![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
With GU surgery what sensory level is preferred for regional anesthesia?
A. T4 B. T5 C.T6 D.T7 E. T10 |
T10= umbilicus
|
|
|
With GU procedures, regional anesthesia is preferred because mental status is easily evaluated, signs and symptoms of bladder perf are evident, and there is a reduced incidence of DVT.
|
Statement
|
|
|
True or False: Sedation for GU procedures may mask signs of water intoxication.
|
True
|
|
|
The following symptoms are common for what type of bladder perforation?
-periumbilical , inguinal, or suprapubic pain, lower abdominal distention, & pain. |
Extraperitoneal bladder perforation
|
|
|
The following symptoms are characterized by what type of bladder perforation?
- abdominal rigidity, distention, pain, referred shoulder pain, hiccup, shortness of breath, tachycardia, hypo or hypertenstion, diaphoresis, and vomiting. |
Intraperitoneal bladder perforation pg. 720 Nag.
|
|
|
Which of the following is not a complication associated with GU TURP surgery?
a.TURP syndrome b.hyperthermia c. hypothermia d. bladder perforation e. coagulopathy (rare) f. septicemia |
b. hyperthermia
They use cold rather than warm fluid to prevent vasodiation and further bleeding with the procedure |
|
|
Blood loss with a TURP procedure: choose all that apply
a. is difficult to assess b. depends on the size of the gland (>45 gm) c. depends on the resection time (>90 mins) d. depends on the surgeons skill e. averages 6-8 ml/min resection time = 400-600ml f. transfusion is indicated in 2.5% patients |
a, b, c, d, f are true
the average blood loss is 3-5ml/min of resection time totaling 200-500ml. |
|
|
- According to our lecture, the reccomended resection time for a TURP procedure should be less than 60 mins. Blood loss depends on a resection time > 90 mins based on the notes.
|
.
|
|
|
True or False: TURP syndrome doesnt occur after 24 hours post procedure and therefore is unimportant at that time.
|
False: TURP syndrome can occur up to 24 hours post procedure and occurs in 2-10 % of TURP patients.
|
|
|
Cardiovascular symptoms of TURP syndrome include: choose all that apply
a. CHF b. pulmonary edema c. hemolysis d. hypertension e. bradycardia f. hypotension g. fever |
Fever is not mentioned and is not a CVS symptom of TURP
|
|
|
Neurologic symptoms of TURP include all of the following except:
a. seizures b. coma c. death d. confusion e. restlessness/agitation f. somnolence |
f. patients are more likely to be restless and agitated than somnolent unless sodium levels fall to drastic levels.
|
|
|
Movement of intravascular water into cerebral cells causes......
|
cerebral edema
|
|
|
The leg height in the lithotomy position is an important anesthetic consideration because?
|
the higher the legs, the increase in risk for decreased perfusion d/t gradient from heart to legs
|
|
|
exaggerated lithotomy position is most commonly used for which kind of surgery?
A. TAH B. TURP C. radical prostatectomy D. hemorrhoidectomy |
C
|
|
|
Resp. considerations of lithotomy position include:
A. risk of tube migration down R mainstem when legs elevated B. diaphragm shifting cephalad C. increased abdominal pressure on diaphragm D. decreased FRC |
All are correct
|
|
|
Why are regional anesthetic techniques preferred for GU surgeries?
|
sedation can mask mental status changes associated with TURP syndrome
|
|
|
TURP syndrome is also known as
(2 things) |
water intoxication
dilutional hyponatremia |
|
|
Common peroneal nerve injuries can lead to what complication?
|
footdrop
|
|
|
Compartment syndrome is a complication of lithotomy position: T or F
|
T
|
|
|
What causes TURP syndrome?
|
Absorption of irrigating fluid through venous sinus near the prostate.
|
|
|
What causes the symptoms of TURP Syndrome?
a. dilutional hypernatremia b. dilutional hyponatremia c. hyperkalemia d. hyperosmolality |
B
|
|
|
Which is NOT a contributing factor to TURP syndrome?
a. irrigation fld pressure b. hypotonicity of irrig fluid c. solute toxicity d. prostate resection time of 45-60min e. >20ml of irrig fluid absorbed per min f. resection time of 15-18min |
All contribute except F. Shorter times are better.
|
|
|
The ideal irrigating fluid for TURP procedures will have all except:
a. isotonic b. contain K+ c. inexpensive d. non-hemolytic e. tranparent |
B is false. We want a non-electrolyte fluid to not interfere with the electrical current of the cautery.
|
|
|
T/F: Mannitol is the best irrig fluid to use for a CHF pt having a TURP b/c of it's diuretic effects.
|
FALSE: Before diuresis occurs, mannitol first increases circulating blood volume which can overload a CHF pt.
|
|
|
Which two types of patients should Glycine not be used as the irrigation fluid during a TURP?
a. severe hepatic dz b. L-arginine deficiency c. Diabetic d. CHF patient |
A b/c glycine is metabolized in the liver to ammonia.
B...not sure why. Not mentioned in textbook, but is on slide. I think it's related to metabolism of the glycine. |
|
|
T/F: Glycine toxicity may lead to tinitis.
|
False: Blindness that resolves with decreasing NH3 levels.
|
|
|
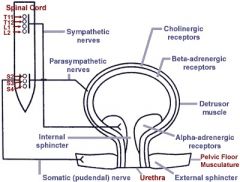
CNS innervation of the Bladder
|
|
|
What are two common methods of Regional Anesthesia used for Bladder procedures:
a. Spinal b. Brachial plexus block c. Epidural d. SAB (subaracnoid) |
c & d
|
|
|
What dermatone level needs to be blocked when using a Regional technique for bladder procedures?
|
T-10 level
|
|
|
When using regional anesthesia for bladder procedures, which method will have a "shorter onset":
a. SAB b. epidural |
SAB
|
|
|
Common dose for SAB when doing bladder procedures?
What is the duration of action? |
45 mg 1.5% lidocaine
45-60 minutes (can add epi 1:200K) |
|
|
The prostate gland increases in size after what age?
|
after age 40
|
|
|
What GU condition leads to bladder neck obstruction?
|
BPH
|
|
|
Benign prostatic hypertrophy frequently leads to....
choose 3 a. recurrent GU infections b. bladder stones c. erectile dysfunction d. renal insufficiency |
a, b, d
|
|
|
Indications of Transurethral surgery of the prostate (TURP) include:
(gland volumes) a. >50 ml b. 20-30 ml c. 40-50 ml d. <30 ml |
c
|
|
|
What are 3 resection methods used for the TURP procedure:
a. electrosurgical loop b. Laser c. fiberoptic d. microwave |
a,b,d
|
|
|
T or F
to avoid bleeding during the TURP procedure it is important to stay within the prostatic capsule. |
True
|
|
|
Violation of the prostatic capsule during the TURP procedure results in absorption of fluid into _____________?
|
venous sinuses
|
|
|
Na lower than 120meq/ml will produce all the following signs and symptoms except:
1. CNS symptoms 2. HA 3. Irritability 4.Confusion 5. Absence of P waves 6. Possible widening QRS |
5. Absence of P waves.
|
|
|
ECG changes, wide QRS, ST elevation, nausea, somnolence can be found in what level of Na?
|
Na level lower than 115meq/ml
|
|
|
Na level of 100meq/ml can lead to:
|
VT or VF, seizure, coma
|
|
|
True or False:
Symptoms of low Na is related to acuteness of changes |
True
|
|
|
True or False:
In GU patients, Na+ and osmolality should be reported separately |
False-They should be reported together.
|
|
|
It is important to monitor the patient's ECG and blood pressure during ESWL?
|
Yes, The ECG must be of good quality because the R wave is used to trigger the shock. (Naglehout, p 718)
|
|
|
What are the most common dysrhythmias seen with ESWL?
|
PVC's and supra ventricular premature complexes. (Naglehout, p718)
|
|
|
List respiratory issues with ESWL
|
Increased work of breathing
Decreased FRC and VC |
|
|
List CV issues with ESWL
|
Hypotension d/t vasodilation
Cardiac arrythmias Hypotension after removal from bath |
|
|
What are advantages of current lithotripters?
1. Pads are gel-filled 2. Only need one treatment 3. Decreased need for anesthesia 4. Machines aren't as powerful |
1, 3 and 4 true
2. false - may need repeated treatments |
|
|
True or False:
BBB is permeable to solutes >8angstoms |
False-It is impermeable to solutes >8 angstoms.
|
|
|
True or False:
GU patients have problem with hyperosmolality in brain cells |
False: False-their problem is hypoosmolality in brain cells.
|
|
|
Treatment of low Na+ include all except:
1. Early recognition and diagnosis 2. Fluid restriction 3. Diuretic 4. Supportive treatment 5. 5-10% saline at 100ml/h or less |
5. 5-10% saline at 100ml/h or less(correct concentration is 3-5% saline)
|
|
|
ESWL stands for:
|
Energy Sound Waves Lithotripsy
|
|
|
Match the following with the indication:
1. Laser lithotripsy___________ 2. ESWL______________ a. For stones in the kidney or upper 2/3 of ureters b. For stones in the lower ureter |
1b.
2a. |
|
|
Current lithotripters:
>___-_____ pad rather than _____ >Most not as _________ >May need ______ treatments >________ need for anesthesia |
Current lithotripters:
>Gel-filled pad rather than water >Most not as powerful >May need repeat treatments >Minimizes need for anesthesia |
|
|
Current lithotripters procedure:
>__________ to locate stone >___ shocks/min >_____-______ shocks per treatment >Lasts __-__ minutes >___ sufficient |
Current lithotripters procedure:
>Fluroscopy to locate stone >120 shocks/min >2500-4000 shocks per treatment >Lasts 30-60minutes >MAC sufficient |
|
|
To avoid cardiac arrythmias ESWL shocks are timed to occur ___ _____ after the __ wave.
|
To avoid cardiac arrythmias ESWL shocks are timed to occur 20 msec after the R wave.
|
|
|
General ESWL complications include:
|
Cardiac arrythmias
Flank Pain Hematuria Bruising Soft tissue swelling Pulmonary Contusions Pancreatitis |
|
|
Anesthetic Implications of ESWL
|
Pt must be immobile
Water bath requires GA or regional Sedation adequate for modern lithotripters |
|
|
6 common GU procedures
|
1.cysto
2.TURP, TURBT 3.Retrograde pyelogram 4.Ureteroscopy 5.Ureteral stent inseration 6.Lithotripsy |
|
|
How long does a cystoscopy usually last?
|
5-30 min
|
|
|
Purpose of cystoscopy
|
examination of the bladder
|
|
|
Cysto is always therapeutic.
T or F |
False can be just for diagnosis
|
|
|
Cysto bladder is distended with fluid.
T or F |
True
|
|
|
Two type of scopes used for cysto
|
rigid or flexible
|
|
|
What type of topical is generally used injected into urethra for cysto?
|
2% Lidocaine
|
|
|
Amt of Lido for cysto for male?
Female? |
Male 15-30 ml
Female 3-5 ml |
|
|
General anesthesia for cysto?
|
Any agent. Adjust to pt comorbidites
|
|
|
GA for cysto always use LMA
T or F |
False may use mask
|

