![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
123 Cards in this Set
- Front
- Back
|
Is the cardiovascular system a closed or open system?
|
Closed
|
|
|
What are the two types of capillaries in the body?
|
Systemic capillaries and Pulmonary capillaries
|
|
|
What type of blood do systemic veins bring back to the heart?
|
Deoxygenated
|
|
|
Oxygenated blood is carried by which types of vessels?
|
Systemic arteries and pulmonary veins
|
|
|
How many cardiac cycles does it take for the full path to be completed?
|
2
|
|
|
What does the circulatory system consist of?
|
-The heart
-Blood vessels -The blood |
|
|
What is the anatomy of the heart?
|
-4 chambers
-2 atria and 2 ventricles -intraventricular septum |
|
|
What is the name of the most inferior portion of the heart?
|
the APEX
|
|
|
The base of the heart lies where?
|
Superior, towards the clavicles
|
|
|
What valves separate the artia from the ventricles?
|
the atrioventricular valves
-Tricupsid is right -Bicuspid/Mitral is left |
|
|
What do the semi-lunar valves separate?
|
the ventricles from the aorta and/or pulmonary arteries
|
|
|
Do we have valves between the veins and the atria?
|
NO!
|
|
|
What is the purpose of valves?
|
to prevent backflow of blood
|
|
|
What structures help anchor the valves and prevent inverting of the valves?
|
Chordae tendineae and Papillary Muscles
|
|
|
What does the heart experience if a backflow of blood does occur due to a faulty valve?
|
the heart has to work that much harder to pump the same amount of blood per beat
|
|
|
Why are there no valves between the atria and the veins?
|
-Atrial pressure is low
-When atria contract, they squeeze the veins closed |
|
|
Where does the heart lie?
|
Within a pericardial sac
|
|
|
What are the two membranes surrounding the heart?
What is their function? |
Pericardial membrane
Epicardial membrane -produce fluid that surrounds them which helps reduce frictional forces against the heart with each beat |
|
|
What are the two main types of cells in the heart?
|
-Contractile muscle cells
-auto-rhythmic cells (ARCs) |
|
|
What percentage of auto-rhythmic cells are in the heart?
|
only 1%
|
|
|
In what ways is cardiac muscle a unique form of tissue?
what function does it have? |
1. connected through intercalated discs (not in any other form of tissue)
2. They have branched structure -these allow them to be physically anchored and electrically connected to each other |
|
|
What are the two types of membrane junctions involved in cardiac muscle?
|
1. Desmosomes
2. Gap Junctions |
|
|
What junctions are responsible for PHYSICALLY anchoring one plasma cell to another?>
|
Desmosomes
|
|
|
Describe Gap Junctions.
|
-Electrical synapses
-allows for a depolarization to move from one cell to the next without having to physically depolarize each cell -allow heart muscle to contract in unison |
|
|
Does the cardiac AP have a hyperpolarization stage?
|
Not a dramatic one
|
|
|
What is unique about the cardiac AP?
|
It has a plateau phase.
|
|
|
Describe the Cardiac AP
|
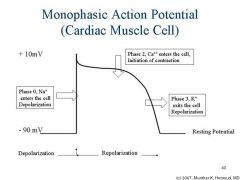
|
|
|
What is responsible for the plateau phase of the cardiac AP?
|
Sustained by the balance of Ca++ and K+ out.
|
|
|
What is the advantage of the plateau phase of the cardiac AP?
|
Allows for nearby cells to get on board and depolarize as a unit!
|
|
|
In pacemaker cells, what direction is the membrane potential constantly drifting towards?
|
Direction of depolarization
|
|
|
Why are pacemaker cells constantly close to depolarization/
|
Because Na+ is permeable and constantly slowing leaking INTO the cell!
|
|
|
Which ion's permeability will remain the same in pacemaker cells?
|
Sodium
|
|
|
Which channels are triggered at the pacemaker cell gets close to threshold?
|
Transient Calcium channels
|
|
|
What channels are triggered once threshold is reached in pacemaker cells?
|
L type Ca++ channels
L= long or latent because they stay open a little longer |
|
|
What is pacemaker potential?
|
Allow the cell to fire APs without any outside input in a spontaneous manner and with an intrinsically set pace.
|
|
|
What type of activity does the membrane potential of ARC's display?
|
pacemaker activity
|
|
|
Can cardiac contractile muscle cells contract without stimulation?
|
No, they must receive stimulation from pacemaker cells ARCs
|
|
|
What factor decides which node is the pacemaker of the heart?
|
the node that has the fastest natural firing frequency
|
|
|
Which node is the pacemaker of the heart?
What is its pace? |
The SA node
-70- 100 APs pm |
|
|
What is the pace of the AV node?
|
40-60 APs per minute
|
|
|
what is phase 4 of the cardiac cycle?
|
Resting cell (where we start)
|
|
|
What is the intrinsic pace of the Bundle of His and the Purkinje fibers?
|
20--40 APs
|
|
|
What do Purkinje fibers do?
|
Connect the Bundle of His and send the AP to the ventricles
|
|
|
Which node reaches threshold more quickly?
|
SA node
|
|
|
What are the 2 directions of AP sent from the SA node?
|
1. interatrial pathway: to the left atrium
2. internodal pathway: to the AV node |
|
|
What intrinsic property allows for the atria to contract before the ventricles, as well as encouraging maximal filing of the vents?
|
The AV nodal delay.
|
|
|
What is Systole?
|
Ventricular Contraction
|
|
|
Describe the Pacemaker AP
|
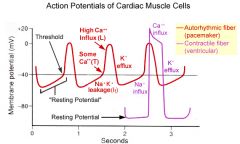
|
|
|
What is Diastole?
|
Ventricular Rest
|
|
|
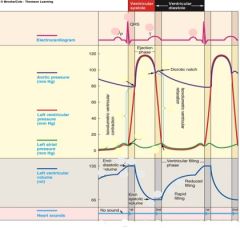
What are we recording in an EKG?
|
The sum of the electrical actvity as it reaches the skin
-as it is conducted to the surface of the skin |
|
|
What is the P wave?
|
Atrial depolarization
|
|
|
What is the PR segment?
|
AV nodal delay
-during this time atria are contacting |
|
|
What is happening during the QRS complex?
|
Ventricular depolarization
|
|
|
What does the ST segment signify?
|
Time during which the ventricles are contracting and emptying
-ejection of blood into the arteries |
|
|
What is the T wave?
|
Ventricular REpolarization
|
|
|
What is the TP interval?
|
Time during which ventricles are relaxing and filling
|
|
|
Why don't we see atrial repolarization in an EKG?
|
Because it is masked by the ventricular depolarization
|
|
|
Does the EKG give any mechanical information of the heart?
|
No only electrical!
-But mechanical things are happening at the same time |
|
|
What is considered an electrical event of the heart?
|
The spread of depolarization from the atria to the ventricles
|
|
|
What side of the heart are we considering during the cardiac cycle?
|
The left side
|
|
|
What happens before contraction?
|
depolarization of the muscle
|
|
|
What are the pressure ranges on the left side of the heart
|
0-120
|
|
|
What is the atrial kick?
|
A little kick of blood into the ventricles as a result of atrial contraction.
-Tops of ventricular filling |
|
|
When will the AV valve close?
At what point are we at in the EKG? |
When pressure in the vent is greater than pressure in the atria
-We are at he the QRS Complex |
|
|
What happens to ventricular volume when the QRS complex spikes?
|
It stays the same. Is in isovolumetric contraction.
|
|
|
What is isovolumetric contraction?
|
The time when no more blood in entering the vents, but they are contracting in order to generate pressure against the aorta.
|
|
|
When will the Aortic valve open?
|
When the pressure in the ventricle is greater than the pressure in the aorta
|
|
|
What is the status of all of the valves during isovolumetric contraction?
|
They are all closed
|
|
|
Why does the aortic pressure line increase during ejection phase?
|
Because the pressure in the aorta is also increasing
|
|
|
Does the ventricular pressure stay above aortic pressure during ejection phase?
|
Yes
|
|
|
What happens to vent volume when the aortic valve opens?
|
It drops rapidly
|
|
|
What is stroke volume?
|
the volume of blood ejected from each ventricle per systolic change
|
|
|
What is End-Diastolic Volume?
|
Volume of vents at the end of diastole (Larger number)
|
|
|
What is end-systolic volume?
|
volume of blood left over after ejection
|
|
|
What is ejection fraction?
|
The fraction of blood ejected from the heart per systole
-Healthy is 50-55% |
|
|
Right around the time of T wave, what is happening to the vents?
|
Parts of the vent are starting to relax
|
|
|
Does all of the vent repolarize and depolarize at the same time?
|
No, there can be both going on.
|
|
|
Where does the AP spread from in the vents?
|
From the apex, up the ventricles.
|
|
|
What type of movement does the vent undergo when it contracts?
|
It twists and rings itself out
|
|
|
When the pressure in the vents falls below aortic pressure what happens?
|
The aortic valve shuts (Dub)
|
|
|
What is the dicrotic notch?
|
Blip in aortic pressure. Reverberation of pressure against the aortic wall.
|
|
|
Could the dicrotic notch be felt throughout the arterial tree? theoretically?
|
Yes
|
|
|
When does isovolumetric relaxation occur?
|
when the pressure of vents is below aortic, but still above atrial.
-Continues until atrial pressure exceeds ventricular |
|
|
Why do you get a rush of blood into the vents as soon as the AV valve opens?
|
Because the atria were actually filling while the ventricles were contracting
|
|
|
Why can the atria fill while the ventricles contract?
|
Because of cardiac suction
|
|
|
What is cardiac suction?
|
When ventricles are twisting, the atria volume is being expanded and creating a negative pressure that sucks blood from the veins
|
|
|
What is passive filling?
|
It is the rush of blood into the ventricles without contraction of muscle
|
|
|
What percent of ventricular filling happens during the atrial kick?
|
ONLY 20%, So 80% of filling happens during diastole!!
|
|
|
What is the equation for Stroke Volume?
|
SV=EDV-ESV
|
|
|
What is afterload?
|
The resistance to ventricular ejection
-The workload that the heart has to meet and exceed to have ventricular contraction |
|
|
What does the diastolic pressure of the aorta say about the work of the heart?
|
It is based on the tone of the aorta (properties of the aorta and blood volume)
-The higher the pressure, the more work the heart has to do to imitate ventricular ejection |
|
|
What is cardiac output?
|
Volume of blood ejected from each ventricle per minute.
-Left should equal right |
|
|
If the R Cardiac Ouptput (CO) > L CO, what could be happening?
|
There may be some congestion in the pulmonary system
|
|
|
What is the equation of Cardiac Output?
|
Stroke Volume x Heart Rate
-~70 ml/beat = 5 liters/ min -At rest, our heart pumps out entire blood supply every minute |
|
|
What is maximal HR a function of?
|
Age
-Some individuals can reach a higher peak HR than what you would expect -Usually 220 - age |
|
|
What is Max stroke volume dependent on?
|
-Weight
-size -How in shape your heart is |
|
|
What is your cardiac reserve?
|
Max CO - resting CO
|
|
|
What is your cardiac reserve a prediction of?
|
Potential for physical performance
|
|
|
What type of control contributes to increasing HR and Stroke Volume
|
Autonomic Control
|
|
|
What effect does the parasympathetic Pathway have on the HR.
|
It will lower the firing frequency of the SA node thus slowing down HR
|
|
|
What does it mean to have parasympathetic tone to the heart?
|
You have low resting HR
-Your heart can put out the same CO with fewer beats -Thus you increase RESERVE!! |
|
|
Which vagus nerve has greater innervation on the SA node?
|
The R Vagus nerve
|
|
|
The AV node is innervated predominantly by which vagus nerve?
|
The Left
|
|
|
What effect do the R and L Vagus nerves have on the heart?
|
They decrease the firing frequency
-They also will increase AV nodal delay |
|
|
What effect does an increase in AV nodal delay have on heart workload?
|
This will bring about greater filling of the ventricles and thus your are pumping more volume per beat
-Thus allowing the heart to work less overall |
|
|
What effect does the Sympathetic Pathway have on the heart?
|
-Raise the firing frequency
-minor shortening of the AV nodal delay -Will bring cells closer to threshold |
|
|
Does the decrease in AV nodal delay during sympathetic pathway compromise the filing of the vents?
|
No it does not.
|
|
|
What are the 2 mechanisms involved in altering SV?
|
-Intrinsic control
-Extrinsic control |
|
|
What does intrinsic control of the heart require
|
Requires nothing but exploiting natural properties of the heart
|
|
|
When you increase the stretching of the cardiac muscles, does this reduce contraction strength?
|
No, it actually increases contractibility of the heart.
|
|
|
What is the optimal length for contraction for skeletal muscle?
|
The resting length of the muscle
|
|
|
How do you increase the strength of contraction in the heart?
|
You increase EDV by increaseing venous return (the amount of blod
|
|
|
What is an inotropic agent?
|
anything that effects contractility of the heart
-Positive: enhances contractility -Negative: decreases contractility |
|
|
Describe a chronotropic agent
|
Anything that changes HR
|
|
|
Why is lengthening the cardiac muscle cell generate more force?
|
Because the branches come in line with each other and thus can contract more!
|
|
|
What is Frank-Starling Law of the Heart?
|
It is the relationship between EDV, stroke volume and force
-Get more out than you've put in. -With Sympathetic added to it, you get more exaggerated Frank Starling relationship You have 2 mechanisms on top of each that stimulates stroke volume |
|
|
What is extrinsic control of the heart?
|
Sympathetic activity on the heart
|
|
|
Which ways does sympathetic activity effect cardiac output?
|
-Extrinsic control: + stroke volume= +CO
- +HR = + CO -+Venous return = increase EDV |
|
|
Why is lengthening the cardiac muscle cell generate more force?
|
Because the branches come in line with each other and thus can contract more!
|
|
|
What is Frank-Starling Law of the Heart?
|
It is the relationship between EDV, stroke volume and force
-Get more out than you've put in. -With Sympathetic added to it, you get more exaggerated Frank Starling relationship You have 2 mechanisms on top of each that stimulates stroke volume |
|
|
What is extrinsic control of the heart?
|
Sympathetic activity on the heart
|
|
|
Which ways does sympathetic activity effect cardiac output?
|
-Extrinsic control: + stroke volume= +CO
- +HR = + CO -+Venous return = increase EDV |
|
|
Describe the cardiac Table
|
|

