![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
Anaesthetic monitoring goal |
- Provide appropriate depth for the procedure - Maintaining normal physiological function |
|
|
- Anaesthetic monitoring |
- Monitor contiguously - Record ever 5 mins - Allows for actions |
|
|
- Monitoring Charts |
- Must be completed - Legal document - Don't neglecte patients by becoming focused on the chart |
|
|
What should be monitored |
- Anaesthetic depth - Circulation - Respiratory System - Temperature |
|
|
Palpebral reflex |
- Brush/ lightly touch medial canthus of the eye or eyelashes - Blink or spontaneous movement if light - Becomes sluggish as deepens - Don't do too often as response can diminish |
|
|
Corneal Reflex |
- Damp cotton bud drawn across the eye - Blink response - Should NEVER be absent |
|
|
Pedal Reflex |
- Firm pinch between toes - Withdrawal reflex - Depth increases = response reduces |
|
|
Jaw tone |
- Becomes looser as depth increases |
|
|
Eye Position |
- Observe both eyes - Surgical plane = ventromedial with some sclera visible - Depth increases = eye becomes central again - Ketamine affects this |
|
|
Pupillary Diameter |
Depth increases = pupil more dilated |
|
|
Salivation |
- Excessive with inadequate anaesthetic depth/pain relief - Breed variation |
|
|
mm and CRT |
- mm = pink - CRT = ~ 2 secs |
|
|
Heart rate and pulse quality
|
- Check every 5 mins - Rapids = light - Slows in surgical planes - Slows further as depth increases |
|
|
Respiratory rate and pattern |
- Check every 5 mins - Rapid & irregular = light - Slower & regular in surgical planes - Shallower & slower = too deep |
|
|
Temperature |
- Hypothermia common - Monitor every 5-30 mins - Frequency depends on case |
|
|
Purpose of monitoring aids |
- Provide additional information about the physiological status of the patient - Never replace basic hands on monitoring |
|
|
Using mechanical aids |
- More precise picture of health status - May detect early changes -> early intervention - Closer control |
|
|
Oesophageal stethoscopr |
- Simple and effective - Hear heart beat reliably - Cold chemically sterilised and re-use - 3 different lengths and widths - Easy to place if ET tube in place aleady |
|
|
Pulse oximeter |
- Non-invasive
- Arterial oxygen saturation - Probe usually placed on the tongue - Can be used on any non-pigmented skin - Audible HR - Oxygen always above 95% |
|
|
How does a pulse oc work |
- Two sources of light at different wave lengths - Absorbed by RBS - Absorption depends on how saturated with oxygen the RBCs are - Device recognises the pulsatile flow of arteries - Displays both oxygen saturation and pulse rate |
|
|
Pulse ox will fail when
|
- Peripheral vasoconstriction
- Low BP - HR too high - Diathermy and operating lights can disrupt the signal - Misleading if patient is anaemic |
|
|
Systolic Blood Pressure |
This is the peak pressure within the arteries that occurstowards the end of the cardiac cycle, when the ventricles are contracting. Itis determined by a combination of peripheral vascular resistance, stoke volumeand intravascular volume.
- Cats, dogs & horses = 90 - 120 mmHg |
|
|
Diastolic Blood Pressure |
This is the minimum pressure within the arteries that occurstowards the beginning of the cardiac cycle. This is when the ventricles arefilled with blood and is predominately determined by the peripheral vascularresistance
- Cats, dogs & Horses = 55 - 90 mmHg |
|
|
Mean blood pressure
|
Thisis the average blood pressure during the cardiac cycle. It provides informationabout tissue perfusion -Cats, Dogs & horses = 60-080 mmHg - Never less than 60 mmHg |
|
|
Why use BP monitoring |
- Direct information about peripheral circulation - Measures cardiovascular function - Useful for patients with cardiovascular disease or under going major surgery - Information on how well the heart pumps - IVFTSupports BP |
|
|
Low blood pressure |
Indicated that vital organs are not being sufficiently perfused and/or the patient is too deep. |
|
|
High blood pressure
|
Indicate that an animal is only lightly anaesthetised or that there is sympathetic stimulation |
|
|
Doppler Ultrasonography |
- Intermittent readings of BP - Apply cuff - Apply doppler to where pulse can be heard - Inflate cuff until pulse cannot be heard - Slowly deflate until first sound of pulse - This is the systolic blood pressue |
|
|
Oscullometric blood pressure |
- Measures magnitude of the arterial pulsations produced within the air filled cuff - Detects movement of artery wall against the cuff - Inaccurate results when patient is moving, Dysrhthmia, hypotension and bradycardia - Can take repeated measurements - All types of pressure recorded |
|
|
Capnograph |
- Information on both repiratory and cardiovascular function - Measures adequay of ventilation - Measure Carbon dioxide in each breath - No way of doing this manally |
|
|
Rebreathing carbon dioxide trace |
|
|
Ifbreathing is too shallow or slow carbon dioxide will build up in the lungs andthe end tidal carbon dioxide will rise |
|
|
Hyperventilation will lead to a reduction in ET carbon dioxide |
|
|
ECG |
- Provide useful info on HR and rhythm - Not indicate mechanical output - Tracing can continue may mins after heart ceased to be an effective pump - Audible beep |
|
|
ECG allows us to determine |
- Bradycardia - Tachycardia - Presence of arrhythmias |
|
|
What can and abnormal ECG shape show |
Indicate impending problems before abnormal 'pumping' action occurs |
|
|
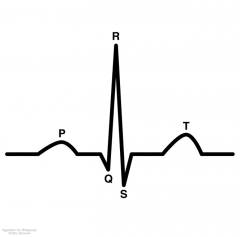
Normal Trace |
|
|
ECG trace does what |
Records the changes in direction of electrical current within the heartP |
|
|
P wave
|
- Electrical activity starts in the sino-atrial node and causes the atria to depolarise and contract
|
|
|
Q |
Passes theough the atrioventricular nose and into the ventricular septum |
|
|
R |
Cause the ventricles to contract |
|
|
S |
Produced as the top of the ventricles depolarise and complete the contraction |
|
|
T wave |
Occurs as the ventricles repolarise and the muscles relax |
|
|
How to take an ECG |
- Patient in right lateral recumbent on an insulated surface - Electrodes attach to lose clipped skin with plenty of contact gel - Red lead = RF - Yellow lead = LF - Green lead = LH - Black lea = RH |
|
|
What is displayed on a ECG screen |
- HR - ECG trace |
|
|
Arterial blood gas |
- Only way of truly knowing how much oxygen and carbon dioxide is in the blood - Gold standard - Blood sample taken form an artery and analysed - Not common in small animal general practice |

