![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
109 Cards in this Set
- Front
- Back
|
blood
|
* "the river of life"
* a fluid tissue three of the primary functions are: 1. Transportation 2. Regulation 3. Protection |
|
|
blood's Transportation:
|
Blood transports oxygen from the lungs and nutrients from the digestive system to the cells in the body. It then removes waste materials from the cells and delivers them to the organs that eliminate waste products
* transportation is used with cardiovascular or circulatory system and the lymphatic and immune systems |
|
|
blood's Regulation
|
The blood also regulates fluid and electrolyte balance, acid-base balance, and body temperature, making it a critical homeostatic mechanism.
|
|
|
blood's protection
|
Finally, the blood helps protect the body from infection by means of phagocytic white blood cells and antibodies. It prevents fluid loss through hemorrhage by implementing the clotting mechanism.
|
|
|
Blood Composition
|

* The average adult has approximately 4 to 6 liters of blood circulating throughout the body, or 7% - 9% of total body weight.
* It is slightly alkaline with a pH of 7.35 to 7.45, always staying just above neutral * almost never becomes the least bit acid, just less alkaline than normal * blood is connective tissue * men have more blood than women has two main components: 1. plasma - a liquid portion 2. formed elements - solid particles, or blood cells |
|
|
plasma
|
* the liquid portion of the blood component
* pale yellow fluid composed of water, proteins, ions, nutrients, waste products, food, hormones, oxygen, salts, gases and other solutes, and regulatory substances. * suspended in the plasma are many different types of cells and cell fragments that make up the formed elements * volume of the plasma part of blood is usually a little more than half the entire volume of whole blood (55%) plasma + formed elements = whole blood * plasma 100% = 7% proteins + 91% water + 2% other solutes * Proteins = albumins 57% + Globulins 38% + fibrinogens 4% + Prothrombin 1% * Other solutes = Ions, Nutrients, waste products, gases, and regulatory substances. * NEVER naturally contains anti-Rh antibodies * the blood minus the formed elements * It is composed primarily of water and is used to transport ions, nutrients, hormones, gases, and waste throughout the body. Plasma also contains proteins (solutes) such as (aka. Plasma proteins): * Albumin, which helps to draw fluid into the blood * fibrinogens - Clotting factors, which help to stop bleeding * Globulins, which include antibodies that protect us from infections * food and salts are dissolved in plasma and also about 3% of the total amount of oxygen (O2) transported in the blood * 5% of the total amount of the waste product carbon dioxide (CO2) that's carried in the blood is dissolved by plasma. |
|
|
Blood serum
|
* plasma without the clotting factors, such as fibrinogen and prothrombin.
* Serum contains antibodies so it can be used to treat patients who have a need for specific antibodies. * obtained from whole blood by allowing the blood to first clot in the bottom of a tube, then the liquid serum that remains at the top is poured off |
|
|
formed elements in blood
|
* the Solid particles in the blood component
* Makes up approx. 45% of whole blood * All of these elements have limited life spans but are replaced as needed by the bone marrow and lymphatic tissue of our body. three main types: 1. erythrocytes or red blood cells - 4.2 - 6.2 million per cubic mm. ( 5 million book) 2. leukocytes or white blood cells - 5K - 9K per cubic mm. ( 7500 book) a. Granular leukocytes 1. Neutrophils 2. Eosinophils 3. Basophils b. Nongranular leukocytes 1. Lymphocytes 2. Monocytes 3. platelets or thrombocytes -140K - 340K per cubic mm. (300K book) cubic millimeter = approximately 1 drop |
|
|
Red Blood Cells (RBC) or erythrocytes
|
* are biconcave disks, which mean that they are curved in on two sides
* They are the most numerous of the blood cells and have no nuclei or cytoplasmic organelles. normal range for men and women is 4.2 to 6.2 million cells per cubic millimeter. * RBC count varies with age, level of hydration, altitude of residence and other variables. * can't reproduce themselves or replace lost or damaged cellular components * most important functions are to deliver oxygen (transport oxygen) and nutrients to the body cells and remove carbon dioxide that has built up by transporting it to the organs of elimination. * red blood cells carry the protein molecule hemoglobin; which is primarily concerned with the transport of oxygen, but also transports a small portion of carbon dioxide. * circulate up to 4 months (80 to 120 days) before they break apart and their components are removed from the bloodstream by the spleen and liver. |
|
|
oxyhemoglobin
|
* oxygenated hemoglobin
* happens when red blood cells circulate through the lungs, oxygen attaches loosely to the iron in the hemoglobin. |
|
|
Red Blood Cell Disorders
|
* Most blood diseases are disorders of the formed elements
* often as a result of damage by toxic chemicals or radiation or if it is an inherited defect, viral infection or even cancer Red blood cell disorders are most commonly due to: * Increased production * Decreased production * Inadequate cellular function Treatments vary according to the disease but may include such measures as iron supplements, transfusions, bone marrow transplants, stem cell transplants, chelation, blood removal, irradiation of bone marrow, or chemotherapy. |
|
|
Polycythemia - Increased production of RBC
|
Polycythemia
* type of Red Blood Cell Disorders * a serious blood disorder characterized by dramatic increases in red blood cell numbers - increased RBC * can be due to an overproduction of red blood cells by the bone marrow or to an increase in blood cell production in response to a condition that interferes with oxygenation, such as lung disease. RBC count may reach or exceed 10 million * increases blood viscosity or thickness, which resists flow and can cause high blood pressure, coagulation problems excessive distention of blood vessels, and hemorrhaging. * RBC % (hematocrit) may reach 60% - norm is 45% * usually indicates a cancerous transformation of elements in the red bone marrow |
|
|
Anemia
|
Anemia
* type of Red Blood Cell Disorders * disorder that results in low oxygen carrying capacity of the blood and tissues * a condition in which the number of red blood cells or the amount of hemoglobin decreases or is ineffective. Overall inadequate numbers of RBCs. symptoms include: fatigued, weak, skin pallot, headache, and faintness. several types of anemia: * Aplastic anemia * Pernicious anemia * Hemorrhagic anemia a. acute blood-loss anemia b. chronic blood loss anemia * iron deficiency anemia * Hemolytic anemia (sickle cell and thalassemia) |
|
|
Inadequate cellular function of RBC
|
* type of Red Blood Cell Disorders
* These diseases are all associated with a decreased red cell life span due to a distortion or destruction Examples: * Sickle cell anemia * Thalassemia |
|
|
Hemorrhagic anemia
|
* caused by a decrease in the number of circulating RBCs which is due to a loss of blood from hemorrhage or bleeding
* RBCs produced during this time are both macrocytic and hyperchromic - an attempt to restore homeostasis by compensating for the low oxygen-carrying capacity caused by the hemorrhagic anemia. two types: 1. acute blood-loss anemia - resulting for example from extensive surgery or sudden trauma 2. chronic blood-loss anemia - caused by slow but continuous loss of blood over time from diseases such as cancer or ulcers. |
|
|
Pernicious anemia
|
* characterized by a dietary deficiency of vitamin B12 or from the failure of the stomach lining to produce "intrinsic factor"—the substance that allows vitamin B12 to be absorbed
* inability to absorb vitamin B12 * genetics plays a role in development of Pernicious anemia, might be an autoimmune disease * vitamin B12 deficiency impairs the bone marrow and results in decreased RBC production as well as a reduction in WBC and platelet numbers * treatment is vitamin B12 injections symptoms include: regular anemia plus nervous system problems such as numbness, tingling, and burning in the feet and hands, mental impairment, delusions, irritability and depression. |
|
|
Aplastic anemia
|
* characterized by destruction of bone marrow and low RBC count
* often related to high dose exposure to certain toxic chemicals such as benzene or mercury, irradiation, and in susceptible individuals, certain drugs including chloramphenicol * acute cases have death rates reaching 70% at 3 or 4 months after diagnosis * treatments include bone marrow or stem cell transplants |
|
|
Thalassemia
|
* an anemia that occurs more frequently among individuals of Mediterranean descent.
* a group of inherited hemolytic anemias * characterized by production of abnormal hemoglobin and inadequate numbers of small (microcytic) and often oddly shaped RBCs that are short lived. two forms: * thalassemia major - two defective genes inherited. severe and life threatening * thalassemia trait - mild, only one defective gene inherited |
|
|
Sickle cell anemia
|
* genetic disease characterized by the formation of abnormal hemoglobin.
* Formation of an abnormal type of hemoglobin called hemoglobin S (HbS) or sickle hemoglobin * This anemia is found almost exclusively within those of African descent. * a person who inherits only one defective gene develops only a small amount of HbS and has a form of the disease called sickle cell trait and often have no symptoms. could become ill under high stress or exertion situation. * if two defective genes are inherited it becomes sickle cell disease which can cause a reduction in blood flow, blood clotting and pooling of red blood cells in a crisis. |
|
|
Hemoglobin (Hb)
|
* red pigment in red blood cells
* oxygen-carrying component of the red blood cell * fills the space in the red blood cell since there is no nucleus and cytoplasmic organelles * Iron (Fe) is an essential nutrient needed to give hemoglobin its oxygen-carrying ability |
|
|
White Blood Cells (WBC) or leukocytes
|
* critical to survival, protect us from disease, and assist in preventing allergic reactions
* They are less numerous than red blood cells and have nuclei, and have a short life cycle (few days to weeks) * White blood cells are continually on the lookout for signs of disease * defend the body from microorganisms that invade the tissues or bloodstream. * When a germ invades the body, the white blood cells have a variety of ways by which they can attack. Some will produce protective antibodies that will overpower a germ, while others will surround and devour a pathogen using phagocytosis. * normal WBC ranges from 5,000 to 10,000 per cubic mm. of blood two classifications of White blood cells - WBC 1. agranulocytes a. Lymphocytes b. Monocytes 2. granulocytes three groups of white cells normally found in the blood: 1. Lymphocytes - with relatively clear cytoplasm 2. Monocytes - also with relatively clear cytoplasm 3. Granulocytes - with granular-filled cytoplasm |
|
|
Lymphocytes
|
* a type of White Blood Cell or leukocyte
* an agranulocytes * secreting antibodies * relatively clear cytoplasm * protect us against infections * B-lymphocytes produce antibodies to fight microbes * approximately 25% to 38% of all the WBC * function as immune mechanisms by secreting antibodies that destroy bacteria, viruses, and toxins. |
|
|
Monocytes
|
* a type of White Blood Cell or leukocyte
* an agranulocytes * relatively clear cytoplasm * largest of all the leukocytes or white blood cells * aggressive phagocytes capable of engulfing the larger bacterial organisms and cancerous cells * associated with "mono - the kissing disease" ie. macrophages is a specialized monocyte |
|
|
Granulocytes
|
* a type of White Blood Cell or leukocyte
* granular-filled cytoplasm or contain granules in their cytoplasm common granulocytes: 1. Neutrophils - the most abundant granulocyte 2. basophils 3. eosinophils |
|
|
agranulocytes
|
* a type of White Blood Cell or leukocyte
* include monocytes and lymphocytes * do not have granules in their cytoplasm |
|
|
Neutrophils
|
* are the most numerous or abundant granulocyte in the WBC
* most numerous white blood cells of the phagocytes * only live fro 10 to 12 hours * play an important role as a phagocytes |
|
|
basophils
|
* a type of Granulocytes in the WBC
* secretes histamine and heparin (anticoagulant) * present in small numbers * active during the inflammatory response through the release of the chemical histamine. * thought to play a role in the prevention of clotting. |
|
|
eosinophils
|
* a type of Granulocytes in the WBC
* limited in number, only 1% to 3% of the white blood cells * serve as weak phagocytes * most important in providing protection against infections caused by certain parasites and parasitic worms * also involved in allergic reactions |
|
|
heparin
|
* released from basophils in the WBC
* a substance that flows through the blood vessels of the body and inhibits the formation of blood clots * an anticoagulant |
|
|
macrophages
|
* specialized monocytes that grow to several times their original size after migrating out of the bloodstream.
* some wonder around the body searching for pathogens to destroy * some remain in particular organs such as the liver, spleen, lymph nodes, or bone marrow to help cleanse the blood of pathogens. * classification is an agranulocytes of WBC |
|
|
White Blood Cell Disorders
|
* are most commonly due to blood-related cancers or neoplasms
Two major groups of disease conditions constitute a majority of WBC and blood-related cancers or neoplasms: 1. Lymphoid neoplasms 2. Myeloid neoplasms common disorders: * Multiple myeloma * Leukemias * Infectious mononucleosis |
|
|
Myeloid neoplasms
|
* a White Blood Cell Disorders
* which arise from B and T lymphocyte precursor cells that are produced in lymphoid tissue |
|
|
Lymphoid neoplasms
|
* a White Blood Cell Disorders
* which are the result of inappropriate production of myeloid stem or precursor cells that normally produce granulocytic WBCs and monocytes |
|
|
Multiple myeloma
|
* cancer of the mature antibody-secreting cells derived from B cells, called plasma cells.
* the most common and one of the most deadly forms of blood-related cancers in people over 65 years of age. * Treatment may include chemotherapy, marrow and stem cell transplantation, and antibody treatment. |
|
|
Leukemias
|
* describes a number of blood cancers affecting the WBCs.
* In most cases, abnormal leukocytes invade the bone marrow and impair the normal blood cell production. * Malignant cells then metastasize throughout the body. * Treatment varies but may include chemotherapy and bone marrow or stem cell transplantation. * terms used to describe various "cancers" of the blood characterized by elevated and uncontrolled leukocyte production: ie. Chronic lymphocytic leukemia, acute lymphocytic leukemia, chronic myeloid leukemia, and acute myeloid leukemia |
|
|
Infectious mononucleosis
|
* the "kissing disease,"
* a noncancerous WBC disorder that appears commonly in adolescents and young adults. * Symptoms vary but may include sore throat, rash, severe fatigue, and enlargement of lymph nodes and spleen. |
|
|
acute myeloid leukemia
|
* accounts for 80% of all cases of acute leukemia in adults
* its sudden and progresses rapidly. |
|
|
Chronic lymphocytic leukemia
|
* most often affects older adults and is rare in individuals under 30 years of age.
|
|
|
acute lymphocytic leukemia
|
* aka. acute lymphoblastic leukemia.
* most common type of cancer in children * can also occur in adults, though the chance of a cure is greatly reduced. * type of cancer of the blood and bone marrow — the spongy tissue inside bones where blood cells are made * progresses rapidly and creates immature blood cells, rather than mature ones in white blood cells |
|
|
chronic myeloid leukemia
|
* accounts for approximately 20% of all cases of leukemia
* occurs most often in adults between 25 and 60 years of age. |
|
|
leukemia
|
* a general term used to describe a number of blood cancers that affect the white blood cells
|
|
|
Platelets or thrombocytes
|
* are irregular-shaped, colorless formed elements that play an essential role in blood clotting
* lifespan of a platelet is 7 to 10 days * Their sticky surfaces let them—along with other substances—form clots to stop bleeding. |
|
|
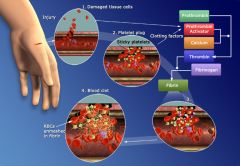
Blood Clotting
|
1. bleeding from a wound suddenly occurs. damaged tissue cells release clotting factors into the plasma which immediately react with other factors already in the plasma to form prothrombin activator.
2. platelets gather at the wound and attempt to block the blood flow by becoming sticky, and adhering to the damaged tissue cells. many platelets quickly accumulate near the opening in the broken blood vessel to form a temporary platelet plug releasing more prothrombin activator. 3. Calcium, vitamin K, and proteins such as fibrinogen help the platelets form a clot that will seal off the opening and stop the loss of blood, , (prothrombin activator triggers the conversion of prothrombin to thrombin. thrombin then reacts with fibrinogen to change the forming clot to a fibrous gel called fibrin. red blood cells accumulate in the fibrin, tissue damage is sealed by the clot, hemorrhage is stopped.) * the clot is formed during a series of chemical reactions that creates a net composed of protein fibers—much like cheesecloth * The net traps large particles such as red blood cells and platelets, which helps to stabilize the clot and stop the bleeding. * Vitamin K stimulates liver cells to increase the synthesis of prothrombin |
|
|
fibrin
|
* much like cheesecloth
* The net traps large particles such as red blood cells and platelets, which helps to stabilize the clot and stop the bleeding. * created when prothrombin activator triggers the conversion of prothrombin to thrombin. thrombin then reacts with fibrinogen to change the forming clot to a fibrous gel called fibrin |
|
|
Clotting Disorders
|
* clots are sometimes formed in unbroken blood vessels within our body.
* When this occurs, our body may shut off the blood supply to a vital organ such as the heart, brain, or lungs if that is where the clot has formed. common disorders: Hemophilia and Thrombocytopenia two types: 1. thrombus - clot remains in the place where it is formed; is pathological blood clot 2. embolus - clot or a part of the clot dislodges and begins to circulate in the bloodstream, curative blood clot |
|
|
thrombosis
|
* a Clotting Disorders
* caused by a thrombus - clot remains in the place where it is formed, |
|
|
embolism
|
* a Clotting Disorders
* caused by a embolus - the clot or a part of the clot dislodges and begins to circulate in the bloodstream |
|
|
Thrombocytopenia
|
* results from a decrease in the platelet count and is characterized by small purplish spots called petechiae.
* These spots are caused by bleeding from many tiny blood vessels throughout the body, most visibly in the skin and mucous membrane. * Treatment options include administration of corticosteroid-type drugs, transfusion of platelets, and in severe cases, surgical removal of the spleen. |
|
|
Hemophilia
|
* a hereditary deficiency of Factor VIII that is linked to the X chromosome.
* results in an impaired ability to clot blood and severe bleeding episodes. * bleeding episodes allow blood to leak into the joints—especially the elbows, knees, and ankles—and cause chronic pain and progressive joint deformity. * Treatment includes measures to prevent injury, rapid response to bleeding episodes, avoiding drugs that interfere with the clotting process, and the administration of Factor VIII. |
|
|
TPA
|
* used to dissolve blood clots
|
|
|
tissue plasminogen activator
|
* substances is given to patients to dissolve blood clots
|
|
|
hematocrit
|
* the volume percentage of red blood cells in a blood sample
|
|
|
acidosis
|
* the alkalinity of your blood decreases toward neutral
* become a very sick person |
|
|
whole blood
|
* precious commodity in regard to human life, especially in major injuries.
* used in blood donations * can only be stored for 6 weeks * must be cross matched and typed before being infused * "golden hour" the first hour after injury with severe blood loss * percentage by volume = 55% plasma + 45% formed elements |
|
|
plasma volume expanders
|
* helps maintain blood volume in the body for short periods after acute losses or in people with low blood volume, hemorrhage, severe burns, or kidney disease.
* will draw about three to four times its volume of fluid into the blood through the process of osmosis * unlike whole blood these solutions do not contain the needed components found in the formed elements and plasma that are required to maintain homeostasis over time. ie. albumin solutions |
|
|
artificial blood
|
* referred to as oxygen therapeutics
|
|
|
blood types
|
* identified as a specific type by using the ABO and Rh systems of classification
* types are identified by certain antigens in red blood cells |
|
|
antigen
|
* a substance that can stimulate the body to make or produce antibodies.
* found on the surface of the red blood cell * almost all substances that act as antigens are foreign proteins - they are not the body's own natural proteins but instead are proteins that have entered the body from the outside by means of infection, transfusion or some other method. |
|
|
antibody
|
* defined in terms of what causes its formation or in terms of how it functions
* by formation - a substance made by the body in response to stimulation by an antigen * by function - a substance that reacts with the antigen that stimulated its formation |
|
|
agglutinate
|
* clumping from antibodies reacting with their antigens ( type A antigen & type A antibodies)
* cause their target antigens to stick together in little clusters - process called agglutination * agglutination reactions cause the RBCs to burst or lyse; a process called hemolysis * harmful effects or even death can result from a blood transfusion if the donor's RBCs become agglutinated by antibodies in the recipient's plasma |
|
|
ABO system of typing
|
* every person is one of these types
1. Type A - 41% of americans have this type 2. Type B 3. Type AB 4. Type O |
|
|
Type A blood
|
* 41% of americans have this type
* A stands for a certain type of antigen (protein) in the plasma membrane of your RBCs that's been present since birth * because your born with Type A antigen, your body does not form antibodies to react with it * Type A blood plasma contains no anti-A antibodies * Type A blood plasma does contain anti-B antibodies |
|
|
Type B blood
|
* B stands for a certain type of antigen (protein) in the plasma membrane of your RBCs that's been present since birth
* because your born with Type B antigen, your body does not form antibodies to react with it * B blood plasma contains no anti-B antibodies * B blood plasma does contain anti-A antibodies |
|
|
Type AB blood
|
* universal recipient blood because it contains no anti-A or anti-B antibodies in its plasma and will not clot in any donor's RBCs containing A or B antigens. blood is compatible with A, B, and O blood types
* AB stands for a certain type of antigen (protein) in the plasma membrane of your RBCs that's been present since birth * because your born with Type A & B antigens, your body does not form antibodies to react with it * AB blood plasma contains no anti-A or anti-B antibodies |
|
|
Type O blood
|
* universal donor blood, always in short supply
* RBCs don't contain any anti-A or anti-B antigens * O blood plasma contains both anti-A or anti-B antibodies * because it contains no anti-A or anti-B antigens it will NOT clump by anti-A or anti-B antibodies it can be used in an emergency to any recipient with only minimal danger of anti-A or anti-B antibodies clumping its RBCs. * persons with any ABO blood group can receive type O blood in a transfusion. |
|
|
Rh-positive
|
* the RBCs of this blood type contain an antigen called the Rh factor
* More than 85 percent of people in the world are Rh-positive. |
|
|
RH System
|

* Rh is used because its blood cell antigen was first discovered in the blood of Rhesus monkeys.
* Rh factor - which is a different type of antigen located on the surface of the red blood cells * Rh factor is either present or absent from everyone's red blood cells. * More than 85 percent of people in the world are Rh-positive. |
|
|
Rh-negative
|
* RBCs do not have the Rh antigens or Rh factor on their surfaces
|
|
|
erythroblastosis fetalis
|
* type of hemolytic anemia
* caused by the mother's Rh antibodies reacting with the baby's Rh-positive cells * condition is also referred to as hemolytic disease of the newborn (HDN). * happens to a baby born with a Rh-negative mother and an Rh-positive father and the baby inherits the Rh-positive trait from his father, the Rh factor on the baby's RBCs may stimulate the mother's body to from anti-Rh antibodies. If she carries a second Rh-positive fetus the baby may develop this type of anemia * doesn't usually harm the first baby * mother becomes "sensitized" by the first baby * mothers should be treated with RhoGAM |
|
|
RhoGAM
|
* protein that stops the mother's body from forming anti-Rh antibodies preventing the possibility of harm to the next Rh-positive baby.
* given to Rh-negative mothers who carry an Rh-positive baby * attaches to any fetal red blood cells that may have crossed into the maternal circulation and causes them to be removed from the mother's system before she can become sensitized. |
|
|
connective tissue
|
two kinds that make blood cells for the body
1. myeloid tissue or red bone marrow 2. lymphatic tissue |
|
|
hematopoiesis
|
the formation of new blood cells
|
|
|
myeloid tissue or red bone marrow
|
* in adults, found mainly in the sternum, ribs, and hip bones
* small amounts found in the vertebrae, clavicles, and cranial bones * forms all types of red blood cells except some lymphocytes and monocytes |
|
|
lymphatic tissue
|
* forms the red blood cells lymphocytes and monocytes
* located mainly in the lymph nodes, thymus and spleen |
|
|
Granular leukocytes
|
* circulate only few days before they break apart and their components are removed from the bloodstream by the spleen and liver.
|
|
|
nongranular leukocytes
|
* can circulate more than 6 months before they break apart and their components are removed from the bloodstream by the spleen and liver.
|
|
|
aspiration biopsy cytology (ABC)
|
* test for bone marrow failure if it is the suspected cause of a blood disorder
* is a sample of myeloid tissue drawn into a syringe from inside the pelvic bone (iliac crest) or the sternum. * allows examination of the tissue that may help confirm or reject a tentative diagnosis |
|
|
bone marrow transplant
|
* needed when the bone marrow is severely damaged.
* myeloid tissue from a compatible donor is introduced into the recipient intravenously. * transplantation also may involve infusion of blood-forming, or hematopoietic, stem cells * if the immune system doesn't reject the transplant; a new colony of healthy tissue may become established in the bone marrow. * tissue destroyed by disease, high-dose irradiation, or chemotherapy is replaced and begin again to produce normal, functioning blood cells. |
|
|
hematopoietic or stem cells
|
* blood-forming
* can be harvested from the individual being treated, from a compatible donor, or from umbilical cord blood. |
|
|
normocytic
|
* in peripheral blood smears, an RBC of normal size is about 7 to 9um in diameter (approximately the same size as the nucleus of a small lymphocyte)
|
|
|
microcytes
|
abnormally small RBCs
|
|
|
macrocytes
|
larger RBCs
|
|
|
normochromic RBCs
|
normal color RBCs
|
|
|
hypochromic RBCs
|
RBCs that are deficient in hemoglobin
|
|
|
hyperchromic RBCs
|
RBCs that have an excess of hemoglobin
|
|
|
compensatory response
|
ie. production of macrocytic hyperchromic RBCs during periods of chronic blood loss intended to maintain homeostasis.
|
|
|
oxyhemoglobin
|
* forms when oxygen unites with hemoglobin to form an oxygen-hemoglobin complex
* makes possible the efficient transport of nearly 97% of all the oxygen required for the body cells (3% is dissolved in plasma) |
|
|
carbaminohemoglobin
|
* forms when hemoglobin combines with carbon dioxide
* it functions to transport about 20% of the carbon dioxide produced as a waste product of cellular metabolism to the lungs for disposal into the external environment. |
|
|
CBC or complete blood cell count
|
* a battery of tests used to measure the amounts or levels of many blood constituents
* often ordered as part of a physical exam * measures the actual numbers of circulating RBCs per unit of blood to provide a "normal" standard |
|
|
buffy coat
|
* layer of WBCs and platelets that settle after blood has been spun (spin) in the middle of the tube
* RBCs forms at the bottom of the tube * Plasma forms at the top of the tube |
|
|
hematocrit test
|
* packed-cell volume test (PCV)
* gives the proportion of RBC to plasma * WBCs and platelets that settle after blood has been spun (spin) in the middle of the tube * RBCs forms at the bottom of the tube * Plasma forms at the top of the tube * screens for dehydration, hemorrhaging, or their circumstances that affect the RBC ratio * normally 45% of blood volume consists of RBCs |
|
|
deficiency anemias
|
* caused by an inadequate supply of some substance such as vitamin B12 or iron required for red blood cell or hemoglobin production
* normal hemoglobin ranges from 12 to 14 grams per 100 milliliters of whole blood for adult females and from 14 to 17 for adult males. * hemoglobin of less that 9 grams per 100 milliliters of whole blood indicates anemia |
|
|
hemolysis
|
* destruction of red blood cells
|
|
|
blood doping
|
* practiced used by athletes to improve performance by injecting red blood cells (erythrocytes)
|
|
|
folate deficiency anemia
|
* similar to pernicious anemia because it also causes a decrease in the RBC count resulting from a vitamin deficiency of folic acid (vitamin B)
* common among individuals with alcoholism and other malnourished individuals * treatment involves taking vitamin supplements until balanced diet is restored. |
|
|
iron deficiency anemia
|
* caused by a deficiency of iron which is required for hemoglobin synthesis
* can be depleted through hemorrhage, increased requirements such as wound healing or pregnancy * most common nutritional deficiency in the world affecting 10% in developed countries, up to 50% in developing countries * indicated by a low hematocrit value * treatment is oral administration of iron-containing compounds, such as ferrous sulfate or ferrous gluconate |
|
|
hemolytic anemias
|
* as a group are all associated with a decreased RBC life span caused by an increased rate of destruction
* frequently an abnormal hemoglobin will cause red blood cells to become distorted and easily broken * might become jaundice caused by the conversion of the heme pigment of hemoglobin in the liver, have swelling of the spleen, problems with iron storage, and gallstone formation. |
|
|
hemolytic disease of the newborn
|
* begins during pregnancy if fetal RBCs of a different ABO type than the mothers cross the placenta and enter the mothers circulation.
|
|
|
leukopenia
|
* term used to describe an abnormally low WBC count < 5000 WBCs/mm3 of blood
* pretty rare |
|
|
leukocytosis
|
* term used to describe an abnormally high WBC count > 10,000 WBCs/mm3 of blood
* more common than leukopenia |
|
|
differential WBC count
|
* special type of white blood cell count
* reveals more information than counting * tests the proportions of each type of white blood cell and reported in percentages of the total WBC |
|
|
plasma cells
|
* are mature lymphocytes
* formed in large numbers in a type of bone marrow cancer called multiple myeloma |
|
|
T Lymphocytes
|
* do not secrete antibodies but instead protect us by directly attacking bacteria or cancerous cells
|
|
|
phagocytes
|
* protect our body from invading microorganisms by actually taking them into their own cell bodies and digesting them in the process of phagocytosis.
|
|
|
prothrombin activator
|
* Protein which activates prothrombin, the inactive precursor of thrombin.
* any one of the substances in the extrinsic or intrinsic pathways of coagulation. |
|
|
prothrombin
|
* A glycoprotein formed by and stored in the liver and present in the blood plasma that is converted to thrombin in the presence of thromboplastin and calcium ion during blood clotting. Also called factor II.
|
|
|
thrombin
|
* the activated form of coagulation factor II (prothrombin); it catalyzes the conversion of fibrinogen to fibrin.
|
|
|
fibrinogen
|
* A protein in the blood plasma that is essential for the coagulation of blood and is converted to fibrin by thrombin and ionized calcium
* Fibrinogen is synthesized in the liver by the hepatocytes * coagulation factor I |
|
|
International Normalized Ratio or INR
|
* a testing standard for the results of anticoagulation testing
* prothrombin time is reported in seconds - .8 - 1.2 is considered normal * keeping the INR between 2 and 3 will help ensure the prevention of unwanted blood coagulation conditions and will prevent further clotting in coronary blood vessels after a heart attack. |

