![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
262 Cards in this Set
- Front
- Back
|
Smooth muscle
|
found in walls of luminal organs, vessels;
under control of the autonomic nervous system (ANS) |
|
|
cardiac muscle
|
myocardium; under control of autonomic nervous system
|
|
|
skeletal muscle
|
voluntary
|
|
|
‘belly’
|
meaty part of muscle
|
|
|
tendons of origin
|
(connect ‘belly’ to bone) - closer to midline & less moveable
|
|
|
tendons of insertion
|
further from midline & more moveable
|
|
|
Collagen
|
primary protein in tendon
|
|
|
ligament
|
connect bone to bone
|
|
|
fulcrum
|
(F) The Joint functions as a FULCRUM (The fixed point around which the lever moves) and the Muscles provide the FORCE to move the Lever.
|
|
|
lever
|
(L) bar turning around a fixed point
Tendons are attached in such a way that they PULL on the Bones and make them work like LEVERS |
|
|
Pull
|
(P) Force or power
|
|
|
Weight
|
(W)weight or resistance
|
|
|
Type 1 lever system
|
Pull---Fulcrum---Weight
|
|
|
Type 2 lever system
|
Fulcrum---Weight---Pull
|
|
|
Type 3 lever system
|
Fulcrum---Pull---Weight
|
|
|
Circulation System
|
Cardiovasular system
Lymphatic System |
|
|
Lymphatic system
|
part of circulating system
|
|
|
return of interstitial fluid to cardiovascular system
|
interstitial fluid (lymph)
lymphatic capillary lymphatic vessel lymph node lymphatic vessel major lymphatic vessel |
|
|
right lymphatic duct
|
receives lymph f/ right half of head, neck & face; upper right extremity & right thorax region
|
|
|
thoracic duct
|
receives lymph f/ everything else and left brachiocephalic vein
|
|
|
Functions of Lymphatic system
|
tonsils, thymus gland,
can produce WBC & antibodies; all lymphatic tissue, spleen cancer can spread through lymphatic system lymph nodes found superficial or deep & follow major arteries |
|
|
Axial Skeleton
|
spine, skull, rib cage
|
|
|
Appendicular Skeleton
|
upper extremities
lower extremities |
|
|
Function of Spine
|
protect spinal cord and spinal nerves
provides a rigid and flexible axis for trunk provides a pivot for the head articulation posture and gate (walking) |
|
|
Movements of spine
|
flex (forward bending)
extend (backward bending) lateral bending circumduction-all of the above (circles) |
|
|
Curvatures of Spine
|
At birth, the thoracic and sacral curvatures are the only curvatures that exist- primary curvatures (posteriorly)
-As you develop, the cervical and lumbar curvatures form-secondary curvatures (anteriorly) |
|
|
Curvature Disorders of Spine
|
Kyphosis-extreme thoracic curvature posteriorly (hump back)
Scoliosis-abnormal later curvature Lordosis-exaggerated lumbar curvature |
|
|
Vertebrae
|
33 total
Body - round, anterior bodies articulate w/ intervertebral disc function-to support weight of body attached to anterior and posterior longitudinal ligaments |
|
|
Vertebrae
|
Cervical - 7
Thoracic - 12 Lumbar - 5 Sacrum - 5 (fused) Coccyx 3-5 (fused) |
|
|
Smooth muscle
|
found in walls of luminal organs, vessels;
under control of the autonomic nervous system (ANS) |
|
|
cardiac muscle
|
myocardium; under control of autonomic nervous system
|
|
|
skeletal muscle
|
voluntary
|
|
|
‘belly’
|
meaty part of muscle
|
|
|
tendons of origin
|
(connect ‘belly’ to bone) - closer to midline & less moveable
|
|
|
tendons of insertion
|
further from midline & more moveable
|
|
|
Collagen
|
primary protein in tendon
|
|
|
ligament
|
connect bone to bone
|
|
|
fulcrum
|
(F) The Joint functions as a FULCRUM (The fixed point around which the lever moves) and the Muscles provide the FORCE to move the Lever.
|
|
|
lever
|
(L) bar turning around a fixed point
Tendons are attached in such a way that they PULL on the Bones and make them work like LEVERS |
|
|
Pull
|
(P) Force or power
|
|
|
Weight
|
(W)weight or resistance
|
|
|
Type 1 lever system
|
Pull---Fulcrum---Weight
|
|
|
Type 2 lever system
|
Fulcrum---Weight---Pull
|
|
|
Type 3 lever system
|
Fulcrum---Pull---Weight
|
|
|
Cervical Vertebrae
|
found in neck C1-C7
|
|
|
C1-atlas
|
articulates w/ occipital condyles (occipital bone) this forms that atlanto-occipital articulation
this joint allows had to nod. has no spinous process, but does have a posterior arch |
|
|
C2-axis
|
articulates w/atlas. Atlanto-axial articulation-allows head to rotate from side to side
dens (odontoid process)-part of anterior arch of axis; fused with atlas |
|
|
C7-vertebral prominence
|
long, tapered spinous process
spinous process of cervical vertebrae is bifid; C7 is not bifid transverse foramen-located in transverse process; only found in cervical vertebrae (all 7) vertebral arteries-travel through transverse foramen of all transverse processes in cervical except C7. |
|
|
Thoracic
|
12; T1-T12
costal facets-facilitate articulation w/ heads of ribs -T1-T10-have facets on transverse processes; ‘transverse costal facet’-articulates w/ tubercle of rib |
|
|
Lumbar
|
5; L1-L5
very thick & short spinous processes bodies very large & thick |
|
|
Sacrum
|
5; S1-S5
5 fused vertebrae gives support to pelvis; forms part of posterior wall of pelvis-articulates w/ 2 parts of hip bone forms sacro-iliac joint 4 pair anterior and posterior sacral foramen allows for passage of dorsal and ventral rami of spinal nerves S1-sacral promontory (anterior side) sacral hiatus (posterior side) |
|
|
Coccyx
|
tail bone; 4 fused (3-5)
|
|
|
Intervertebral discs
|
located between pre-sacral vertebrae
-made f/ 2 types of tissue: fibrocartilaginous (1. fiber and 2. cartilage) -function-absorb energy of axial skeleton |
|
|
herniated disk
|
-when you have a herniated disk, the annulus fibrosis weakens. The nucleus pulposus intrudes outward. If you herniated posteriorly, you can get muscle weakness, abnormal sensations (b/c it is putting pressure on the spinal nerves) most of the time it is posterior herniation b/c the posterior ligament is weaker than the anterior ligaments.
disks dehydrate with time-so your spine shrinks. |
|
|
Zygapophyseal Joints
|
(facet joints)-formed between the flat surfaces of the superior articulation processes of an inferior vertebrae and the inferior articulating processes of the superior vertebrae.
|
|
|
SPINAL CORD
|
begins at magnum foramen and ends about L2
-42-45 cm in length -only occupies upper 2/3 of vertebral canal -superiorly it continues on as the medulla oblongata in the brain -located & protected by the vertebral canal -protection |
|
|
Spinal Cord
|
spinal cord is symmetrical except in two places
1)cervical enlargement-produces brachial plexus; brachial plexus produces nerves that supply the upper extremities 2)lumbar enlargement-produces lumbosacral plexus which form nerves that innervate lower extremities. |
|
|
Spinal cord
|
3 meninges
cerebrospinal fluid (CSF) ligament of vertebra |
|
|
conus medularis
|
around L2 the spinal cord tapers
|
|
|
filum terminal
|
condensation of pia mater; it terminates at the 1st level of the coccyx.
contains no neurons is associated with cauda equina |
|
|
cauda equina
|
aka-horse’s tail)-a collection of dorsal & ventral rootlets-(make up lumbar & sacral spinal nerves)
located in subarachnoid space surrounded by CSF |
|
|
Meninges
|
dura mater
arachnoid mater pia mater |
|
|
dura mater
|
continuous w/ dura of brain; tough, thick, vascular membrane
-terminates at coccyx level -superiorly it attaches to the magnum foramen; also attached (ventrally) to posterior longitudinal ligament (ventral surface of dura attached to posterior longitudinal ligament) -extends laterally into intervertebral foramen; it covers spinal nerves and dorsal root ganglion -spinal cord is suspended in dura mater by denticulate ligaments (about 21 pair-denticulate ligaments are not really ligaments, it is pia mater) |
|
|
arachnoid mater
|
-(middle layer)-avascular; continuous with arachnoid mater of brain. Separated by dura mater in a potential space called subdural space
-between arachnoid & pia mater is the subarachnoid space. This is filled with cerebral spinal fluid. -between L2 & L3-lumbar cistern |
|
|
pia mater
|
innermost of 3 layers. Surrounds spinal cord & each dorsal & ventral rootlets. Vascular. Also continuous w/ pia mater of brain
|
|
|
filum terminal
|
condensation of pia mater; it terminates at the 1st level of the coccyx.
contains no neurons is associated with cauda equina |
|
|
cauda equina
|
aka-horse’s tail)-a collection of dorsal & ventral rootlets-(make up lumbar & sacral spinal nerves)
located in subarachnoid space surrounded by CSF |
|
|
Meninges
|
dura mater
arachnoid mater pia mater |
|
|
dura mater
|
continuous w/ dura of brain; tough, thick, vascular membrane
-terminates at coccyx level -superiorly it attaches to the magnum foramen; also attached (ventrally) to posterior longitudinal ligament (ventral surface of dura attached to posterior longitudinal ligament) -extends laterally into intervertebral foramen; it covers spinal nerves and dorsal root ganglion -spinal cord is suspended in dura mater by denticulate ligaments (about 21 pair-denticulate ligaments are not really ligaments, it is pia mater) |
|
|
arachnoid mater
|
-(middle layer)-avascular; continuous with arachnoid mater of brain. Separated by dura mater in a potential space called subdural space
-between arachnoid & pia mater is the subarachnoid space. This is filled with cerebral spinal fluid. -between L2 & L3-lumbar cistern |
|
|
pia mater
|
innermost of 3 layers. Surrounds spinal cord & each dorsal & ventral rootlets. Vascular. Also continuous w/ pia mater of brain
|
|
|
cross section of spinal cord
|
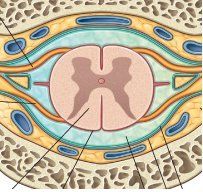
gray matter (H-shaped) it is gray b/c it contains cell bodies. Cell bodies are not myelinated. The cell axons of cellular processes of neurons are in the white area. They are myelinated and tend to be white
|
|
|
-CSF-cerebral spinal fluid
|
found in subarachnoid space around brain or spinal cord; also found in ventricular system of the brain.
|
|
|
-CSF-cerebral spinal fluid
functions |
1)acts as a cushion-a protective layer
2)physiological activities of neurons |
|
|
Cerebral Spinal Fluid
|
comes from choroid plexus of ventricular system
most is produced in lateral ventricles clear, contains electrolytes. No protein should be in CSF |
|
|
Blood Supply of Spinal Cord
|
3 sources
right & left posterior spinal arteries anterior spinal artery radicular arteries |
|
|
Blood Supply to Spinal Cord
right & left posterior spinal arteries |
both are branches of vertebral arteries, descend through magnum foramen. Serve upper 1/3 of the posterior side of spinal cord
|
|
|
Blood Supply to Spinal Cord
anterior spinal artery |
comes off vertebral arteries
descends & serves upper 1/3 of anterior side right and left posterior and anterior spinal arteries have an anastomal relationship- branches overlap |
|
|
Blood Supply to spinal cord
radicular arteries |
take care of distal 2/3 of spinal cord
branches off lumbar arteries |
|
|
spinal nerves
|
31 spinal nerves
8 cervical 12 thoracic 5 lumbar 5 sacral 1 coccygeal product of a fusing of a dorsal and ventral root (5-7 rootlets made a root) ventral roots contain motor neurons dorsal roots contain sensory neurons dorsal & ventral rami-become named nerve of peripheral nervous system most are products of ventral rami |
|
|
Superficial Muscles of spine
|
muscles that are attached to upper extremity and is involved in moving it (aka extrinsic back muscles)
innervated by ventral rami |
|
|
Intermediate Muscles of spine
|
muscles that are attached to the ribs and involved in respiration (aka extrinsic back muscles)
innervated by ventral rami |
|
|
Deep Muscles of spine
|
attached to spine (aka intrinsic-move the spine)
innervated by dorsal rami |
|
|
Thoracolumbar fascia
|
located in lumbar region
-very dense -connective tissue that ‘sandwiches’ the erector spinae muscles superficial fascia layer is thickest function-add strength; serve as an origin or insertion for a tendon |
|
|
trapezius Muscle
|
extrinsic, superficial, triangle shaped
O: superior nuchal line (skull)external occipital protuberance (skull) ligamentum nuchal (cervical vertebrae) spinous processes of C7-T12 I: spine of scapula acromion process of scapula F: extends & draws head side to side (lateral bending) adducts scapula IN: accessory nerve (cranial nerve 11) |
|
|
latisimus dorsi muscle
|
O: iliac crest, thoracolumbar fascia
lower 4 ribs spinous processes T7-T12 I: intertubercle groove of humerus F: extends, rotates and adduct upper extremities IN: thoracodorsal nerve |
|
|
levator scapula
|
extrinsic & superficial
O: C1-C4 I: medial border of scapula F: elevates scapula IN: dorsal scapular nerve |
|
|
rhomboid major & minor muscles
|
extrinsic & superficial
F: rotate & adduct scapula IN: dorsal scapular nerve |
|
|
serratus posterior superior muscle
|
F: pulls/elevates ribs respiratory muscle
IN: intercostal nerves (1-4) |
|
|
serratus posterior inferior muscle
|
extrinsic & intermediate
F: pulls down on ribs, respiratory muscle IN: intercostal nerves (10, 11 & 12) |
|
|
splenius capitus & splenius cervicis muscles
|
intrinsic & deep
O: base of skull F: extend head or neck, laterally bending head or neck IN: dorsal rami of cervical spinal nerves |
|
|
erector spinae muscle
|
aka sacrospinalis muscles)-intrinsic & deep
massive bilateral group of muscles that extend the full length of the back spinalis-most medial longissimus-intermediate iliocostalis-lateral F: extend spine; if only one side is working lateral bending IN: dorsal rami of intercostal nerves |
|
|
Thoracic cavity
|
cavity bound by thoracic wall & diaphragm
right and left pleura cavities |
|
|
mediastinal pleura
|
divides cavities so one side can handle trauma
|
|
|
LUNGS
|
located in thoracic cavity-not pleura cavity
F: exchange carbon dioxide with oxygen normal healthy lungs should be a pink color, but do get dark w/ time (particulate matter) both lungs attached to trachea via right and left bronchi |
|
|
pulmonary ligament
|
double fold of visceral pleura; inferior to root of lung-attaches lung to lateral side of pericardium
|
|
|
root of lung
|
where things go in and out
1 bronchus (right and left) 2 pulmonary veins lymphatic vessels & lymph nodes 2 pulmonary arteries (RIGHT lung only) 1 pulmonary artery (LEFT lung only) 1 bronchial artery (RIGHT lung only) 2 bronchial arteries (LEFT lung only) plexus of bronchial veins in general, right lung is larger than left |
|
|
LOBES
|
Right lung 3 lobes
Left lung 2 lobes |
|
|
Right lung
|
3 lobes
1)upper / horizontal fissure / (2)middle / oblique fissure / (3)lower apex is most superior portion (actually resides in neck) within lobes are broncho-pulmonary segments upper right-3 middle right-2 lower right-5 total in right lung: 10 |
|
|
Left lung
|
2 lobes
(1)upper / oblique fissure / (2)lower -broncho-pulmonary segments upper left-4 lower left-5 total in left lung: 9 |
|
|
alveolar sacs
|
within broncho-pulmonary segments
|
|
|
venous drainage of lungs
|
bronchial plexus
|
|
|
right bronchial plexus
|
drains into azygous vein
|
|
|
left bronchial plexus of veins
|
drains into hemiazygous & accessory hemiazygous veins
|
|
|
bronchi Lengths
|
right bronchus is larger & shorter than left bronchus
|
|
|
Pleural cavities
|
space between visceral pleura & parietal pleura
parietal pleura-serous epithelial membrane that line the internal aspect of thoracic wall and superior surface of diaphragm types of parietal: diaphragmatic pleura (next to diaphragm) cupola pleura (up top) costal pleura (next to ribs) |
|
|
visceral pleura
|
serous epithelial membrane that covers lungs
in pleura cavity you will find: serous fluid--acting as a lubricant |
|
|
pleuritis
|
-inflammation of pleura; excess fluid
|
|
|
dry pleurisy
|
membrane is diseased so fluid is not produced. Membranes rub-very painful.
|
|
|
Mediastinum Boundries
|
space
Boundaries anterior-sternum posterior-vertebral column inferior-diaphragm lateral-medial borders of the lungs |
|
|
Mediastinum Categories
|
anterior mediastinum
superior mediastinum middle mediastinum posterior mediastinum |
|
|
HEART
|
located in mediastinum
-a little left of center (mid-line) -apex-tip-located in 5th intercostal space -involuntary organ-controlled by intrinsic pacing system -can be influenced by autonomic nervous system |
|
|
Functions of heart
|
receive un-oxygenated blood
pump un-oxygenated blood to lung intakes oxygenated blood f/ lungs pumps oxygenated blood to systemic system (all tissue in body) |
|
|
Layer of hearts
|
Pericardium
Myocardium Endocardium |
|
|
Pericardium
|
outermost layer, superficial to myocardium
fibroserous sac (3 layers) 1. fibrous layer--(thickest, outermost, densest) allows pericardium to attach to vessels that enter or leave the heart 2. parietal serous layer-(adjacent to fibrous layer) 3. visceral serous layer-(in contact with myocardium) space between 2 & 3 is called pericardial cavity. Serous fluid is in cavity. Allows serous membrane to slide with no friction |
|
|
Myocardium
|
middle & thickest layer
cardiac muscle intrinsic pacing system of heart is located here thickness varies chamber to chamber can produce specialized structures 1. papillary muscles-only found in ventricles. Attached to cusps of bicuspid and tricuspid valves via chordae tendonae. -function of chordae tendonae is to prevent inversion of the valves 2. trabeculae-folds & bridges of myocardium |
|
|
Endocardium
|
innermost, thinnest, comes in contact with blood.
lines chambers of heart & also vessels that enter & exit the heart. |
|
|
Chambers of the Heart
|
Right atrium
Right ventricle Right ventricle Left Ventricle |
|
|
Right ventricle
|
pumping chamber
Function: pumps unoxygenated blood to lungs pulmonary artery takes oxygenated blood to lungs receives venous blood from right atrium shares septum w/ right atrium (right atrioventricular septum) shares septum w/ left ventricle (left interventricular septum) 3 papillary muscles-attached to cusps via chordae tendonae 1)anterior papillary 2)posterior papillary 3)septal papillary |
|
|
Right atrium
|
larger than left
walls are thinner than left atrium receiving chamber-receives venous blood superior & inferior vena cava & coronary sinus drain into right atrium shares interatrial septum w/ left atrium specialized structures -fossa ovalis-flat depressed area on right side of interatrial septum. Represents foramen ovale (open during fetal circulation) shares right atrioventricular septum w/ right ventricle right auricle adds volume to heart |
|
|
Left Atrium
|
receiving chamber
receives oxygenated blood f/ lungs enters through 4 pulmonary veins shares interatrial septum and left atrioventricular septum has left auricle |
|
|
Left Ventricle
|
largest chamber of the heart
receives oxygen blood f/ left atrium primary function to pump (profuse) oxygenated blood to systemic system 2 papillary muscles attached to cusps via chordae tendonae 1)anterior papillary 2)posterior papillary |
|
|
Valves of Heart
|
Right atrioventricular valve
Pulmonary valve Left atrioventricular valve Aortic valve |
|
|
Right Atrioventricular valve
|
(aka tricuspid valve)
made of 3 triangular shaped cusps attached to respective papillary muscles names of cusps 1)anterior cusp 2)posterior cusp 3)septal cusp Function: controls flow of blood f/ right atrium to right ventricle located in right atrioventricular septum open during diastole closed during systole |
|
|
Pulmonary valve (semilunar valve)
|
made of 3 semilunar cusps
1)anterior cusps 2)left cusps 3)right cusps open during systole closed during diastole controls flow of blood f/ right ventricle to lungs |
|
|
Left atrioventricular valve
|
(aka bicuspid or mitral valve)
located in left atrioventricular septum made of 2 cusps Function: controls flow of oxygenated blood between left atrium and left ventricle open during diastole closed during systole |
|
|
Aortic valve (semilunar valve)
|
Made of 3 semilunar valve
1)right cusp 2)left cusp 3)non-coronary cusp open during systole closed during diastole thicker, larger, & stronger than pulmonary valve |
|
|
Superior vena cava
|
located in superior mediastinum
tributary of right atrium 1 major tributary-arch of azygous vein formed by junction of 2 brachiocephalic veins |
|
|
brachiocephalic veins
|
2 brachiocephalic veins (right and left) are a product of the fusion of subclavian vein & internal jugular vein
left brachiocephalic vein is longer than right tributaries of brachiocephalic veins internal thoracic veins vertebral veins inferior thyroid veins |
|
|
Right Coronary Artery
|
Begins at right coronary cusp (at aortic valve)
Follows coronary sulcus (groove that correlates with atrioventricular septum) |
|
|
Right Coronary Artery Branches
|
SA (sinoatrial) nodal branch
Marginal branch Posterior interventricular branch |
|
|
SA (sinoatrial) nodal branch
|
This artery goes to the SA node (SA node is part of the intrinsic pacing system)
|
|
|
Marginal branch
|
comes off inferior aspect of the heart; travels or course towards the apex
|
|
|
Posterior interventricular branch
|
continuation of right coronary artery
Largest branch Found in posterior interventricular sulcus Function: serves the right ventricle (sulcus correlates with interventricular septum) |
|
|
Left Coronary Artery
|
Begins at left coronary cusps of aortic valve
Short- 1.5 inches in length Bifurcates in 2 major branches |
|
|
biforcation of Left Coronary Artery
|
anterior interventricular branch
circumflex |
|
|
anterior interventricular branch of left coronary artery
|
descends into anterior interventricular sulcus (correlates with anterior interventricular septum)
terminates with apex function: primarily serves left ventricle but does send branches to right ventricle. Serves interventricular septum. It forms an anastomosis relationship with the posterior interventricular artery Most heart attacks occur in anterior interventricular branch, this serves left ventricle which is vital |
|
|
circumflex branch of Left Coronary Artery
|
courses posteriorly to left
ends up in posterior coronary sulcus function: primarily serves left ventricle and two atrium |
|
|
Venous Drainage of Heart
Coronary Sinus |
main vein (receives directly or indirectly blood from all heart veins)
Tributary to right atrium Located in posterior coronary sulcus 2 major tributaries of coronary sinus |
|
|
major tributaries of coronary sinus
|
great coronary vein
middle cardiac vein |
|
|
great coronary vein
|
located in anterior interventricular sulcus
coronary sinus is a continuation of great coronary sinus |
|
|
middle cardiac vein
|
located in posterior interventricular sulcus
begins in apex region |
|
|
Intrinsic Conduction System of the Heart
|
function: to initiate the normal rhythmic heartbeat and coordinate the contractions of the 4 chambers
may be overridden by the autonomic nervous system (ANS) ANS Sympathetic—speeds up heart rate Parasympathetic—slows down heart rate The heart has potential to beat on its own (without ANS). Cells in heart ‘want’ to contract |
|
|
Sinoatrial node (SA node)
|
specialized area of modifies myocardial cells capable of initiating impulses. (responsible for initiating intrinsic cardiac cycle) (1 systole; 1 diastole)
|
|
|
Abnormalities with SA node
|
arrhythmia
|
|
|
SA Node
|
Located anterior and laterally at junction of superior vena cava and right atrium
|
|
|
SA Node
|
Innervated by ANS; both sympathetically and parasympathetically
|
|
|
SA Node
|
When SA node is activated it causes all myocardial cells in both atria to contract (blood goes from right atria to right ventricle and left atria to left ventricle)
|
|
|
Atrioventricular node (AV node)
|
Smaller than SA node
Located in the posterior, inferior aspect of the interatrial septum Near orifice of coronary sinus Receives input of myocardial cells of atria Sends information into both ventricles via the atrioventricular bundle (AKA: bundle of HIS) |
|
|
Atrioventricular Bundle (Bundle of HIS)
|
Located in the membranous (superior portion) part of the interventricular septum
Bifurcates into right and left bundle branches Right bundle branch Innervate myocardium of right ventricle Left bundle branch Innervate myocardium of left ventricle |
|
|
Purkinje fibers
|
tell myocardium (ventricles) to contract
|
|
|
Phrenic Nerves
|
Bilateral
Originate from cervical spinal cord (ventral rami of C3, C4, C5) Terminate with diaphragm Innervates diaphragm Located in posterior and superior mediastinum As it passes by myocardial sac-attached to pericardial sac |
|
|
Thymus Gland
|
Located in superior mediastinum
Inferior and deep to manubrium Lobated and large In young people it is pink; after puberty, it turns into fat (non-functioning in adults) Function: part of lymphatic system—immunity system. Processes T-lymphocytes (makes lymphocytes) and B-lymphocytes (makes antibodies) |
|
|
Superior Vena Cava
|
Located in superior mediastinum
Formed by the right and left brachiocephalic veins and terminates at the right atrium of the heart. |
|
|
Aortic Arch
|
Located in superior mediastinum
Continuation of ascending aorta Becomes descending aorta at approximately T-4 3 major branches innominate artery (aka: brachiocephalic artery trunk) left common carotid left subclavian |
|
|
Brachiocephalic trunk
|
bifurcates and forms
right subclavian right common carotid |
|
|
Descending aorta
|
T-4 and diaphragm
pass through posterior mediastinum passes through aortic foramen and enters abdomen always to left of esophagus (and midline) covered by parietal pleura it descends posterior to root of left lung |
|
|
Ligamentum Arteriosum
|
connection between arch of aorta and root of left pulmonary artery
located in superior mediastinum in adult, it is ligamentous tissue structure of fetal circulation |
|
|
Vagus Nerves
|
bilateral structures
C-10 Enter thorax through superior thoracic aperture, then enters posterior mediastinum (after passing through superior mediastinum) 2 major branches Right and left recurrent laryngeal nerves |
|
|
Right and left recurrent laryngeal nerves
|
Recur or travel back in neck
Innervate larynx Left arches under arch of aorta Right goes back under right subclavian artery |
|
|
Vagal nerves
|
branch and form vagal plexi and descend to posterior mediastinum
Plexi innervates lungs, heart and esophagus (all parasympathetically) Plexi re-condense into anterior and posterior vagal trunks These pass through esophageal foramen and enter abdomen. They branch and innervate structures in abdomen |
|
|
Esophagus
|
Located in posterior mediastinum
Muscular tube that begins with oral pharynx Terminates with esophageal sphincter Function: tube to get food and fluid from mouth to stomach |
|
|
Esophagus
|
Food is moved by peristalsis (rhythmic contractions of esophagus)
Peristalsis is under control of ANS Divided into 1/3’s – upper, middle, and lower Upper 1/3 – skeletal, voluntary Middle 1/3 – transition, (mixture) Lower/distal – smooth, involuntary No digestion takes place in esophagus, because there are no digestive enzymes. There is mucus in the stomach for lubrication |
|
|
Esophagus Arterial blood
|
Several pair of esophageal arteries (from thoracic aorta)
Several pair of esophageal veins—these are tributaries of the azygous vein |
|
|
Esophagus
|
Always to the right of thoracic aorta
Posterior to trachea Exits thoracic cavity through esophageal foramen (approximately at T-10 level) Esophagus is anterior to vertebral column |
|
|
Thoracic Duct
|
Located in posterior mediastinum
Located between thoracic aorta and esophagus Largest lymphatic vessel in body Begins in abdomen (approx. T-12) Chyle Cisterna—where thoracic duct begins Dilated sac Enters thorax through aortic foramen Ascends and terminates at junction of left subclavian vein & internal jugular vein [left brachiocephalic vein] |
|
|
Abdomen
|
area between diaphragm and pelvis
|
|
|
Abdominal wall
|
Superior wall—diaphragm
Posterior wall Anterior wall Lateral wall (2) |
|
|
Lateral wall muscles (3)
|
External abdominus oblique
Internal abdominus oblique Transverses abdominus muscle |
|
|
External abdominus oblique Muscle
|
O: Ribs 5-12
I: linea alba, pubic tubercle, and iliac crest Medial limit—linea semilunaris Fiber direction is inferior and oblique Most superficial of 3 lateral wall muscles |
|
|
Internal abdominus oblique Muscle
|
O: iliac crest, inguinal ligament, and thoracolumbar fascia
I: linea alba, ribs 10-12 Part of lateral wall Medial limit—linea semilunaris Fibers run inferior and oblique |
|
|
Transverses abdominus muscle
|
deepest of 3 lateral muscles
inguinal ligament, iliac crest, thoracolumbar fascia, cartilage from ribs 5-10 I: linea alba, pubic crest, inguinal ligament, xyphoid process Medial boundary—linea semilunaris Fibers run perpendicular to rectus abdominus muscle |
|
|
Anterior wall muscles
|
Rectus abdominus muscle Muscle
|
|
|
Rectus abdominus muscle Muscle
|
O: pubic symphysis and pubic crest
I: xyphoid process and costal cartilage from ribs 5, 6, & 7 Only muscle in anterior wall Has 3 tendonous intersections |
|
|
Function of Oblique and Transverse Abdominus Muscles
|
anteriorly flexing trunk
laterally bending trunk rotation of trunk |
|
|
Functions of
External abdominus oblique Internal abdominus oblique Transverses abdominus muscle Rectus abdominus muscle |
rectus abdominus - flexing trunk
all 4 muscles assist in respiration during inspiration, (when the diaphragm goes down) the muscles have to relax also pull down on ribs during forced expiration all 4 muscles put pressure on visceral structures during visceral functions vomiting urination defecation birthing |
|
|
Innervation of abdominal Wall
|
Intercostal nerves 6-12 and L-1 (bifurcates—iliohypogastric and ilioinguinal)
Skin and subcutaneous tissue are also innervated by these nerves |
|
|
Arterial blood Supply to abdominal muscles
|
Superior epigastric artery
Inferior epigastric artery Deep circumflex artery Lower 2 posterior intercostals arteries 4 pair of lumbar arteries lower anterior intercostals arteries |
|
|
Superior epigastric artery
|
Terminal branch of internal thoracic artery
Enters the rectus abdominal muscle superiorly and descends to meet the inferior epigastric about 1/3 of the way. They form an anastomotic relationship |
|
|
Inferior epigastric artery
|
Branch of external iliac artery
Ascends to rectus abdominus muscle; goes 2/3 of the way where it meets superior epigastric artery |
|
|
Deep circumflex artery
|
Branch of external iliac artery
Serves inferior parts of anterior and lateral abdominal wall |
|
|
Lower 2 posterior intercostals arteries
|
Branches of abdominal aorta; serve posterior abdominal wall
|
|
|
4 pair of lumbar arteries
|
serve posterior wall of abdominal wall
|
|
|
lower anterior intercostals arteries
|
serve anterior and lateral abdominal walls
branches of musculophrenic arteries |
|
|
venous drainage of Abdominal wall
|
Superior epigastric vein
Inferior epigastric vein Lumbar veins |
|
|
Superior epigastric vein
|
Tributary to internal thoracic vein
|
|
|
Inferior epigastric vein
|
Tributary to external iliac vein, common iliac and inferior vena cava
|
|
|
Lumbar veins
|
Tributaries to inferior vena cava
|
|
|
Rectus Sheath
|
Long aponeurotic sheath which encloses the rectus abdominus muscle
Formed by aponeurosis of 3 lateral abdominal muscles There is an anterior and posterior rectus sheath External oblique goes over (becomes part of anterior rectus sheath) Product of aponeurosis of internal oblique and transverses abdominus Aponeurotic layers fuse at midline and form the linea alba |
|
|
Fascia Transversalis
|
Layer of transparent fascia that lines all the abdominal cavity
Between muscle and aponeurosis and parietal peritoneum (lines abdominal cavity) |
|
|
Incisions lateral to the linea semilunaris
|
Skin
Subcutaneous tissue External abdominus oblique muscle Internal abdominus oblique muscle Transverses abdominus oblique muscle Transverses fascia (extraperitoneal fat) Peritoneum (parietal) Peritoneal cavity Peritoneum (visceral) Organ of abdominal cavity |
|
|
Peritoneum
|
Lines inner aspects of walls of abdomen and pelvis
May surround a visceral structure Moist (b/c of serous fluid) Function: allows sliding—reduction of friction between organs Layers: Parietal Visceral |
|
|
Parietal Peritoneum
|
Lines inner aspects of abdominal and pelvic wall
|
|
|
Visceral Peritoneum
|
Surrounds or is touching visceral organs
|
|
|
Peritoneal cavity
|
Space between parietal and visceral peritoneum
Special Structures of Peritoneum |
|
|
Mesenteries
|
double sheet of peritoneum which attaches an organ to the abdominal wall
May contain a variable amount of fat |
|
|
Types of mesentery
|
Greater omentum
Lesser omentum The mesentery Mesocolon |
|
|
Greater omentum
|
attached to greater curvature of stomach and transverse colon; varies in size. AKA policeman of the stomach b/c it walls off infection
|
|
|
Lesser omentum
|
hangs off lesser curvature of stomach. Also attached to liver and proximal duodenum
|
|
|
The mesentery
|
attaches small intestine to posterior wall of abdomen. Important b/c it contains vessels involved in absorption of amino acids, simple sugars, and fatty acids into the blood stream.
|
|
|
Mesocolon
|
attaches colon (large intestine) to posterior abdominal wall
|
|
|
Digestion
|
Proteins>amino acids
Carbohydrates>simple sugars Fats>fatty acids |
|
|
Peritoneal ligaments
|
double folds of peritoneum without the fat; extensive vessels function to stabilize structures with each other
|
|
|
Falciform ligament
|
attached liver to inferior portion of diaphragm
|
|
|
Peritoneal recesses
|
where peritoneum forms ‘blind’ pouches; where it reflects on itself.
|
|
|
Peritoneal Recesses
|
Omental bursa (lesser curvature of the stomach)
Epipoloic foramen—entrance to Omental Bursa (lesser sac) Peritoneal cavity (greater sac) |
|
|
Retro-peritoneal Structures
|
anterior (or ventral) surfaces are covered by parietal peritoneum
Anything behind parietal peritoneum |
|
|
Inguinal ligament
|
Product of rolled under edge of the aponeurosis of the external oblique muscle. (it’s a tendon)
Extends between Anterior Superior Iliac Spine (ASIS) and pubic tubercle Separation plane of tissue between abdomen and thigh |
|
|
Inguinal canal
|
Passage for:
Male - spermatic cord Female - round ligament of uterus The canal is about 4.5 cm long Runs inferiorly and medially Begins with deep inguinal ring Inguinal canal terminates with the superficial inguinal ring The inguinal canal is less prominent in women It is a 360 degree structure During fetal development, the gonads of the male travel down the inguinal canal to the scrotum. Also, the male has a higher risk of a inguinal hernia than a woman. |
|
|
Deep inguinal ring
|
found in abdominal cavity
Superior to inguinal ligament Just lateral to the branching of inferior epigastric artery |
|
|
Spermatic Cord
|
Begins with vas deferens
Extends between testicle and urethra Carries sperm and seminal fluids Pampiniform plexus of veins Testicular arteries Cremaster muscle Genitalfemoral nerve Varying types of fascia Sympathetic and parasympathetic nerves Lymphatic vessels |
|
|
Pampiniform plexus of veins
|
condense to form the testicular veins
Right testicular vein is a tributary to the inferior vena cava Left testicular vein is a tributary to left renal vein |
|
|
Testicular arteries
|
Right and left testicular arteries
Both branch off abdominal aorta; both come off just inferior to the renal arteries |
|
|
Cremaster muscle
|
Fibers are parts of internal abdominus oblique muscles
Function: to force sperm from testicles to urethra Innervated by genitalfemoral nerve |
|
|
Testis
|
Surrounded by dense connective tissue
Referred to as tunica albuguinea (white tissue) Function: produces sperm and hormone (ex: testosterone) Sperm are produced in seminiferous tubules |
|
|
Route of average spermatozoa
|
Seminiferous tubules of testicle
Rete testis Efferent ductules Head of epididymis Vas deferens Urethra Outside world |
|
|
Seminiferous tubules
|
Seminiferous tubules are connected to rete testis, rete testis are connected to about 20 efferent ductules; efferent ductules are attached to head of epididymis (kind of a storage) epididymis changes name to vas deferens
|
|
|
Epididymis
|
3 parts of Epididymis
1. head 2. body 3. Tail |
|
|
Scrotum
|
single structure
Muscular sac made of smooth muscle Dartos muscle—when exposed to cold, dartos contracts to keep testis warm (it pulls them closer to abdomen) Function - Protect testicles Keep testicles warm (sperm has to be a certain temperature to be viable) |
|
|
Arteries in Abdominal Cavity
|
descending aorta(abdonminal aorta)
Inferior Phrenic Arteries Lumbar Arteries Testicular / Ovarian arteries Adrenal Arteries |
|
|
Inferior Phrenic Arteries
|
paired
Serve inferior surface of diaphragm 1st branches off the aorta |
|
|
Lumbar Arteries
|
4 pairs
o Come off in lumbar region o Serve primarily posterior abdominal wall, some extend and serve lateral wall |
|
|
Testicular / Ovarian Arteries
|
Come off just inferior to renal arteries
Go to respective gonads |
|
|
Adrenal Arteries
|
numerous, small, bilateral branches
Come off superior to renal arteries |
|
|
Celiac Artery (aka celiac trunk)
|
not bilateral
Comes off about T12 Short, about 1 inch long 3 major branches splenic artery left gastric artery common hepatic artery |
|
|
splenic artery
|
goes to spleen (left)
|
|
|
left gastric artery
|
goes to lesser curvature of the stomach (left)
|
|
|
common hepatic artery
|
goes to right
branches serve liver, pancreas, gall bladder, duodenum and stomach |
|
|
Superior Mesenteric Artery
|
not bilateral
Comes off about 1 inch below celiac artery Extensive distribution pattern Serves small intestine, cecum, appendix, ascending colon, part of transverse colon |
|
|
Renal Arteries
|
bilateral; paired
Comes off about where superior mesenteric artery Comes off about L1 or L2 Travel to kidneys Left is shorter than right renal artery |
|
|
Inferior Mesenteric Artery
|
not bilateral
Comes off inferior to renal arteries Smaller than superior mesenteric artery Serves transverse colon, descending colon, sigmoid colon & rectum |
|
|
Inferior Vena Cava
|
Major vein in abdomen
Tributary of right atrium Formed by fusion of 2 common iliac veins Right of vertebral column Retroperitoneal structure Largest vessel in body in terms of diameter |
|
|
Tributaries of IVC
|
Renal veins (from kidneys)
Hepatic veins (from liver) Gonadal veins (right gonadal vein only)—(left gonadal vein is tributary of left renal vein) Lumbar veins (from posterior abdominal wall) Right adrenal vein (from right adrenal gland)—(left adrenal vein is a tributary of left renal vein) All digestive organs do not drain directly into IVC. They drain into the portal system. The portal system runs through the liver |
|
|
Stomach
|
Large sac-like structure
Made primarily of smooth muscle Smooth muscle runs horizontal and longitudinal. This means it facilitates peristalsis. Digestive organ Wall of the stomach Chief cells Parietal cells Proteolytic enzymes peristalsis On average the stomach can hold 2-3 quarts of food. |
|
|
Chief cells
|
Synthesize and secrete proteolytic enzymes
Enzymes digest proteins |
|
|
Parietal cells
|
Produce and secrete hydrochloric acid
|
|
|
Proteolytic enzymes
|
activated by hydrochloric acid. They are activated by the low pH.
|
|
|
peristalsis
|
Stomach churns
|
|
|
chyme
|
Stomach contents
|
|
|
Greater curvature of the stomach
|
(always to left)
|
|
|
Lesser curvature of the stomach
|
(always to right)
|
|
|
Lower esophageal sphincter
|
where the esophagus meets the stomach (aka-cardiac valve
|
|
|
Anatomical sections of Stomach
|
Fundus
Cardiac notch Cardiac orifice Body Pyloric antrum Pyloric canal Pyloric valve/sphincter Duodenum |
|
|
Internal Anatomy of Stomach
|
Lined with mucosal tissue
Protects stomach; also contains chief and parietal cells Folds and ridges in lining called rugae |
|
|
Stomach Location
|
Stomach touches diaphragm superiorly
Touches left lobe of liver to the right Inferiorly the stomach lies on top of the pancreas Inferiorly touches transverse colon |
|
|
Arterial Blood Supply To Stomach
|
Celiac artery----left gastric artery
Celiac artery----splenic artery----left gastroepiploic artery Celiac artery----common hepatic artery----gastroduodenal artery----right gastroepiploic artery Celiac artery----common hepatic artery----right gastric artery OR celiac artery----common hepatic artery----gastroduodenal artery----right gastric artery Splenic artery----4 or 5 short gastric branches Celiac Artery—primary artery that takes blood to stomach Left Gastric Artery Branch of celiac artery Goes to superior half of lesser curvature of stomach Left Gastroepiploic Artery Serves left half of greater curvature of stomach Right Gastroepiploic Artery Serves right half of greater curvature of stomach Right and left gastroepiploic arteries form anastomosis relationship Right Gastric Artery Serves inferior half of lesser curvature of stomach 4 or 5 short gastric branches comes off splenic artery serves body of stomach |
|
|
Venous Drainage System of stomach
|
Either drain directly or indirectly into portal system
Right and left gastric veins are tributaries of portal veins Right gastroepiploic vein is a tributary to superior mesenteric vein Left gastroepiploic vein is a tributary of the splenic vein Short gastric veins are tributaries of splenic vein Veins 4 or 5 short gastric veins right gastric vein right gastroepiploic vein left gastroepiploic vein Left Gastroepiploic vein Left Gastric vein Celiac vein |
|
|
Innervation of stomach
|
Innervated by ANS, both sympathetically and parasympathetically
Sympathetically it is innervated by the splanchnic nerves Parasympathetically it is innervated by the vagus nerve [FYI: Normally, the sympathetic nervous system speeds up activity, and the parasympathetic nervous system slows down activity. In digestion, they do the opposite.] |
|
|
Pancreas
|
the pancreas is a retroperitoneal structure
|
|
|
Function of Pancreas
|
Endocrine function—gland that produces hormones, but doesn’t have any ducts. (ductless system) The hormones go in vessels.
Isles of Langerhan Produce insulin About 1% of tissue is endocrine Exocrine—glands that have ducts 99% of tissue main pancreatic duct ability to produce digestive enzymes that digest proteins, carbohydrates, and fats |
|
|
Anatomy of pancreas
|
Head
Located in curve of duodenum Deep (posterior) to stomach Termination of main pancreatic duct Neck Between head and body About 2 cm in length Superior mesenteric vein and splenic vein fuse to form portal vein—this occurs posterior to neck Body Between tail and neck Crosses abdominal aorta Inferior and posterior to stomach Tail Terminates at hilum of spleen Terminal part of pancreas |
|
|
Celiac artery-->splenic artery-->10 short pancreatic arteries
|
Splenic artery
10 pancreatic arteries primarily serve the tail and body |
|
|
Aorta-->celiac artery-->common hepatic artery-->gastroduodenal artery-->superior pancreaticoduodenal artery
|
Serves head of pancreas
|
|
|
Aorta-->superior mesenteric artery-->inferior pancreaticoduodenal artery
|
Serves part of head of pancreas
|
|
|
Venous Drainage of pancreas
|
Veins have same name as arteries, just go backwards
Main vein that drains pancreas is the splenic vein (which is a tributary of superior mesenteric vein) |
|
|
Innervation of pancreas
|
Sympathetically—splanchnic nerves
Parasympathetically—vagus nerves |
|
|
LIVER
|
Weighs about 1500 grams
Largest organ in the body Occupies upper right quadrant of abdominal cavity Part of left lobe occupies upper left quadrant 2 major surfaces diaphragmatic surface—in contact with inferior surface of diaphragm visceral surface—in contact with different organs of abdomen attached to inferior surface of diaphragm right and left triangular ligaments covered by visceral peritoneum liver goes around IVC lobes right lobe—larger than left (two lesser lobes) quadrate lobe—resides between gall bladder and falciform ligament caudate lobe—adjacent or inferior to IVC left lobe—has no subdivisions both lobes are separated by falciform ligament falciform ligament double fold of visceral peritoneum also attach liver to inferior surface of diaphragm |
|
|
major metabolic functions of liver
|
biodegradation/breakdown of hemoglobin into bilirubin and bile
major detoxifying organ in body stores glycogen (a polymer of glucose) fat, protein, carbohydrates metabolism major producer of lymphatic fluids ¼ - ½ of lymph received by thoracic duct comes from the liver; therefore, there are a lot of lymphatic vessels in the liver |
|
|
porta hepatis
|
port of liver (where things go in and out of liver)
portal vein receives all venous blood from digestive organs formed by fusion of splenic v. and superior mesenteric v. tributary of liver |
|
|
portal venous system
|
venous system which directs all venous blood from digestive organs to pass through liver prior to returning to heart
portal system->capillaries of digestive organs->major veins-> superior mesenteric vein and splenic vein-> portal vein->liver-> sinusoids of liver->hepatic veins->IVC->right atrium involves two capillary beds—atypical; most of the body only has one capillary bed capillaries of digestive organs capillaries of liver |
|
|
arterial blood supply to liver
|
aorta-> celiac a. -> common hepatic a. -> hepatic a. proper
|
|
|
biliary tree
|
a. system of ducts which collect bile
b. hepatocytes—break down hemoglobin into bile. c. Bile collected in canaliculi (which are tributaries of interlobular ducts) tributaries to right and left hepatic duct right and left hepatic ducts fuse to form common hepatic duct common hepatic duct fuses with cystic duct to form common bile duct common bile duct and main pancreatic duct form at hepatopancreatic ampulla d. Choledochal sphincter (made of smooth muscle cells) e. Sphincter of main pancreatic duct (made of smooth muscle cells) f. Sphincter of Oddi—controls flow of bile or pancreatic secretions into duodenum |

