![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
77 Cards in this Set
- Front
- Back
|
5 main types of blood vessels |
Arteries Arterioles Capillaries Venules Veins |
|
|
Arteries |
Carry blood away from the heart Large - elastic and leave the heart Medium - muscular Small |
|
|
Arterioles |
Smallest arteries |
|
|
Capillaries |
Thin walls Gas substances between blood and tissue |
|
|
Venules |
Smallest veins |
|
|
Veins |
Convey blood from tissues to the heart |
|
|
Angiogenesis |
Formation of blood vessels |
|
|
3 layers of blood vessel |
Tunica Interna -Epithelial inner lining Tunica Media - Middle layer consisting of smooth muscle and elastic connective tissue Tunica Externa - Connective tissue covering |
|
|
Lumen of blood vessel |
Interior opening |
|
|
Layers of tunica interna 2-3 |
Endothelium - simple squamous Basement membrane - collagen base for endothelium Internal elastic lamina (in arteries only) - thin sheet of elastic fiber resembling Swiss cheese |
|
|
Tunica media |
Muscular and connective tissue Relatively thick layer Smooth muscle cells - vasoconstriction/vasodilation- like ring around finger External elastic lamina - Substantial elastic fibers
|
|
|
Tunica externa |
Elastic and collagen fibers Numerous nerves Vaso vasorum - Tiny blood vessels in largest blood vessels Anchors blood vessel to surrounding tissue |
|
|
Precapillary sphincter |
Distal most muscle cell of the arterioles Monitors blood flow to capillary |
|
|
Resistance |
Opposition to blood flow due to friction between blood and the walls of blood vessels |
|
|
Compliance |
High - can stretch easily without tearing Arteries have high compliance |
|
|
Elastic arteries |
Largest arteries in body Aorta pulmonary trunk Branches of aorta Vessel walls are relatively thin Well defined internal and external elastic lamellae Help propel blood onward while ventricle is relaxing - pressure reservoir |
|
|
Pressure reservoir |
Elastic fibers of elastic arteries hold mechanical energy as they stretch |
|
|
Muscular arteries |
Smooth muscle Fewer elastic fibers Walls are relatively thick Vasoconstriction and vasodilation Well defined internal elastic lamellae Thin external elastic lamellae Called distributing arteries Tunica externa thicket that tunica media Tunica externa contains fibroblasts collagen and elastic fibers oriented longitudinally |
|
|
Anastomoses |
Union of the branches of two or more arteries supplying the same body region Can also occur between veins arterioles and venules |
|
|
Collateral circulation |
Alternative route of blood flow to a body part through an anastomosis |
|
|
End arteries |
Do not anastemose Obstruction equals death to organ |
|
|
Arterioles |
Small arteries Abundant Microscopic Thin tunica interna Thin internal elastic lamellae at terminal end One or two layers of cells in the tunica media Tunica externa consists of areolar connective tissue with abundant unmyelinated sympathetic nerves Key role in regulating resistance-resistance vessels |
|
|
Metateriole |
Terminal end region of arterioles Tapers toward capillary junction |
|
|
Capillaries |
Smallest blood vessels Extensive network to make contact with body’s cells Primary function is exchange of substances between blood and interstitial fluid Exchange vessels More near areas of High metabolic activity Lack tunica media and tunica externa |
|
|
Postcapillary venule |
Venule that receives blood from a capillary |
|
|
Microcirculation |
Flow of blood into postcapillary venule |
|
|
Capillary bed |
Network of 10-100 capillaries that arise from a single metateriole |
|
|
Two ways that blood can travel through a capillary network from an arteriole into a venule |

Capillaries Thoroughfare |
|
|
3 types of capillaries |
Continuous capillaries Fenestrated capillaries Sinusoids |
|
|
Intercellular clefts |
Gaps between neighboring endothelial cells |
|
|
Continuous capillaries |
Most common Endothelial cells form a continuous tube interrupted only by intercellular clefts Found in central nervous system, lungs, muscle tissue and skin |
|
|
Fenestrated capillaries |

Plasma membranes of endothelial cells have fenestrations Found in kidneys, villi of the small intestine, choroid plexus of ventricles in brain, ciliary processes of the eyes, most endocrine glands |
|
|
Sinusoids |

Wider and more winding Large fenestrations in endothelial cells Incomplete or absent basement membrane Large intercellular clefts that proteins and sometimes blood cells pass through from tissue into blood stream Ex red blood cells from red bone marrow Specialized lining cells adapted to particular tissue |
|
|
Venules Characteristics |
thin walls do not readily maintain shape drain capillary blood and return flow of blood back toward the heart |
|
|
Postcapillary Venules |
smallest venules receive blood directly from capilaries have looslely organized intercellular junctions and thus are very porous significant exchange of nutrients/wastes and white blood cell emigration highly distensable (expandable) |
|
|
Muscular Venules |
have two layers of circularly arranged smooth muscle cells exchange with interstitial fluid can no longer occur highly distensable (expandable) |
|
|
Is the tunica interna thicker in veins or arteries |
arteries |
|
|
is the tunica media thicker in veins or arteries + 1 other difference |
much thicker in arteries little smooth muscle and elastic fibers in veins |
|
|
Special features of veins |
not built to withstand high pressure lack internal or external elastic laminae lumen of a vein is larger than that of a comparable artery often appear collapsed (flattened) when sectioned blood pressure is lower in veins have valves that prevent backflow |
|
|
How does blood move through the veins |
pumping action of heart contraction of skeletal muscles |
|
|
Vascular Sinus |
Vein with a thin endothelial wall that has no smooth muscle to alter its diameter. surrounding dense connective tissure replaces the tunica media and tunica externa in providing support ex. dural venous sinuses (supported by dura mater) and coronary sinus of the heart |
|
|
Are there more veins or arteries |
There are more veins some veins are paired and accompany medium to small sized muscular arteries -- anastomotic veins Superficial Veins - course through the subcutaneous layer -- arteries do not |
|
|
Capillary Exchange |
movement of substances between blood and interstitial fluid |
|
|
3 basic mechanisms of capilary exchange |
Diffusion Transcytosis Bulk Flow |
|
|
Substances that move through diffusion is capillary exchange |
oxygen - lipid bilayer carbon dioxide - lipid bilayer glucose - intercellular clefts and fenestrations amino acids - intercellular clefts and fenestrations steroid hormones - lipid bilayer proteins and blood cells - sinusoids |
|
|
Transcytosis |
substances in blood plasma enclosed with tiny pinocytic vesicles endocytosis and exocytosis ex. insulin and certain antibodies |
|
|
Bulk Flow |
- passive process which large number of ions, molecules or particles in a fluid move together in the same direction movement from area of high pressure to low pressure for regulation of volume |
|
|
Filtration |
Pressure driven movement of fluid and solutes from blood capillaries into interstitial fluid |
|
|
Reabsorption |
pressure driven movement of fluid and solutes from interstitial fluid into blood capilaries |
|
|
Two pressures that promote filtration |
Blood Hydrostatic Pressure - heart pump Interstitial Fluid Osmotic Pressure |
|
|
Net Filtration Pressure |
balance of blood hydrostatic pressure and interstitial fluid osmotic pressure and blood colloid osmotic pressure and interstitial fluid hydrostatic pressure - determines fluid volume change NFP=(BHP+IFOP)-(BCOP+IFHP) |
|
|
Blood Hydrostatic Pressure |
pressure that water in blood plasma exerts on blood vessel walls |
|
|
Interstital Fluid Hydrostatic Pressure |
Pull on fluids from capillaries into interstital fluid from colloids suspended in IF. Typically minimal |
|
|
Pressure that promote reabsorption |
Blood Colloid Osmotic Pressure force caused by the colloidal suspension of large proteins in plasma |
|
|
3 determinants of blood pressure |
cardiac output blood volume vascular resistance |
|
|
Systolic blood pressure |
highest BP during systole |
|
|
Diastolic Blood Pressure |
lowest BP during diastole |
|
|
Mean Arterial Pressure (MAP) |
average blood pressure in arteries MAP=diastolic BP + 1/3 (systolic BP - Diastolic BP) ie a third of the way from diastolic to systolic |
|
|
Cardiac Output |
Heart Rate * Stroke Volume |
|
|
How does CO affect MAP |
CO ^ = MAP ^ |
|
|
Vascular Resistance |
Opposition to blood flow due to friction between blood and the walls of blood vessels |
|
|
3 determinants of Vascular Resistance |
1. Size of the lumen (small = resistance) 2. Blood Viscosity (Greater = resistance) 3. Total Blood Vessel Length (longer = resistance) |
|
|
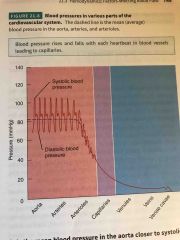
How does BP change through the system |
Back (Definition) |
|
|
Cross Sectional Area |
Increases each time an artery branches Total area that blood can flow through |
|
|
Velocity of Blood flow |
volume of blood that flows through any tissue in a given time period |
|
|
What is the relationship of velocity of blood flow to cross sectional area |
Inverse As Cross Sectional Area increases, velocity of blood flow decreases Think of capillaries, blood flow through capillaries is very slow to allow time for filtration and absorption |
|
|
Circulation Time |
time required for a drop of blood to pass from the right atrium and return at rest, typically one minute |
|
|
Things contorlled by the cardiovascular center neurons |
heart rate, contractility of ventricles, blood vessel diameter, vasoconstriction, vasodilation |
|
|
3 main types of sensory receptors that provide input to the CV center |
proprioceptors baroreceptors chemoreceptors |
|
|
autonomic nervous system regulation of blood flow/blood pressure |
sympathetic impulses reach heart via cardiac accelerator nerves, increase heart rate and contractility parasympathetic stimulation follows vagus nerves, decrease heart rate |
|
|
Vasomotor Nerves |
receive input from CV centre - Spinal Cord - Thoracic and first two lumbar spinal nerves - sympathetic trunk ganglia -sympathetic nuerons innervate blood vessels in viscera and peripheral areas - especially skin and abdominal areas |
|
|
Vasomotor tone |
moderate state of tonic contraction or vasoconstrictions sets resting level of systemic vascular resistance |
|
|
Hormones that effect blood pressure |
Renin-Angiotensin-Aldosterone system (RAA) Epinephrine and norepinephrine ADH Atrial Natriuretic Peptide (ANP) |
|
|
Local Control of Blood Flow by Tissues |
Autoregulation in capillary bed local changes regulate vasomotion vasodilators start dilation of arterioles and relaxation of precapillary sphincters increase blood flow, increase O2 level vasoconstrictors constrict arterioles and contract precapillary sphincters, decrease blood flow and decrease O2 level |
|
|
Physical changes that cause autoregulation |
Warming, Cooling Stretching - stretching decreases, smooth muscle relaxing increases |
|
|
Vasoldilating and Vasoconstricting Chemicals that effect autoregulation |
secreted by cells VASODILATING Potassium Hydrogen Lactic Acid Adenosine from ATP Nitric Oxide NO VASOCONSTRICTING thromboxane A2 superoxide radiclals Serotonin (from platelets) endothelins |
|
|
O2 level effect in pulmonary vs systemic circulations |
Systemic - low O2 causes dilation Pulmonary - low O2 causes constriction |

