![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
pancreatic functions exocrine
|
Proteolytic: Proteases
trypsinogen chymotrypsinogen Procarboxypeptidase Amylolytic: Amylase Lipolytic: Lipase/prophospholipase A2 water electrolytes: HCO3 |
|
|
where esle is amylase also found beside the pancrease
|
saliva
|
|
|
endocrine asspects of the pancrease
|
Insulin (Beta Cells)
Glucagon Somatostatin the hormones result in systemic effects as compared to the exocrine functions of the pancreas |
|
|
acute pancreatitis
|
mild-severe inflamation
generally reversible exocrine and or endocrine function rarely progresses to chronic |
|
|
chronic pancreatitis
|
longstanding pancreatic injury
fibrosis/destruction of tissue irreversible exocrine and or endocrine function from multiple injuries to the pancreas over a good amount of time |
|
|
what is the distinguishing feature of chronic pancreatitis vs. acute
|
preminent dysfunction of the exocrine and endocrine properties of the pancreas in chronic
|
|
|
pathophys of acute pancreatitis
|
inital insult--> realease of active enzymes within the pancreas (autodigestion)--> release of cytokines, vasoactive substances--> inflammation, ischemia, tissue damage/death
local affects in addtion to systemic |
|
|
clinical features of pancreatitis
|
Abdominal Pain***
Epigastric, severe: Sharp or “knife-like” Radiation to back Abdominal distention Nausea/vomiting: inflammtion in the area is causing 5HT realease which is causing the N/V Fever : not due to infection, but an imflammatroy response Jaundice: because bile acids are obstructed and therefore go systemically because fo the inflammation |
|
|
clinical features of pancreatitis
|
Severe
Shock, MS changes, ARDS, SIRS, AKI Lab abnormalities Alterations in glucose Na/K if N/V present Increased ALT/AST: because of gallstones Local Complications: Necrosis (15%) Hemorrhage Abscess or infection Pseudocyst |
|
|
during pancreatitis what are the lab abnormalities
|
increase in glucose
decrease in Na/K if N/V present increased ALT/AST because of gallsotnes (this can be confused as hepititis) |
|
|
local complications of pancreatitis
|
Necrosis (15%)
Hemorrhage Abscess or infection Pseudocyst |
|
|
abscess
|
walled off defined area of fluid
|
|
|
psedocytes
|
are typical of chronic pancreatitis
form from local inflammation the area becomes walled off area of fluid but no epithilial lining (need to be surgically removed) |
|
|
diagnosing pancreatitis
|
Imaging (Ultrasound, CT)***
Laboratory***** Amylase Rises 2-12 in hours, persists for 3-5 days Interference from other disease states and bodily sources (e.g. _saliva_) Lipase Peaks at 24 hrs; normalizes in 8-14 days More sensitive and specific marker |
|
|
can you diagnosis pancreatitis by just looking at a patient
|
no
|
|
|
what are the most significant symptoms of pancreatitis
|
pain
N/V |
|
|
what enzyme is more diagnostic for pancreatitis
|
lipase
local inflammation is causing a release of activated enzymes released into the bloodstream, which causes lots of damage |
|
|
etiologies of acute pancreatitis #1 cause
|
alcohol over a long time
direct to toxicty |
|
|
what % of cases of pancreatitis are caused by alcohol
|
80%
|
|
|
#2 cause of pancreatitis
|
gallstones
obsturcts ducts the rate of this type of pancreatitis is rising and getting close to alchol caused pancreatitis becasue the risk factors for gallstones are increasing |
|
|
iartogenic pancreatitis
|
Endoscopic retrograde cholangiopancreatography (ERCP) (~5%)
ERCP is a diagnostic test that is used to treat gallstones, but can also cause them |
|
|
more diagnostic features of pancreatitis
|
Hypertrigylceridemia mayinterfere with enzyme assays for amylase, intraqbdomial inflammation can increase amylase, also elevated in renal failure (25% cleared by kidney)- want at leat 2-3 X elevations
Alcoholics may not have as high of a rise due to a burned out pancreas Increase ALT > 3X ULN C/W gallstones(low sensitivity) lipase can also be affected by intra-adominal inflammation and renal failure pancreas contains ~ 4.5 x more lipase than amylase |
|
|
idiopathis of drugs percentage of pancreatitis causes
|
10-30%
|
|
|
how long and how much alcohol does it take to cause pancreatitis
|
large quantities >1-2 drinks/day over a period of 8-10 years
|
|
|
risk factors for gallsotnes
|
Increasing age
Female (3:1) Pregnancy or estrogen use (increases risk 2-3 times) Extensive ileitis or ileal resection Obesity Rapid weight loss (gastric bypass surgery) Caucasian, Native American Prolonged total parenteral nutrition (because the gallbladers cue to contract is food, fat and nutrients, coming from the stomach, so it is not being stimulated) |
|
|
Cholelithiasis =
|
presence of gallstones in GB
|
|
|
gallstone composition
|
lipids (cholesterol)
vs. bilirubin +/- glycoproteins |
|
|
acute pancreatitis causes
|
Toxins
Scorpion venom, insecticides Trauma ERCP is often placed in this category Blunt trauma Triglycerides > 500 (usually above 1000) Ischemia |
|
|
accute pancreatitis caused by what structural abnormalities
|
Pancreas divisum (congenital)
Tumors |
|
|
what infections can cause acute pancreatitis
|
Bacterial: tuberculosis
Viral: HIV, Hep A/B/C, varicella, CMV Parasitic: ascaris worms (not all that common in US, but it is a parasite that lives in the GIT) |
|
|
drug-induced pancreatitis
|
> 100 drugs implicated
Rarely cause chronic pancreatitis Issues Most are case reports/series Definite associations are difficult to establish Manifestations are same as non-drug causes Can’t predict who will develop Often do not want to rechallenge patient |
|
|
Drug-Induced Pancreatitis mechanisms
|
Hypersensitivity
Direct toxicity Accumulation of toxic metabolites Pancreatic duct constriction Changes in osmotic pressure within the pancreas Induction of intrapancreatic thrombosis approximatley 2% of cases |
|
|
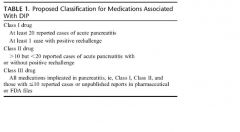
definite drug association and proposed classifications for medications that cause pancreatitis
|
|
|
|
Common drugs that cause pancreatitis
|
azathioprine
valporic acid measalamine various estrogens (premarin) opiates steroids furosemide (hypersensitivity) hydrocodone/apap |
|
|
general managment strategies for pancreatitis
|
Stop oral intake (i.e. make NPO)
Decreases stimulation of pancreas Possible NG suction Transition slowly to oral food/liquid Treat Pain and N/V Hydration Electrolyte replacement Remove offending agent(s) |
|
|
list of general managment strategies for pancreatitis l
|
Pain management
Antiemetics Acid suppressants Antibiotics Octreotide Nutritional support |
|
|
pain management for pancreatitis
|
Goal: Relief of Abdominal pain
Narcotic Analgesics Morphine Hydromorphone (Dilaudid®) Fentanyl (Sublimaze®) Meperidine (Demerol®) Patient Controlled Analgesia (PCA) |
|
|
what narcotic should be avoided in pancreatitis
|
meperididne
it is highly addictive and has an acive metabolite that is CNS toxic (seizures) renal dysfunction makes the toxic metabolite accumulate even more |
|
|
what is the number one drug of choice for pain treatment in pancreatitis
|
narcotics
they can cause pancreatitis, but we do not deny them |
|
|
narcotic controversy and pancreatitis
|
Possible spasm of sphincter of oddi
Increases in abdominal pain secondary to increased pressure in biliary tract Increases in amylase/lipase Morphine most commonly cited Questionable clinical significance Outcomes are generally not affected all narcotics can cause this but it is not clinically significant |
|
|
N/V treatment and pancreatitis
|
Antiemetics
May be given scheduled or as needed Use IV or PO dose forms as initial therapy Phenothiazines (promethazine) Serotonin antagonists (ondanstotran) |
|
|
nutritional support in pancreatitis
|
Nutritional deficits may develop rapidly in severe cases
Consider if > 1 week NPO anticipated TPN vs. Enteral Feeding TPN Higher rate of: infection Gallstones Hyperglycemia ? Effects on mortality |
|
|
enteral feeding and pancreatitis
|
Benefits in severe acute pancreatitis
Aids in mucosal repair Prevents bacterial translocation Reductions in: Infectious complications (sepsis) Need for surgery Length of stay Lower cost preferred route start slowly and gradual increases |
|
|
antibiotics and pancreatitis
|
Not recommended for routine use
May use in the setting of infected necrosis or abscess Target: Gram (-) intestinal flora Systemic Antimicrobial Agents Require adequate pancreatic concentrations Imipenem/cilastatin, Fluoroquinolone + Metronidazole Duration: 2-4 weeks → surgery |
|
|
octreotide and pancreatitis
|
Somatostatin analog
Mechanisms Suppression of pancreatic output ? Protective effect on pancreatic cells ? Improvement in water/electrolyte absorption Possibly effective for severe cases Dose: 0.1 mg SQ/IV TID rarely used it supresses pancreatic secretions rarely used |
|
|
somatostatin
|
a hormone secreted by the exocrine cells of the pancreas
|
|
|
other managment strategies of pancreatitis
|
Acid suppression
H2RAs or PPIs No proven benefit other than in stress ulcer prophylaxis (those in the ICU, on ventilation, anti-coag) Gallstone pancreatitis May use ERCP to remove/break stones Laparoscopic cholecystectomy (removal of the gallblabber causes the patient not able to digest fats so causes diarrhea) Ursodiol (Actigal®, URSO®) not effective for acute gallstone dissolution (6-12 mo) |

