![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
35 Cards in this Set
- Front
- Back
|
What are the layers (incldng spaces) from bone to brain?
|
Bone
Extra-dural space dura mater Sub-dural space Arachnoid mater sub-arachnoid space (CSF) Pia mater |
|
|
Which vessels cause an extra-dural hematoma? What usually causes this hemorrhage?
|
Middle meningeal artery and vein.
Usually trauma - hemorrhage compresses the brain that will regain it's shape/function once blood evacuated |
|
|
Describe a subdural hematoma (cause, course, effects)
|
Small vessels are broken so it's a slow bleed - the blood breaks down and becomes osmotically active drawing more fluid out --> more swelling --> more vessels get broken.
Usually d/t minimal trauma. Effects can be minor as the brain will accommodate the slow squishing |
|
|
Describe a subarachnoid hematoma (cause, symptom, tx)
|
Usually caused by a rupture of an aneurysm in the circle of willis at the base of the skull.
The blood leaks into the CSF or can spray agains the brain tissue itself, causing the worst headache of your life. Aneurysms can be repaired or clipped by accessing them through the carotid. |
|
|
A fracture of the ________ plate of the _____ bone, is particularly susceptible to infection. Why?
What is a sign that you have this #? |
# of the cribriform plate of the ethmoid bone is susceptible to infection because the # line will cross sinuses that are filled with bacteria which can then get into CSG --> meningitis.
Sign: CSF leaking from the nose! |
|
|
What 2 structures hold the brain in place?
|
Falx - separates the two hemispheres of the brain
Tentorium - separates posterior fossa contents from the rest of the skull cavity |
|
|
What happens to brain and falx/tent when there's a space occupying lesion?
|
The falx can shift a little to accommodate the lesion but eventually brain will herniate out the foramen magnum. (temporal lobe will herniate out of Tentorium beside the midbrain). ** Cerebellum can also herniate up
|
|
|
Why can the eye be thought of an an extension of the brain?
|
Because the cornea is continuous with the dura mater and has the same layers underneath it.
|
|
|
The 6 muscles of the eye sit in ____?
A tumor or enlargement of what 4 things can cause exophthalamus? |
Fat!!
CN III ocular muscles meninges lacrimal gland (thyroid diorders can also cause exopthalamus) |
|

Label adductors and abductors
|
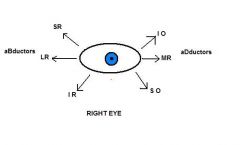
|
|
|
What is the effect of a CN VI palsy?
|
The lateral rectus will be affected = failure to abduct (down & in)
|
|
|
What happens when you get a CN IV palsy? (name of nerve?)
|
Trochlear palsy disables the superior oblique muscle resulting in difficulty in depressing the eye in adduction (will tend to have probs walking downstairs)
|
|
|
What happens when you get a CN III (name?) palsy?
|
Most of the muscles (MR, IR, SR, & IO) will get knocked out. Thus the eye will deviate laterally and downwards b/c SO and LR are the only ones left with tone.
|
|
|

|
|
|
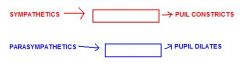
Horner's symptom can arise from a problem in sympathetic nerves anywhere along their pathway. List the pathway from T1 to the nerve's 4 possible destinations.
|
T1 - Sympathetic chain ---> climbe to superior cervical ganglia ---> carotid artery --> internal carotid --> cavernosus sinus --> opthalmic artery -->
1. dilator pupillae 2. Mullers muscles (levator pallpabrae superiorus = eyelid) 3. blood vessels 4. lacrimal gland |
|
|
From lateral to medial what is the order of the nerves that exit the superior orbital fissure?
|
Vein, Lacrimal (V1), Frontal (V1), Trochlear (IV), Superior division (III), Nasocilliary ( V1), Inferior division (III), and Abducens (VI)
|
|
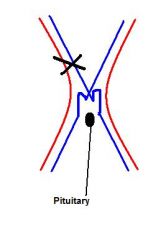
What would happen to the visual fields if there was a lesion like this? Why (ie. name the structure)?
|
The L field will be completely obliterated and the lateral side of R field will be lost. This is because at Von Willerbrand's knee there is cross-over between the fibers
|
|
|
What is a carotid-cavernous fistula?
|
When the epithelium of the carotid becomes continuous with the epithelium of the venous spaces w/in the sinus. (carotis passes through the sinus in middle of head, pituitary sits in the sinus)
|
|
|
Which sinuses are wholly within the fibrous layer of the dura? Where do extra-dural hematoma's happen?
|
The inferior saggital and the straight. E-D hematoma's happen between the endostial layer and the fibrous layers of the dura.
|
|
|
What are the 4 components of the facial nerve that all exit the __________ meatus?
|
Exiting the internal acoustic meatus:
Greater petrosal nerve Nerve to Stapedius Chorda tympani (contain parasymp for salivary glands and some sensory for taste) Facial Nerve* then leaves via the stylomastoid foramen |
|
|
Describe Herpes Zooster virus (where does it live in body - significance of this?)
|
Lives in nerves and the rash is produces will thus map the dermatome supplied by the infected nerve.
|
|
|
What is it called when an air sinus becomes infected? What is the effect of this?
|
Mucocele. Bones in the ethmoid sinus are mobile and thus an infection in the ethmoid air sinus can push the bones and cause V1 pain.
|
|
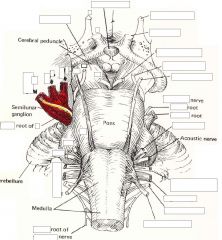
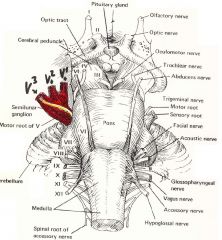
Identify the cranial nerves.
|
|
|
|
Where should you test for V function? Why?
|
On the front of the face b/c there are huge amounts of individual variation on the sides of the head.
|
|
|
Damage to the motor branch of CN V would produce what type of deficit?
|
The jaw would deviate to the paralyzed side when it is opened. Jaw deviates to side of injury.
|
|
|
What is TIC Douloureux?
1. Type of pain? onset, duration, location? 2. Affected age group? 3. Suspected cause? |
1.Stabbing very severe pains (can be immobilizing). Abrupt onset and termination, lasts mins/hours/days, restricted to trigeminal distributions (rarely also includes CN VII & IX)
2. 50-70yrs 3. Compression of trigeminal nerve by artery (most common), vein or tumor |
|
|
What is the medical tx for TIC douloureux? Surgical tx? (2 options)
|
Anticonvulsant therapy - effective for 75% of people
Surgery - (only after drugs have failed) 1. Gangliolysis: put a needle in the cheek and through the foramen ovale to create a lesion in V1, 2 or 3, by using heat, alcohol or pressure from a balloon. ** don't want anesthesia - just a loss of sensation. So, keep pt awake and do pinprick test - stop when no longer able to feel pinprick pain. 2. microvascular decompression - pull the vessels away from the nerve and use a small piece of felt to keep them apart. (much more invasive but very effective) |
|
|
Why are maxillar sinus tumors usually noticed by denturists?
|
Because these tumors will push teeth out and will change the shape of the mouth by changing the shape of the maxillary sinus.
|
|
|
What are the symptoms of a maxillary tumor?
T L N V# D L |
Toothache
Loosening of teeth Nasal discharge V2 pain - tumor will go through roof of maxilla and into infraorbital foramen Displacement of orbit as tumor moves superiorly Lacrimation - tumor will invade the lacrimal sac causing obstruction and tears will flow constantly down the face |
|
|
What is the parasympathetic never supply to the lacrimal gland?
|
The Rami Lacrimales that leave the pterygopalatine ganglia and go to the gland via the infraorbital fissure.
|
|
|
Describe the blood supply to the nose (ie. which part is supplied by which carotid). Where do most nosebleeds come from? Why?
|
All the vessels above the middle conchae are supplied by the internal carotid and all those below the conchae are supplied by the external carotid.
All 5 arteries supplying the nasal septum anastomose on the anterior portion of the nasal septum. As a result this ares is often where epistaxis occurs. |
|
|
How do parasympathetic fibers get to the submandibular and sublingual glands?
|
Presynaptic fibers are carried on VII, in chorda tympani. They synapse in the submandibular ganglia that hangs off the lingual nerve on top of the hyoglossus. The postsynaptic fibers reach the glands via arteries.
|
|
|
How do psym and symp fibers get to lacrimal gland?
(hint: start with CN VII) |
The greater petrosal nerve carries psymp fibers from CN VII, and branches at the geniculate ganglia. It then joins the deep petrosal nerve at the foramen lacerum (coming off the internal carotid). The newly formed nerve of the pterygoid canal goes to the pterygopalatine ganglia, synapse then go to lacrimal gland via the rami lacrimens.
|
|
|
How do psymp fibers get to the eye and what do they do there?
|
CN III carries the fibers to the cilliary ganglion that lies just inferior to the medial rectus. The fibers ynapse in the cilliary ganglion and then hitchhike out on the short ciliary nerves of V1 to constrictor pupillae and lens (cilliary) muscles.
|
|
|
How do psymp fibers get to the parotid gland?
|
Psymp fibers are carried on CN IX- glossopharyngeal. They leave on the tympanic branch, and go to the tympanic plexus on the promontory of the middle ear. They emerge as the lesser petrosal nerve, go through the temen tympani, into the middle cranial fossa, out foramen ovale and then synapse on the otic ganglion (between tensor velli palatini and madibular N). Psymp fibers leave otic ganglia by hitchiking on the auriculotemporal branches of V3.
|

