![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
50 Cards in this Set
- Front
- Back
|
ACR Quality Defined as: |
The Right Procedure done in the right way, at the right time with the correct interpretation to maximize the desired health outcomes and to satisfy the patient. |
|
|
PQI Practice Quality Improvement Ongoing Organization Wide Framework to Monitor all aspects of an organization's activities for the purpose of continuous improvement. |
Goals of PQI -Improve Quality of Care for Patients -Reduce Error -Minimize Medical Legal Risk -Save Money |
|
|
PQI Practice Quality Improvement |
Important Components of PQI
-Break Down the Process Into Steps -Understand variation that may lead to error -Test on a small scale before implementing -Teamwork |
|
|
Implementing PQI:
PDSA Cycle |
PDSA Improvement Method four Steps:
1. Plan a test --- start small. 2. Do the test 3. Study the Outcomes of the test 4. Act on Knowledge Gained from test May do same test on larger scale. |
|
|
Measurement of Patient Dose? |
Patient Dose is Complex Radiation Dose Can Only Be Estimated. |
|
|
Air Kerma |
Formerly Called "Exposure" Air Kerma specifies the amount of radiation existing at a position in space (e.g., output of the CT Scanner) Unit of Air Kerma is Gray (Gy) or milliGray (mGy) Air Kerma is the Quantity Typically measured by imaging physicist. |
|
|
Absorbed Dose |
-Occurs When energy carried by an x-ray is transferred to kinetic energy of charged particles in the tissue as the x-rays pass through the tissue.-transferred energy may cause damage --Units: Gray (Gy) or milligray (mGy) --Absorbed dose is typically NOT directly measured. It is calculated from air kerma measurements. |
|
|
CTDI vol |
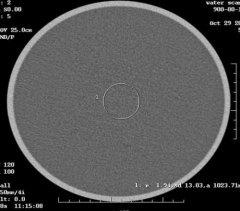
Absorbed dose given to 1 of 2 standard-sized plastic cylindrical phantoms by a CT scanner Units: Gray (Gy) or milligray (mGy) Imaging physicists use 1 of the 2 phantoms shown to make the measurements needed to calculate CTDI vol. Pediatric/Head (16 cm) or body phantom (32cm) |
|
|
CTDI vol Estimate of Patient Dose? |
CTDI vol is NOT estimate of patient dose CTDI vol is the dose to one of the CTDI phantoms. It allows comparison of the radiation output between CT scanners. |
|
|
More Dose at Center or Periphery of Phantom? |
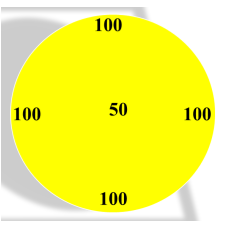
More Dose at Periphery of Phantom Average CTDI vol is 84 Surface dose is 2 times greater than the central dose CTDI vol is average of central & peripheral dose. |
|
|
CTDI vol in Neonate- under or over estimate? |
CTDI vol may underestimate a neonatal dose by over 200%.
Phantoms not accurate depiction of neonate |
|
|
CTDI vol of 16 cm phantom is same as CTDI vol of 32 cm phantom-- True/False |
False! Dose Estimates May Be off by factor of 2 if you use the wrong phantom.
ex: 20 mGy estimate dose based on a 16cm phantom = a 10 mGy dose based on a 32 cm phantom. |
|
|
CTDI vol measure radiation dose to patient.
True/False |
False! CTDI vol measure the radiation dose to one of the CTDI phantoms. It is NOT an estimate of patient dose, because it does not take into account patient size, patient shape, or the varying tissue attenuating factors of the human body and, therefore, it may significantly underestimate dose. |
|
|
Dose Length Product (DLP) |
DLP = CTDI vol x scan length (cm) |
|
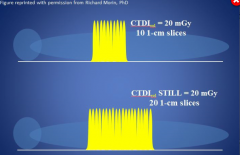
10 slices = 20 mGy CTDI vol
20 slices = 20 mGy CTDI vol |
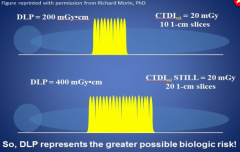
10 slices = 200 mGy/cm DLP
20 slices = 400 mGy/cm DLP |
|
|
DLP is indicator of patient dose.
True/False |
False! DLP, just like CTDI vol, is not indicator of patient dose.
Neither measurement accounts for changes in patient size, since both use dose delivered to 1 of 2 standard phantoms. |
|
|
With same technique (120kV, 200mA, 1 sec) Measured CTDI vol same with small phantom and large phantom? |
No!!!! Measured CTDI vol is 2.6 times larger with smaller phantom---- But the displayed CTDI vol is the the same. |
|
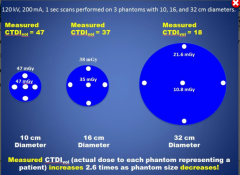
|
No!!!! Measured CTDI vol is 2.6 times larger with smaller phantom---- But the displayed CTDI vol is the the same. |
|
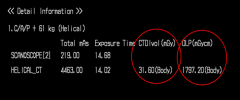
Estimates of Radiation dose on CT Console. |
CTDI vol (mGy) = 31.60 (body phantom)
DLP (mGym) = 1797.20 (body phantom) |
|
|
Confusion When Talking About Radiation Output (Estimate of Radiation dose)
Radiation Output-- Not Patient Dose! |
31.6 mGy CTDI vol32 x2 = 63.2 mGy CTDI vol 16
Remember these are not patient doses. Also depending on the size of the phantom, a conversion factor (2) may need to be used to correct from one CTDI phantom to the other. |
|
|
SSDE? |
SSDE = Size Specific Dose Estimate
Which takes into account the effect of the patient's size on their radiation dose.
SSDE is currently the best estimate of patient dose. |
|
|
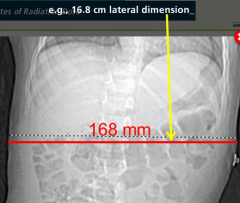
SSDE--Better estimate of patient dose Acurrate to within 10-20% Conversion factor is applied. NEED 4 THINGS: -Patient Size (lateral dimension) -CTDI vol phantom 16 or 32 cm -Conversion factor -Displayed CTDI vol from clinical scan |
|
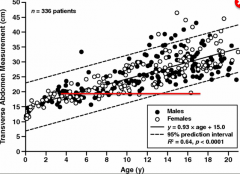
Largest 4 Y/O and Smallest 18 Y/O are the same size |
The Most Accurate Method to Estimate body Size is Patient Thickeness.
Avoid Using: -Age -Weight |
|
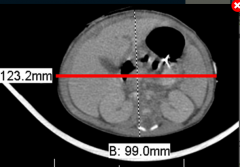
Red Line Demonstrates Lateral Width, and Dotted Line demonstrates (AP) dimension. |
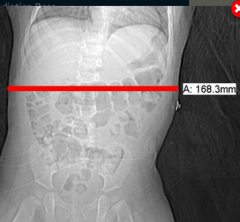
Patient size can be calculated from the projection before the scan or from the axial image after the scan. |
|
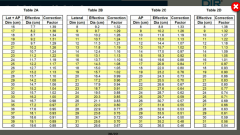
Look Up Table TG204 |
SSDE can be calculated from
- AP Dimension -Transverse or Lateral Dimension -AP + Lateral Dimension or -Effective Diameter |
|

|
One Factor That Influences Radiation Dose is Image Quality.
Image Noise is One Component of Assessing Image Quality. |
|
What is Image Noise? |
Image Noise Appears as the speckled Gray Background of a Uniform Phantom.
It is measured as the standard deviation of the voxel values in a homogenous (typically water) phantom. |
|
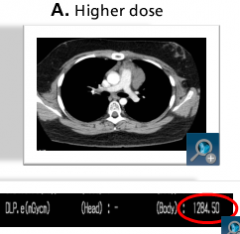
Higher Dose Exam DLP 1284 |
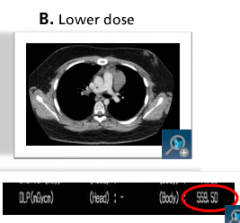
Lower Dose Exam DLP 559 Grainer Image But Diagnostic Much Lower "Dose" -Need Balance: Best vs Acceptable (Diagnostic) Image |
|

Target Level for CT Radiation Dose
What is DRL? |
Diagnostic Reference Levels (DRL)- are dose levels for typical examinations for groups of standard-sized patients or standard phantoms for different types of equipment. |
|
|
Diagnostic Reference Levels (DRLS) If site's CT > 75% percentile compared to peers, then local action should be triggered
True/False |
DRLs -Derived from Surveys / Registries -Tool to Compare Doses at Different Sites -Apply to Populations of Patients, NOT Individual Exams -Are NOT a dividing line between good and bad medicine-Are Inappropriate to use for regulatory air commercial purposes./Voluntary/Will Change |
|
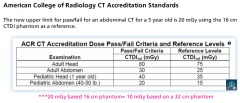
New Upper Limit for Pass/Fail for Abdominal CT for a 5 Year Old is 20mGy using the (Pedi)16cm CTDI Phantom as a Reference |
Remember! If you use Adult Phantom 32 cm for Pedi Abdomen then would get 10 mGy-
Instead of the 20 mGy for the Pedi Phantom 16cm. |
|
|
Registry? |
Registry is a systematic method for collection of observational data on patient health and demographics in a uniform manner to evaluate specified metrics for a population defined by a particular condition or procedure. |
|
|
ACR
Dose Index Registry DiR
Part of National Radiology DATA Registry NRDR |
CT DIR
uses CTDI vol and SSDE to collect dose data
NOT age.
SSDE more accurate estimate dose then estimates based on patient age. |
|
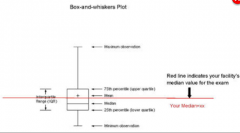
Box and Whiskers Plot |

Box and Whiskers Plot
Individual Facility's dose estimates SSDE are lower than the national medium.rP |
|
|
Practical Measures to Optimize Radiation dose for Pediatric CT |
-Consult Medical Imaging Physicist -Adopt recommendations and protocols outlined in this module -"Child Size" CT protocols based on patient body size |
|
|
"Universal Protocol" |
"Universal Protocol"
-allows any site with any machine to adapt their protocols and compare results to best practice as suggested by an appropriate DRL.
The Universal Protocol serve as a start to lower dose. |
|
|
Other Methods to Reduce Dose Pediatric Patients |
-Appropriate Centering -Optimize Projection Scans -Limit Scan Length -Eliminate Multiphase Scan (non-contrast, contrast, delayed CT scans) -Organ Shielding (Gonads, thyroid, lens of eye) -Automatic Tube Current Modulation (ATCM) -Iterative Reconstruction |
|
|
-Appropriate Centering |
-Appropriate Centering
Entrance dose to the Skin is, in part, a function of the distance of the skin from the focal spot of the CT Scanner (Inverse-Square law), positioning the patient's body in the middle of the CT gantry reduces the radiation dose to the patient. |
|
|
Reduce Dose During Projection Views |
- Switch from AP Projection to PA Projection to reduce dose to the male gonads, breast, thyroid, lens of the eye)
-Proper High voltage and/or tube current |
|
Limit Scan Length
Limit Scan Length for Scout and Clinical Images
Use Appropriate FOV |
Multiphase Exams
Rarely Needed
Doubles the Dose to the Pediatric Patient |
|
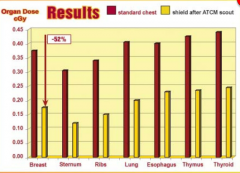
Bismuth Shield- Some Controversy-
Place Shield After ATCM Scout-otherwise may increase dose to patient |
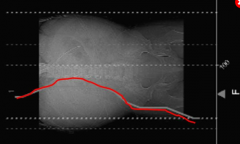
Automated Tube Current Modulation (ATCM- red line) the scanner automatically adjusts mA according to the projection scans. Reduces Dose |
|
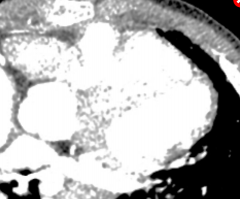
Iterative Reconstruction --Reduces Dose Compared to Filtered Back Projection Techniques |
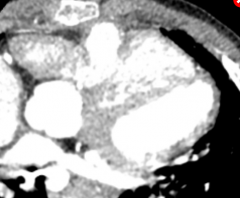
Post-Iterative Reconstruction Image- Compare to Prior |
|
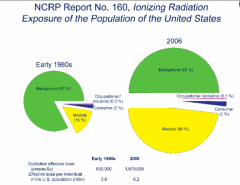
1980 Medical Radiation was 15%
2006 Medial Radiation Increased to Almost 50% of Radiation that population receives . |
Two Types of Radiation Effects:
1. High dose>> Deterministic --Tissue Effects (acute)---Dose Dependent--threshold associated
2. Lower dose >>>>> Stochastic Effects Potential for Cancer, Genetic Effects No assumed Threshold |
|
|
Potential Stochastic Effects in Children |
Stochastic Effects in Children are Potential for Cancer and Genetic Effects -Risk Depends on Dose -There is assumed no threshold -Children's cells are rapidly dividing, i.e. more vulnerable than adults for most cancers -Children live longer- more time to manifest adverse effects, i.e. cancer |
|

Children with chromosomal deletions have increased risk of developing radiation induced cancer. Which ones? |
-Ataxia Telangiectasia -Fanconi anemia -Hereditary Retinoblastoma -Down syndrome -Gardner syndrome -Nijmegan breakage syndrome -Basal Cell Nevus -Boom, Cockayne, Usher syndromes |
|
|
Risk Cancer 4 out of 10 will get cancer without radiation from CT!
One half die from the disease
No way to tell if cancer occurred from effect of radiation. |

Background Radiation Sun and Soil 3 mSv/year |
|
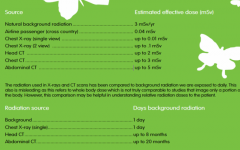
Abdominal CT = 20 months background radiation
Chest Xray = One day of Background Radiation |
Chest xray 0.01 mSv Head CT 2 mSv Chest CT 3 mSv Abdominal 5mSv |
|
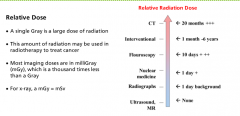
Practical a mGy=mSv
-A Gray is large dose for radiation therapy --Thousand time less is a milligray - small dose for medical radiation |
Two Views - Rising Risk -No Risk Because Threshold, More Harm from avoiding the exam |
|
|
Medical Radiation Cause Cancer? |
We don't know.
We should act cautiously as if there may be a risk. |
|
|
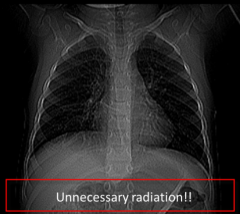
Justification of Scan
Needed in Each Case
Benefit Vs Small Risk |
Clinical Question-
Will Scan Answer the Question?
If Not, then scan is not justified. |

