostatic urethra |
|
|
What does the prosate produce |
Prostatic fluid |
|
|
What % of semens volume is prostativ fluid |
20-30% |
|
|
What are the components of the prostatic fluid |
-enzymes to prevent sperm coagulation -seminalplasmin: an antibiotic that prevents male urinary tract infections |
|
|
Where are the bulbo-urethral glands located |
Base of the penis |
|
|
Whats secreted by the bulbo-urethral glands and for why |
-alkaline that: -neutralizes urinary acids in urethra -and lubricates tip of penis (precome) |
|
|
How much semen is typically ejaculated |
2-5ml |
|
|
What is semen made of |
-20 million to 100 million sperm -seminal fluid: a mixture of secretions from accessory glands -enzymes: protease, seminalplasmin, fibrinolysin |
|
|
What is protease |
Enzyme in semen that helps dissolve mucus in the vagina |
|
|
What is seminalplasmin |
An enzyme in semen thats an antibiotic |
|
|
What is fibrinolysin |
-An enzyme in semen that liquifies clotted semen after 15-30 minutes -also helps increase sperm motility once in the female reproductive tract |
|
|
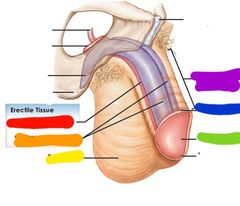
What are the parts of the weiner |
Root Body Glans Foreskin |
|
|
The penises erectile tissue is made of... |
3 parallel cylindrical columns |
|
|
What erectile tissue makes up the 3 parallel cylindrical columns |
Corpora cavernosa Corpus spongiosum |
|
|
What seperates the vascular channels of erectile tissue |
Elastic connective tissue and smooth muscle |
|
|
When the penis is at rest... |
Arteries are constricted and there is relatively little blood flow |
|
|
When the penis is erect... |
Arteries are dilated, blood flow increases, and erectile tissue is engorged |
|
|
2 steps of semen release |
Emission and ejaculation |
|
|
Emission |
-SNS coordinates peristatic contractions from ductus deferens through bulbourethral glands -these contractions mix the components of semen |
|
|
Ejaculation |
-rhythmic contractions originating in the pelvic floor muscles -which expels semen from penis |
|
|
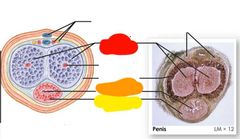
Red: corpora cavernosa Orange: spongy urethra Yellow: corpus spongiosum |
|
|
Red: corpus spongiosum Orange: corpora cavernosa |
|
|
Red: corpus spongiosum Orange: corpora cavernosa Yellow: scrotum Green: glans penis Blue: neck of glans Purple: body/shaft |
|
|
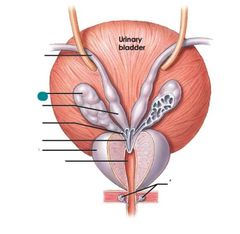
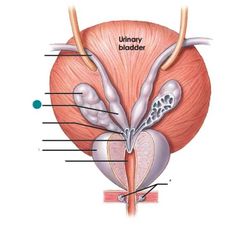
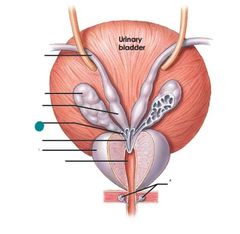
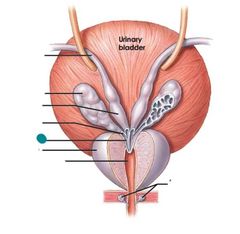
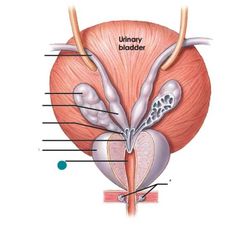
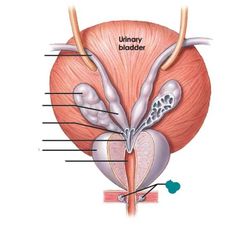
Urinary bladder |
|
|
Ductus deferens |
|
|
Seminal glands |
|
|
Ampulla of ductus deferens |
|
|
Excretory duct of seminal gland |
|
|
Ejaculatory duct prostate |
|
|
Prostatic urethra |
|
|
Bulbo-urethral glands |
|
|
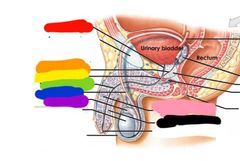
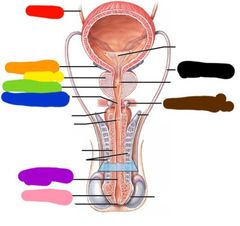
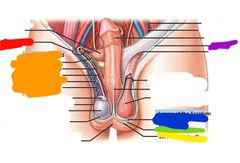
Red: prostatic urethra Orange: ejaculatory duct Yellow: membranous urethra Green: spongy urethra Blue: ductus deferens Purple: epididymis Pink: corpus cavernosum Black: corpus spongiosum |
|
|
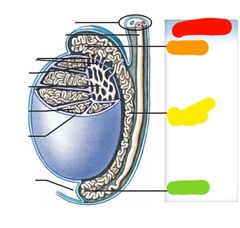
Red: Epididymis Orange: head Yellow: body Green: tail |
|
|
Red: spermatic cord Orange: ductus deferens Yellow: efferent ductules Green: seminiferous tubule Blue: tunica albuginea Purple: scrotal cavity |
|
|
Red: ureter Orange: seminal gland Yellow: prostate Green: protatic urethra Blue: membranous urethra Purple: spongy urethra (under this external urethral opening) Pink: glans penis Black: ductus deferens Brown: bulbo urethral gland |
|
|
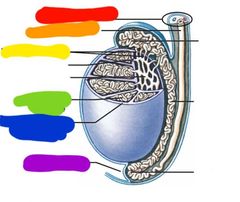
Red: tail Orange: neck Yellow: head Green: acrosome Blue: nucleus Purple: centrioles Pink: mitochondrial spiral |
|
The dotted line |
Blood testis barrier |
|
|
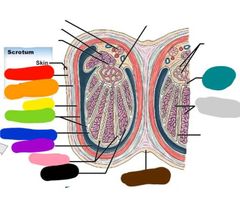
Red: dartos muscle Orange: superficial scrotal fascia Yellow: cresmaster Green: tunica vaginalis Blue: tunica albuginea Purple: scrotal cavity Pink: septa testis Black: lobule Brown: raphe Gray: seminiferous tubules Teal: straight tubules |
|

|
Red: epididymis Orange: scrotal cavity Yellow: testis Green: tunica vaginalis Blue: raphe Purple: spermatic cord Pink: scrotal septum Black: cremaster |
|
|
Red: inguinal canal Orange: spermatic cord Yellow: scrotal skin Green: dartos muscle Blue: superficial scrotal fascia Purple: inguinal |
|
|
Female gonads are... |
Ovaries |
|
|
Components of the female reproductive tract are... |
Uterine tubes Uterus Vagina |
|
|
External genitalia of the female reproductive system |
Vulva |
|
|
What do the ovaries do? |
Produce oocytes and secretes hormones |
|
|
Do ovaries have a peritoneal covering |
No |
|
|
What are the layers of the ovaries |
Germinal epithelium Tunica albuginea Stroma |
|
|
What cells make up the germinal epithelium layer of the ovaries |
Simple cuboidal epithelium |
|
|
What makes up the tunica albuginea layer of the ovaries |
Dense connective tissue |
|
|
What makes up the stroma layer of the ovaries |
Cortex (gametes) And medulla |
|
|
What are the cycles of the female reproductive system |
Oogenesis Ovarian cycle Uterine cycle |
|
|
What happens during oogenesis |
Oocytes are produced |
|
|
What is the ovarian cycle |
The monthly process of maturing an oocyte |
|
|
What is the uterine cycle |
The Monthly process of preparing the uterus for implantation of a fertilized oocyte |
|
|
When does oogenesis begin |
Before birth |
|
|
What is made during oogenesis |
Reproductive stem cells oogonia becomes primary oocytes (4N) *happens in mitosis* |
|
|
Steps of oogenesis |
Mitosis Meiosis I Meiosis II |
|
|
Monthly what happens to oocytes |
1 primary oocyte develops for ovulation becomes secondary oocyte (2N) and polar bodies *happens in meiosis I* |
|
|
What happens after fertilization in oogenesis |
-Secondary oocyte finishes meiosis II -mature ovum formed and along with polar bodies |
|
|
Primordial follicle is... |
Primary oocyte plus the follicle cells |
|
|
Each oocyte is surrounded by |
A simple squamous layer of follicle cells |
|
|
Primary oocytes rest in what? |
Egg nests |
|
|
As a oocyte becomed a primary follicle what do follicular cells do |
-they become cuboidal and divide -several follicular layers form granulosa cells which feed oocyte |
|
|
What does the oocyte make to protect its self |
Zona pellucida |
|
|
What layer do ovarian stromal cells form |
Thecal cells |
|
|
Thecal cells plus granuloda cells make what |
Estrogens (mainly estradiol) |
|
|
Many _ become primary follicles |
Primordial follicles |
|
|
Only a few _ become secondary follicles |
Primary follicles |
|
|
Why do only a few primary ovarian follicles become secondary? |
Because we only have usually 1 baby at a time...no litters...we dont want more then 1 egg to get fertilized |
|
|
What happens to secondary ovarian follicles |
Follicle wall begins to thicken |
|
|
How long does tertiary follicle formation take |
2-3 months |
|
|
What happens to tertiary follicle? |
Deep follicular cells secrete fluid which accumulates in follicle making the antrum |
|
|
Whats the antrum? |
Fluid filled space in a tertiary follicle |
|
|
Whats the corona radiata |
-A mass of granulosa cells that stay with oocyte for protection -what the sperm has to work through |
|
|
How many secondary follicles do you make per cycle and how many do u ovulate |
-20 -1 |
|
|
What is atresia |
Breakdown of a follicle that did not ovulate |
|
|
During ovulation what happens? |
The tertiary follicle releases the secondary oocyte and its corona radiata by literally exploding out of the ovary |
|
|
What moves the oocyte into the uterine tube |
Fimbrae |
|
|
Once the secondary oocyte and its corona radiata are expelled what happens in the ovary? |
The ovulated follicle forms a corpus luteum in the ovary |
|
|
How does the corpus luteum form? |
-The tertiary follicle collapses after shooting out secondary oocyte and its corona radiata -remaining granulosa cells invade the tertiary follicle |
|
|
What does the corpus luteum do? |
Makes estrogen and progesterone |
|
|
When does the corpus luteum break down |
12 days after ovulation unless fertilization occurs |
|
|
When the corpus luteum breaks down what happens? |
-Progesterone and estrogen levels drop triggering the release of GnRH -fibroblasts invade producing a knot of scar tissue called the corpus albicans |
|
|
Whats the corpus albicans |
A knot of scar tissue that forms in place of corpus luteums after ovulation |
|
|
What are uterine tubes |
13 cm long hollow muscular tubes |
|
|
What are the parts of the uterine tubes |
Fimbriae Infundibulum Ampulla Isthmus Uterine part |
|
|
What is the fimbriae |
Part of the uterine tube -fringe projection that drapes over ovary |
|
|
What is the infundibulum |
Part of the uterine tube -expanded funnel |
|
|
What is the ampulla |
Middle region of the uterine tube |
|
|
Whats the isthmus |
Part of the uterine tube that connects the ampulla to the uterus |
|
|
What is the uterus part |
Part of the uterine tube that opens into the uterine cavity |
|
|
What make up the uterine tube |
-Ciliated and unciliated columnar epithelium -smooth muscle muscularis |
|
|
What is ovum transport |
Peristalsis and cilia |
|
|
How long does it take to move the secondary oocyte from infundibulum to uterine cavity |
3-4 days |
|
|
Where does ovulation usually occur |
The ampulla |
|
|
What needs to happen in order for fertilization to occur? |
Sperm must meet egg within 12-24 hrs of ovulation |
|
|
What is the uterus |
-pear shaped organ -3 inches long and 2 inches wide and bends anterior at base |
|
|
Where does the uterus lie |
Posterior and superior bladder |
|
|
Whats the gross anatomy of the uterus |
Body Fundus Isthmus Cervix |
|
|
What does the mucus lining of the internal os do |
-Helps prevent bacterial invasion of uterus -thins around time of ovulation to facilitate sperm entrance
|
|
|
The cervix is made of the... |
Internal and external os |
|
|
What ligaments hold the uterus in place |
Suspensory ligaments: broad and round |
|
|
What supplies blood to the uterus |
Branches of the uterine artery/vein and branches of the ovarian artery |
|
|
Layers of the uterine wall |
Perimetrium Myometrium Endometrium |
|
|
What is the perimetrium |
Outer serous layer of the uterine wall |
|
|
What makes uo the myometrium of the uterine wall |
Muscles 1 circular 2 longitudinal |
|
|
What is the endometrium |
The inner lining of the uterine wall |
|
|
What is the function of the endometrium functional layer |
To Change over the course of the uterine cycle |
|
|
Endometrium layers |
Basal and functional |
|
|
What is the function of the basal layer of the endometrium |
Connects endometrium and myometrium |
|
|
What supplies blood to the endometrium |
Uterine artery Arcuate artery Radial artery Straight and spiral arteries |
|
|
What supplies the basal layer of the endometrium with blood |
Straight arteries |
|
|
What feeds the functional layer of the endometrium blood |
Spiral arteries |
|
|
What is the menstrual phase of the uterine cycle |
The degeneration of the functional layer of the endometrium |
|
|
What happens during the menstrual phase |
- spiral arteries constrict and restrict blood flow -secretory glands and tissues of functional layer die -weekend arterial walls rupture causing blood to fill connective tissue of functional layer -all this bad joo joo exits the uterus via cervix -1 to 7 days |
|
|
Whag triggers the menstrual phase of the uterine cycle |
The drop in progestin and estrogen that occurs because of the death of the corpus luteum |
|
|
What is the proliferatice phase of the uterine cycle? |
-The uterus being restored after the menstrual phase -estrogen rises -epithelial cells in basal layer proliferate -functional layer restored -by ovulation functional layer is several mm thick and highly vascularized |
|
|
What is the secondary phase of the uterine cycle |
-when uterus is at its best -endometrial glands enlarge and increase secretion (high estrogen from corpus luteum) |
|
|
When does the secondary phase of the uterine cycle occur |
-At the beginning of ovulation -peaks 12 days after ovulation -if embryo implants it continues because estrogen stays high -if no implantation occurs estrogen drops and period starts |
|
|
Whats the average length of the vagina |
3-3.5 inches |
|
|
Functions of vagina |
-passageway to eliminate menstrual fluids -place for penis during intercourse -forms lower portion of birth canal |
|
|
What lubricates the vagina |
-cervical secretions -water movement across vaginal epithelium |
|
|
The vulva consists of the |
Vestibule Labia minora and majora Urethral opening Clitoris Vestibular glands (maintains moisture) Mons |
|
|
Mammary glands |
Aprocrine Lobes Lobules Ducts |
|
|
Whats the lactiferous sinus |
Opening on nipple |
|
|
Whats the underlying of the boob |
Pectoral fat pad Pectoralis major |
|
|
Active breast development... |
-secretory apparatus develops during pregnancy -prolactin and human placental lactogen trigger development -fully developed at 6 months gestation |
|
|
What cells on the out side of the blastocyst in the first trimester come in contact with the uterine wall during implantation |
Trophoblast cells |
|
|
Describe a blastocyst |
-out cells are trophoblasts -inner cell mess made of stem cells -blastocyst cavity |
|
|
What happens when the trophoblast cells come in contact with the endometrial lining of the uterine wall |
They divide rapidly |
|
|
Where does the blastocyst implant in the uterus usually? |
The fundus or body usually |
|
|
What is formed when the trophocyst fuses with the endometrial lining |
A syncytiotrophoblast |
|
|
What is a syncytiotrophoblast? |
-layer of cytoplasm with multiple nuclei -releases hyaluronidase |
|
|
What is hyaluronidase |
Substance secreted by the syncytiotrophoblast to erode endometrial lining to zygote can implant |
|
|
What are the steps of implantation |
-trophoblasts come in contact with endometrial lining and divide rapidly -trophobast cells fuse with lining to make syncytiotrophoblast -extensions of trophoblast (villi) grow around endometrial capillaries and dissolve into capillary walls -when implanted the inner cell mass separates from trophoblast area -this forms 2 cavities: amnionic and blastocoele |
|
|
What facilitates the formation of lacunae in the first trimester |
-trophoblast villi extensions growing around endometrial capillaries and dissolving into them |
|
|
What 2 cavities are formed when the inner cell mass separates from the trophoblast? |
Amnionic cavity and blastocoele cavity |
|
|
What layers of cells form between the amnionic cavity and the blastocoele cavity in the first trimester? |
Epiblast layer and hypoblast layer |
|
|
What does the epiblast layet face? |
The amniotic cavity |
|
|
What does the hypoblast face |
The blastocoele cavity |
|
|
What produces the yolk sac? |
Migration and separation of hypoblast cells |
|
|
What provides the fetus with nutrients and eliminates waste? |
The umbilical cord |
|
|
Placental circulation |
-Blood flows from fetus to placenta in paired umbilical arteries -blood returns via a single umbilical vein |
|
|
Placental circulation |
-Blood flows from fetus to placenta in paired umbilical arteries -blood returns via a single umbilical vein |
|
|
What is labor |
A series of strong rhythmic uterine contractions |
|
|
What is the goal of labor? |
Parturition (get fetus out) |
|
|
What are the 3 stages of labor |
Dilation Expulsiob Placental |
|
|
What happens during the neonatal period |
-lungs fill with air -blood circulation changes (ductus arteriosus closes and so does foramen ovale) -heart rate drops from 120-140 to 70 bpm -breathing rate drops from 30 pm to normal rate -kidneys filter blood -digestive system becomes active -metabolic rate is increased to maintain warmth |
|

|
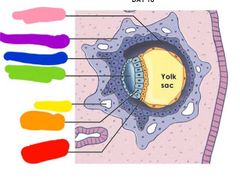
Red: blastocyst Orange: blastocyst cavity Yellow: trophoblast Green: inner cell mass |
|

|
Red: cytotrophoblast Yellow: epiblast Orange: hypoblast Green: syncytiotrophoblast Blue: endometrial capillary |
|
|
Red: hypoblast Orange: epiblast Yellow: lacuna Green: amniotic cavity Blue: cytotrophoblast Purple: syncytiotrophoblast Pink: blastocoele |
|
|
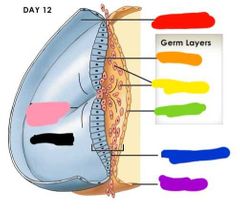
Red: amnion Orange: ectoderm Yellow: mesoderm Green: endoderm Blue: embryonic disc Purple: yolk sac Pink: primitive streak Black: blastodisc |
|

|
Red: chorion Orange: amnion Yellow: embryo Green: yolk sac Blue: fetal placenta Purple: maternal placenta Pink: umbilical cord Black: allantois |
|

|
Red: parietal decidua Orange: basal decidua Yellow: umbilical cord Green: placenta Blue: amniotic cavity Purple: amnion Pink: chorion Black: capsular decidua Brown: mucus plug |
|
|
Red: future head Orange: neural plate Yellow: neural folds Green: somites Blue: wall of amniotic cavity Purple: future tail |
|
|
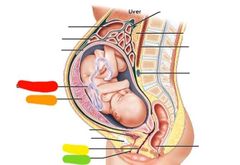
Red: placenta Orange: umbilical cord Yellow: uterus Green: amniotic fluid Blue: cervix Purple: vagina |
|
|
Red: umbilical cors Orange: placenta Yellow: vagina Green: urethra |
|
|
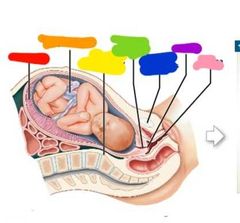
Red: placenta Orange: umbilical cord Yellow: not important Green: cervical canal Blue: pubic symphysis Purple: cervix Pink: vagina |
|
|
What creates the primitive streak? |
Gastrulation: Epiblast cells moving towards the center of the blastodisc |
|
|
What creates the 3 germ layers? |
-epiblast cells headed to the primitive streak migrating between epiblast layer and hypoblast layer |
|
|
What are the three germ cell layera |
Ectoderm Mesoderm Endoderm |
|
|
What do the 3 germ layers do? |
Each layer will form specific tissues and organs of the body |
|
|
What is the ectoderm |
-germ layer -derived from epiblast layer -is in contact with the amniotuc cavity |
|
|
What is the mesoderm |
-germ layer -new layer between the epiblast and hypoblast |
|
|
What is the endoderm |
-germ layer -derived from hypoblast layer |
|
|
What structure do the 3 germ layers make up |
Thr embryonic disc |
|
|
What extra embryonic membranes are formed by the germ layers |
Yolk sac Amnion Allantois Chorion |
|
|
What the yolk sac derived from |
Endoderm and mesoderm |
|
|
What is the yolk sac |
-A pouch that extends from hypoblast cells into the blastocoele -earliest site for blood cell formation |
|
|
What is amnion derived from |
Ectoderm and mesoderm |
|
|
What is amnion |
The amniotic fluid filled amniotic cavity...this provides cushion for embryo |
|
|
What is allantois derived from |
Endoderm and mesoderm |
|
|
What does allantois give rise to |
The urinary bladder |
|
|
What forms the chorion |
Mesoderm and trophoblast layers |
|
|
What is the chorion |
Blood vessels that link the embryo with the trophoblast |
|
|
When does the placenta form |
When chorion form villi that extend into the endometrial lining |
|
|
What is the placenta derived from |
Maternal and embryonic tissue |
|
|
Body stalk of the placenta does what |
Connects embryo to chorion |
|
|
Yolk stalk of the placenta does what |
Connects endoderm to yolk sac |
|
|
What regions develop as the placenta grows |
Capsular decidua Basal decidua Parietal decidua |
|
|
Placental circulation |
-Blood flows from fetus to placenta in paired umbilical arteries -blood returns via a single umbilical vein |
|
|
When does embryogenesis occur |
Shortly after gastrulation |
|
|
When do the head fold and tail fold develop for baby |
4 weeks |
|
|
What is organogenesis |
-Formation of organs -happens at 12 weeks |
|
|
What happens in the second trimester of pregnancy? |
-Fetus is covered by amnion -fetus grows faster then the placenta |
|
|
What happens in the third trimester of pregnancy |
Fetal organs become functional |
|
|
How much bigger does the uterus get during pregnancy? |
Goes from 7.5 cm to 30cm |
|
|
How much fluid does the uterus contain during pregnancy |
5 L |
|
|
How much does the uterus and its contents weigh during pregnancy? |
22 pounds on average |
|
|
What happens to a womens organs when pregnant |
They get pushed out of their normal position |
|
|
What happens in the dilation stage of labor |
-cervix dilates -fetus pushed by muscular contractions into cervical canal -amnion ruptures |
|
|
What happens in the expulsion stage of labor |
-fetus moves through cervical canal and vagina |
|
|
What happens in the placental stage of labor |
-placenta is ejected |
|
|
What is the neonatal period |
The period from birth to 1 month |

