![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
147 Cards in this Set
- Front
- Back
|
measures the extrinsic and common factors -deficiency of a clotting factor will prolong time -vitamin K deficiency will prolong the time |
Prothrombin Time PT |
|
|
Partial Thromboplastin Time. Two disorders that have prolonged PTT |
Hemophilia A (8) and B (9) |
|
|
EDTA from blood reacts with platelets an causes them to lyse |
pseudothrombocytopenia |
|
|
used to evaluate conditions such as renal artery stenosis and DVT |
duplex angiography |
|
|
assessment of arterial blood flow in client with peripheral vascular disease |
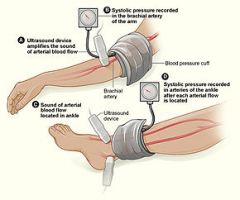
ankle-branchial index |
|
|
helps distinguish between primary and metastatic tumors |
bone marrow |
|
|
the lowest detectable concentration of anaylate that can be measured with some defined certainty or the rate of change of signal intensity as analytic concentration changes |
Analytic Sensitivity |
|
|
the extent to which other substances in the test system interfere with measurement of the analysis of interest |
Analytic specificity |
|
|
best indicator of how the bone marrow is responding to a bleed |
Reticulocyte count |
|
|
used to identify hemoglobinopathies |
Hemoglobin electrophoresis Isoelectric focusing HPLC Capillary zone electrophoresis |
|
|
Proteinuria and hematuria may be clues to________ as the case of blood loss or decreased epo production |
Renal disease |
|
|
Normal range for MCH Too high?? Too low?? |
27-32pg hyperchromic hypochromic |
|
|
Most common reason for iron deficiency anemia in adult |
chronic GI blood loss secondary to PUD, NSAID use, or cancer |
|
|
Lab Values of Patient X: 1. HCT low 2. HgB low 3. RC low 4. Smear: hypochromic, microcytic, angiocytosis, poikilocytosis 5. Serrum Ferritin: 11ng/ml |
Iron deficiency anemia Serrum Ferritin under 12 will give it away. |
|
|
Pt with weakness, malaise, lightheadedness, & pallor and other health problems. Smear: normochromic, normocytic RC: normal Serum ferritin: normal |
Anemia of Chronic Disease Tx: treat underlying disease possible tx EPO |
|
|
A patient who has microcytic hypochromic anemia, normal RBC, reticulocytosis, palor, and splenomegaly |
Thalassemia |
|
|
Main stay diagnostic test for Thalassemia |
Hemoglobin Electrophoresis variable amounts of HgF and hemoglobin A BETA Thal: elevated levels of HgB A2 or F |
|
|
Treatment for which type of thalassemia in includes -folic acid supplementation -avoiding iron and oxidative drugs |
Hemoglobin H |
|
|
The txt for B thalassemia major |
-Stem cell transplant -regular transfusions to keep HgB above 12 -folic acid supplementation -Defarasirox: prevents life threatening organ damage from iron overload |
|
|
A patient with skin darkening, sider blast cardiomyopathy, hepatitis, fibrosis, and cirrhosis and endocrine disorders likely is dealing with what condition. |
Iron Overload Secondary condition due to Thalassemia |
|
|
Bart's Hemoglobin is associated with stillborns and what type of Thal? |
Hydrops Faetalis -"Alpha major" |
|
|
Most common type of B12 deficiency |
pernicous anemia women 35 or older |
|
|
Pernicious anemia is caused by an decrease of ____ that is used for b12 absorption. |
intrinsic factor |
|
|
A pt who is homozygous for beta thalassemia will get enlargement of bone marrow with bony deformities of the skull and face, long bones, and spine |
Cooley's Anemia B thal Major |
|
|
Pt that are compound heterozygotes for two different beta global chain mutations and have a disease that is intermediate in severity between thalassemia minor and beta thalassemia major |
Beta thallasssemia intermedia |
|
|
Pt with the following lab values: DDX 1. MCV 120 2. HCT: 43 3. RC: 1 Metabolic studies: 1. RBC folate: normal 2. serum folate: normal 3. Serum b12: low 4. MMA: high 5. homocysteine:high Smear megoblastic hypersegmented neutrophils (more than 4) |
B12 Deficiency vitamin b12 is not present RC: Low megoblastic MMA and homocysteine are high. |
|
|
Old school test used to determine B12 deficiency using radioactivity and urine |
Schilling test |
|
|
Diagnostic test for B12 deficiency |
bone marrow biopsy -marked erythroid hyperplasia -megoblastic changes -giant bands of metmyelocytes |
|
|
TX B12 deficiency |
vitamin B12 supplement -folic acid supplement for several months until B12 replaced |
|
|
The anemia that present with neurologic symptoms: 1. parathesia 2. balance and gate problems 3. decreased vibration and positional sense 4. confusion and dementia |
B12 Deficiency: Severe |
|
|
Pt history: Alcoholic, anorexia, lack of fruits and vegetables, or over cooking them DDX? |
Folic Acid Deficiency MC: dietary problem |
|
|
Macrocytic anemia, megoblastic smear, normal serum ferritin levels, reduced folic acid, normal vitamin B12 levels. |
Folic Acid Deficiency |
|
|
A patient reports having weakness, lightheadedness, and palor. He says he has a weird sour mouth and sores on the sides of his mouth. He also notices that he is bruising easily. What would you do? |
DDX: Folic Acid Deficiency Order labs, 1. CBC + differential +peripheral smear 2. order metabolic study Macrocytic anemia Reduced folic acid levels in RBC or serum normal serum vitamin B12 levels |
|
|
Definitive diagnostic test for Sickle cell anemia |
Hemoglobin Electrophoresis Hemoglobin S present in 50% greater in SSA |
|
|
Treatment for sickle cell |
Systematic care folic acid supplementation hydroxyurea transfusions during crisis Low dose penicillin from birth to age 6 due to spleen problem Vaccine PNA and influenza PFT |
|
|
a patient with sickle cell should avoid high altitude and deep sea diving. Why? |
to prevent hypoxemia |
|
|
acquired hemolytic anemia caused by IgG autoantibody |
Warm Autoimmune hemolytic |
|
|
Positive ANTIGLOBULIN coombs test is indicative of what disorder? |
Warm Autoimmune hemolytic |
|
|
TXT for Warm AIH |
prednisone |
|
|
A pt comes to the office with rapid onset of fatigue, SOB, angina, jaundice, spleenomegally, fever and dark colored urine. You run a CBC and is is normal. The blood smear shows reticulocytosis and sherocytosis. The serum direct bulirubin test is high. |
Think: hemolytic Warm autoimmune hemolytic anemia |
|
|
IgM autoantibody directed antigen of RBC reacts with cells at low tempature. RBC then sequestered and lysed in the liver. |
Cold Agglutinin |
|
|
A pt present with mottled or numb fingers or toes. Episodic back pain. dark colored urine. Smear shows agglutinated RBC, reticulocytosis, and spherocytosis. |
Cold agglutinin hemolytic anemia |
|
|
The anti globulin (COOMBS) test is postive ONLY for complement proteins in which disorder |
Cold Agglutinin **cold agglutinin titer will also be positive |
|
|
episodic hemolysis in response to oxidant drugs or infections |
G6PD x-linked |
|
|
G6PD MC in what population |
males: X-linked MC: tropical and subtropical zones in the eastern hemisphere American Black men |
|
|
The presence of Heinz bodies. Which are HgB that has precipitated out into cytoplasm causing premature remove via spleen. Indication of what disease? |
G6PD Deficiency |
|
|
A patient who is having periods of episodic anemia without splenomegaly. The provider performs a peripheral smear and finds bite cells, blister cells, and heinz bodies. HMMM??? |
G6PD |
|
|
Aspirin, dapsone, primaquine, quinidine, sulfonamides, nitrofurantoin, fava beans all fall under what category? |
Oxidative Drugs! Don't give to people with Hemoglobin H disease or G6PD |
|
|
Depletion of stem cell lines by any agent (drug) or even (radiation) |
Aplastic anemia |
|
|
The following lab results indicate what type of disorder? 1. pancytopenia 2.normacytic --> macrocytic 3. leukopenia 4. reticulocytopenia 5. unremarkable blood smear 6. Bone marrow: hypocellular |
Aplastic Anemia |
|
|
A patient with mild aplastic anemia treatment option |
supportive care EPO RBC platelet transfusions when necessary Abx for infection |
|
|
A young person with SEVERE aplastic anemia may be given? |
bone marrow transplant Not for adults over 40yo |
|
|
A patient comes to the office with bone pain, enlarged liver, and spleen. You run labs and get the following report. pancytopenia, reticulocytosis, and an unremarkable peripheral smear enters the office. What do you think? |
The labs make you think aplastic anemia. The bone pain r/o aplastic anemia and you should be thinking CANCER |
|
|
Very slowly progressive bone marrow disorder characterized by increased number of RBC and increased total blood volume |
Polycythemia Vera |
|
|
Mutation most likely found in a pt with Polycythemia Vera |
Jak2 |
|
|
A 66 year old male patient patient presents with headaches, dizziness, blurred vision due to retinal engorgement, and fatigue. He also complains that after a bath he gets a very weird itchy red rash. You decided to run a CBC and blood smear. What results would you expect? If you ran an ABG, what you expect. |
Polycythemia Vera -HCT higher than 54% Smear: -neutrophil leukocytosis -increased basophils and eosinophils -increased number of large platelets Normal arterial O2 saturation |
|
|
Three most common reasons for neutropenia |
1. infection: bacterial, fungi, viral TB, malaise 2. Drugs: MC: corticosteroids, PCN, Cephalosporins, sulfas, quinidine 3. Autoimmune: analogy of autoimmune hemolytic anemia: Crohns, SLE, RA,hodkins |
|
|
neutropenia with rheumatoid arthritis and splenomegaly |
Felty syndrome my joints FELT bad. TX: splenectomy or sustained myeloid growth factors |
|
|
A reaction to infection, inflammation, and physiologic stress could cause |
leukocytosis |
|
|
Why would hyper leukocytosis increase morbidity and mortlity? |
Traffic jams! too many cells the higher the blood count the higher the mortality rate. |
|
|
Cells that work to control parasites and mediate allergic reactions. MC: allergies and drug hypersensitivity, uticaria |
Eosinophilia low frequency in differential |
|
|
Least abundant of circulating cells. Active during allergic reactions, inflammation, release histamine |
Basophils |
|
|
Provides the sustained response to an infection. Largest cell in the blood |
Monoctyes **in tissue: macrophages** |
|
|
rapid response to an infection. 1st line defense against bacteria or fungi |
Neutrophils (54-62%) |
|
|
create antibodies against bacteria, viruses, and foreign and malignant cells coordinates and executes immune system |
Lymphocytes (25-33%) |
|
|
slower, more sustained response to infection and inflammation |
monocytes |
|
|
resolution of an acute infection done by which cell |
monocytes |
|
|
attack parasitic and allergic infection chronic inflammation/cancer asthma |
Eosinophils 1-3% |
|
|
release histamine in response to Allerghic/inflammatory conditions Release heparin |
Basophils |
|
|
A red streak from wound or area of cellulitis towards regional lymph nodes, which are usually tender and enlarged |
lympangitis |
|
|
A pt comes to your office 5 days after cutting her finger with a knife. She has fever, chills, malaise and anorexia. She noticed a red streak on her arm developing yesterday, it seem to be traveling up her arm. What would you expect from a CBC? What would you expect from a blood culture? What do you think it is? |
CBC: leukocytosis with left shift and many neutrophils Culture: S. aureus or Hemolytic strep LYMPHANGITIS (channel) |
|
|
A 42yo women who has had a left sided mastectomy complains of painless, yet persistent edema on her left arm. You touch her leg and notice some pitting edema. 1 What is happening? 2 How can she treat it? 3 If it is severe, what types of diagnostics may you choose to run? |
1 Lymphedema 2 elevation, elastic compression stockings, massage toward the trunk Intermittent diuretics 3 lymphangiography and radioactive isotope studies to identify focal defects in lymph flow |
|
|
A pt presents with fatigue, fever, and bleeding from the gums. He complains that his bones have been hurting and that last week he had this weird bloody rash on his trunk. You begin to think he may have leukemia. What would you do? |
Run a CBC & peripheral smear and look for pancytopenia with circulating blasts. If positive for blasts, do a bone marrow biopsy look for more than 20% blasts and hypocellular Other tests: hypouricemia, serum fibrinogen (low), PTT prolonged, D-dimer present. |
|
|
If you suspected a pt to have meningeal leukemia. What test would be diagnostic? |
Spinal tap Blasts in the CSF |
|
|
A peripheral smear in a patient with suspected leukemia contains auer rods. What should that alert you to? |
AML "eosinophilic needle like inclusions on the cytoplasm" |
|
|
Median age for diagnosis with AML |
60 |
|
|
Myeloid proliferative disorder characterized by overproduction of myeloid cells |
Chromic myleogenous leukemia |
|
|
A 53yo female presents with fatigue, night sweats, low grade fever, and a weird abdominal fullness. She notices that her chest is really tender right at her sternum. You run a CBC and notice her WBC is elevated at 180,000/mcL. What can you conclude? How would you treat? |
1. abdominal fullness is splenomegaly 2. She could have CML. Sternal pain! If CML is confirmed: Watchful waiting until WBC get to over 200,000/mcL |
|
|
A patient that was diagnosed with CML 7 years ago suddenly has a jump in WBC to 250,000/mcL. You assume that she has jumped from the acute phase to the accelerated/blast phase. What would you expect to see on a CBC and bone marrow aspiration? |
1. anemia 2. thrombocytopenia 3. pancytopenia 4. blasts in blood and bone marrow increase 5. Bone marrow: hyper cellular with left shifter myelopoesis Diagnostic: blasts in 20% of bone marrow |
|
|
Which type of leukemia is most common in children? What age? |
ALL 3-7 |
|
|
A 5 child had PNA and his pediatrician had a chest x-ray performed. Incidentally, a mediastinal mass was noticed on the chest X-ray. Instantly, you think back and remember that the child was pale and had been complaining about growing pain. Your heart sinks because you think he may have? |
ALL mediastinal mass! pallor bone pain |
|
|
A child with ALL has genetic testing done and is determined to have the Philadelphia chromosome. What is the prognosis for the child? What treatment should you start? |
ALL + philadelphia = unfavorable combination chemotherapy |
|
|
Which leukemia do 90% of the cases happen at the age of over 50? |
CLL |
|
|
A 66 yo patient notices that he has been getting sick a lot lately and feels very tired. You decide to run a CBC and the B-cell lymphocytes are high at 7000/mcL. You start to think he may have CLL. You do a bone marrow biopsy and what would you find? |
bone marrow will be infiltrated with small lymphocytes |
|
|
While taking a shower a women notices a round lump in her groin area, it is painless. The next morning, she weighs herself and she has lost 12 lbs without trying. She chalks it up working out at the gym. That night, she can't sleep because her sheets are soaked with sweat. She begins to get nervous that something is wrong. She calls her PCP and says to come in immediately. Why? |
The painless round lump sounds like lymph node swollen, lypmadenopathy. The weight loss and night sweats are constitutional symptoms. Concern that she could have non-hodgkin lymphoma. |
|
|
a variety of lymphocyte cancers with variable presentation and course |
Non-hodgkins lympoma |
|
|
A provider suspects a pt has non-hodgkins lymphoma. What should he order? |
Tissue biopsy: via needle aspiration Full body PET scan CBC + differential + smear smear: normal |
|
|
A pt notices a painless node on her neck. Three weeks later, she notices another painless node about three cm below it. She begins to worry and contacts the doctor. The nodal progression here is indicative of what type of lymphoma? How would a pathological diagnosis be made? What would be found on a peripheral smear? |
Hodgkins lymph node biopsy reed steinberg cells |
|
|
malignancy of the hematopoetic stem cells terminally differentiated as plasma cells |
multiple myeloma |
|
|
monoclonal papaprotein by serum or by urine protein analysis, replacement of bone marrow, and bone destruction are all indicative of |
multiple myeloma |
|
|
a patient with clonal plasma cells in the bone marrow or in a tissue biopsy or both. |
multiple myeloma |
|
|
A tissue smear that is normal but has Rouleuax formation. Hypercalemia proteinuria |
Multiple myeloma |
|
|
Treatment for Multiple Myeloma |
1. Lenalidomide or thalidomide + high dose dexamthasome 2. avoid immobilization and dehydration 3.treat hypercalcemia 4. autologous stem cell transplant: may be curative, but risky |
|
|
Low platelet count |
Thrombocytopenia |
|
|
MC metabolic laboratory finding in a patient with thrombocytopenia |
Vitamin B12 deficiency |
|
|
treatment for ITP |
prednisone if fail: IVIG if fail: splenectomy |
|
|
A person with platelet levels in the 20-30,000/mcL will likely be experiencing |
spontaneous bruising, nosebleeds, hemorhhage |
|
|
In any patient over 60yo, you should perform what test before you diagnosis them with ITP |
bone marrow biopsy |
|
|
The pathognomonic pentad for what disease? 1. microangiopathic hemolytic anemia 2. thrombocytopenia 3. fever 4. renal failure 5. neurologic symptoms |
TTP |
|
|
microagniopathic hemolytic anemia and thrombocytopenia in the absence of another plausible explanation |
Thrombotic Microangiography |
|
|
Treatment for Thrombotic Microangiography |
Immediate Platelet Exchange **can use fresh frozen plasma if platelet exchange not available **NO NO NO platelet transfusion |
|
|
The major risk in HIT |
thrombosis in 50% of the patients, bleeding uncommon |
|
|
thrombocytopenia within 5-10 days of exposure to heparin |
Thrombocytopenia |
|
|
HIT pathophysiology |
formation of IgG antibodies to heparin platelet factor 4 (PF4) complexes; antibodies bind platelets, which activates them. Platelet activation leads to both thrombocytopenia and pro-thrombic state |
|
|
A patient who had taken IV heparin 7 days ago now how a platelet count that is 50% of his baseline. What should you do? |
Assume HIT 1. stop all heparin 2. Give direct thrombin inhibitor: Argatroban & bivalrudin- continue until platelets recover 3. start Vitamin K antonist (warfarin) 4. stop when INR warfarin 2:3 |
|
|
thrombocytopenia decreased fibrinogen levels consumption of clotting factors and platelets that leads to bleeding |
DIC Disseminated Intravascular Coagulation |
|
|
Describe the progression of platelets and fibrin as DIC progresses. |
early: platelet and fibrin are normal progressive: thrombocytopenia later: serum fibrinogen low |
|
|
A person with DIC will have what definitive lab results |
Prolonged PTT and PT time D-dimer increased (not specific) plasma smear: schistocytes |
|
|
A patient was admitted to the hospital with sepsis 3 days ago. suddenly, he being bleeding out of his IV catheter and other areas of the body. What might this be? What would you do? |
DIC treat sepsis! fresh frozen plasma if severe bleeding platelet transfusion CI: heparin if platelet count is low |
|
|
mutation in JAK2 that increases the production of RBC, WBC, and platelets |
Essential Thrombocytosis (same mutation as Polycythemia Vera) |
|
|
elevated platelet count in the absence of other causes Normal red blood count mass |
essentail thrombocytosis |
|
|
painful burning of the hand accompanied by erythema is called? What condition presents with it? |
Essentail thrombocytopenia erythromelalgia |
|
|
A pt with essential thromboctyosis has a bone marrow biopsy and peripheral smear. What would be expected? |
marked proliferation of megakaryotype in the bone marrow large platelets |
|
|
Treatment for essential thrombocytosis |
1. control cardiovascular risk 2. control platelet count: hydroxyurea 3. Aspirin to reduce risk of thrombosis 4. plateletphoresis |
|
|
The burn out phase of the bone marrow is |
when bone marrow becomes fibrotic and scared over due to too much use essential thrombocytosis |
|
|
Recurrent hemarthrosis and arthropathy |
Hemophilia A and B |
|
|
A patient with hemophilia can become resistant to exogenous clotting factors due to treatment. Thus, they can no longer be supported by factor 8. What % of pts? |
15% |
|
|
Hemophilia A and B clotting factors inheritance pattern |
8 and 9 x linked |
|
|
most common inherited bleeding disorder |
von Willebrand disease |
|
|
treatment for von Willebrand disease |
DDAVP |
|
|
cramping pain or tenderness or pain in the calf with exercise. Reduced popliteal and pedal pulses foot pain at rest |
Femoral and popliteal arteriosis |
|
|
severe pain of the forefoot that is relieved by dependency pain or numbness when walking ulceration or gangrene of the foot pallor in foot when walking |
tibial and pedal arteriosis |
|
|
dilated tortuous superficial veins in the lower extremeties |
varicose veins |
|
|
induration, redness, and tenderness along a superficial vein, usually the saphenous vein |
superficial venous thrombophlebitis |
|
|
edema, stasis (brawny) skin pigmentation, sub liposclerosis in the lower leg above the ankle |
chronic venous insufficiency |
|
|
A 66yo male presents to the ER with cramping pain in his leg and calf. He has a history of smoking and says that the severity of his pain changed chilly. When he sits down, he feels relief. He has a diminished femoral use. You suspect an occlusive dz of aorta and iliac arteries. You order a doppler. What result should you get? Explain the dx. How would you treat? |
1. The ratio of systolic blood pressure at the ankle compared with brachial artery of upper arm is reduced below .9. 2. Calf pain, smoking history, relieved when sitting. Diminished femoral pulse. 3. If signs of clotting, use TPA. Visible clot remove via mechanical mechanism. |
|
|
A woman reports that walking 3-4 blocks to get her mail has become challenging. She is having tenderness in her calf when she exercises. She also notices that her right calf has atrophied. What dx. Her PCP performed a ABI and the results were .5. What surgical intervention may be plausible for her. |
Femoral -popliteal bypass with autogenous saphenous vein |
|
|
A pt with severe pain of the forefoot that is relieved by dependency. |
Tibial and pedal artery disease *dangling foot over edge of bed relieves pain |
|
|
dilated and tortuous superficial veins in the lower extremities |
Varicose veins |
|
|
Mainstay for diagnosing varicose veins |
duplex angiography |
|
|
Management of varicose veins |
-compression stockings -elevation -endo-venous ablation -radiofrequency or laser ablation |
|
|
Induration, redness, and tenderness along a superficial superficial vein, usually saphenous vein |
Superficial venous thrombophlebitis |
|
|
Dysphagia in an iron deficient person due to esophageal webs |
Plummer Vinson Syndrome |
|
|
Gold standard for the diagnosis of anemia of inflammation |
bone marrow biopsy with iron stain |
|
|
Which two anemias are considered megoblastic? |
Folic Acid and vitamin B12 |
|
|
Haptoglobin is a protein produced by the liver. It attaches to a certain type of hemoglobin in the blood. |
Haptoglobin attaches to this released hemoglobin, which is also called "free" hemoglobin. Free hemoglobin is not contained within red blood cells. The level of free hemoglobin is usually very low. But it rises when red blood cells are dying |
|
|
schistocytes are fragmented RBC. In what diseases are they found? |
TTP and DIC |
|
|
Why do you start the Positive PF4 heparin antibody enzyme-linked immunosorbent assay by ELISA along side the Serotonin release assay in a pt with HIT? |
PPF4 takes 24 hr Serotonin takes 4-5d May use PPF4 to RO HIT, but if positive start pt on anticoagulants empirically |
|
|
a severe form of DIC in peripartum women that results in hemolysis, elevated liver enzymes, and low platelets. The treatment is evacuation of the uterus |
HELLP Syndrome |
|
|
a malignancy related to DIC |
Troussau |
|
|
A type of thrombocytopenia that is similar to TTP but is found primarily in children and adults exposed to toxigenic Eschericha coli O157:H7, salmonella, and shigella. TX: |
HUS **has more renal problems **tx: emergent plasma exchange |
|
|
measures the integrity of the intrinsic system (Factors XII, XI, VIII, IX) and common clotting pathways. |
PTT |
|
|
specifically evaluates the presence of factors VII, V, and X, prothrombin, and fibrinogen |
PT |
|
|
increased hepcidin levels, which block the iron absorption from the gut and the ease of iron from bone marrow are characteristic of what disease? |
Anemia of chronic disease Specifically: Chronic Inflammation |
|
|
The pneumonic HIT stands for Hereditary, immune attack, and trauma. What diseases are realted to each. |
Hereditary: G6PD, thalassemia, sickle cell Immune attack and Trauma TTP, HUS, DIC |
|
|
An elevated Retic count in the presence of falling HgB are hallmarks of |
Hemolytic anemia |
|
|
A peripheral smear with howell jowell bodies |
Sickle Cell Anemia |

