![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
272 Cards in this Set
- Front
- Back
|
Name the 2 neural cell types?
|
Glial cells and neurones
|
|
|
What are astrocytes?
|
Glial cells that nourish neural tissue
They also clean up synapses and plug up leaks of blood vessels |
|
|
What do oligodendrocytes make?
|
myelin
|
|
|
What condition kills oligodendrocytes?
|
multiple sclerosis
|
|
|
What glia act as phagocytes?
|
microglia (they are the garbage and policemen)
|
|
|
which glia are anti-regeneration?
|
oligodendrocytes (Schwann)
|
|
|
What neurones are usually inhibitory (the beaurocrats)?
|
interneurones
|
|
|
T/F projections modify and interneurones make
|
False. Projections make and interneurones make
|
|
|
What is a nucleus?
|
a collection of cells that look similar and have similar functions
|
|
|
What is a commissure?
|
when an axon cross midline
|
|
|
What is an axonal grouping that does not cross midline?
|
a tract
|
|
|
What pathways have a diffuse and non-mapped CNS projection pattern?
|
visceral/arousal pathways
|
|
|
What is the CNS projection pattern of somatic pathways?
|
the projection pathways are precise and mapped (1:1 relationship between X and Y)
|
|
|
Who releases the No-Go protein?
|
oligodendrocytes
|
|
|
What is chromatolysis?
|
the dissolution of Nissl bodies in the cell body of a neuron
|
|
|
T/F.. adults have a set number of neural cells (and what evidence supports your answer?)
|
False... the hippocampus grows from exercise and learning
|
|
|
What does the vertebral atery supply?
|
hindbrain
|
|
|
What end of a neuron does Wallerian degeneration affect?
|
distal end
|
|
|
What is required for successful regrowth of a neuron?
|
Schwann cell cord penetration
|
|
|
What does the internal carotid artery supply?
|
forebrain
|
|
|
T/F... the brain's vessels are well anastomosed
|
False. the brain has lots of end arteries (the exception is the Circle of Willis)
|
|
|
What artery does rotating one's head occlude?
|
cervical vertebral artery
|
|
|
Look up to the sky (tilt head back) and you see stars. Why?
|
occlusion of vertebral arteries
|
|
|
Why don;t you die when your vertebral arteries are occluded?
|
Circle of willis shunts blood from internal carotid to vertebral artery
|
|
|
T/F... hunger alters CSF concentration
|
False.. CSF doesnt change concentrations, unlike plasma
|
|
|
Why is CSF concentration constant and what is its function?
|
to provide stability and buoyancy
|
|
|
T/F... epithelial cells of the blood brain barrier are mostly fenestrated?
|
False
|
|
|
Where in the blood brain barrier does epithelia leak?
|
choroid plexus and area postrema
|
|
|
Where in the blood brain barrier are the epithelia tight?
|
cerebral capillaries and arachnoid
|
|
|
What bodily structures does the cortex project to?
|
all of them. it controls everything!
|
|
|
what does ipsilaterally mean?
|
structures lie on the same side as one another
|
|
|
what does contralateral mean?
|
structures lie on the opposite sides of one another
|
|
|
what skills are left cerebrally dominant?
|
language, mathematics, logic
|
|
|
what do high order fibres do?
|
connect parts of the cortex on the same hemisphere to communicate with one another
|
|
|
what are the effects of a corpus callostomy?
|
decreased motor skills
split brain alien hands (ie 2 brains with the right side of the brain causing the left hand to misbehave, and the left side of the brain tries to control it with the right hand) |
|
|
what abilities are dominant on the right cerebral side?
|
spatial abilities, music, face recognition, visual imagery
|
|
|
what are the sensory receptor types?
|
tactile, proprioception, pain (and temperature)
|
|
|
What are Pacinian receptors responsive to?
|
deep press and vibrations
|
|
|
What are Ruffini receptors responsive to?
|
stretch
|
|
|
What are Merkel receptors responsive to?
|
touch and press
|
|
|
What are Free receptors responsive to?
|
pain, temp crude touch
|
|
|
What are muscle spindles responsive to?
|
muscle length - proprioception
|
|
|
What do Meissner receptors detect?
|
touch and press
|
|
|
Where are Pacinian receptors located?
|
subcutaneously and in myelin
|
|
|
Where are Ruffini receptors located?
|
all skin and myelin
|
|
|
Where are Merkel receptors located?
|
all skin, hair and myelin
|
|
|
Where are Free receptors located?
|
all skin, viscera, no/little in myelin
|
|
|
Where are muscle spindles located?
|
muscles, myelin
|
|
|
Where are Meissner receptors located?
|
glabrous (hairless) skin
|
|
|
What are the sensory receptors for proprioception?
|
muscle spindles, joint receptors, golgi tendon organs
|
|
|
What are the sensory receptors for tactility?
|
Meissner, Pacinian, Ruffini, Merkel
|
|
|
Why is grey matter grey?
|
It contains cell bodies
|
|
|
What are the functions of cells in the dorsal horn?
|
somatic sensory
|
|
|
What sensations are the cells of the dorsal horn associated with?
|
tactile, pain and proprioception
|
|
|
What cells lie n the dorsal horn?
|
tract cells, interneurones
|
|
|
What cells lie in the Intermediate Grey Matter?
|
preganglionic motor cells, interneurones
|
|
|
What is the Intermediate Grey Matter associated with?
|
visceroreceptors, smooth muscle
|
|
|
What is the function of Intermediate Grey Matter?
|
autonomic sensory motor
|
|
|
What is the function of the ventral horn?
|
somatic motor
|
|
|
What is the ventral horn associated with?
|
somatic muscle
|
|
|
What cells lie in the ventral horn?
|
alpha motor cell (motor end-plate), gamma motor cell (spindles), interneurone
|
|
|
What are funiculi?
|
large areas of white matter
|
|
|
What sensations are relayed through the sensory ascending tracts?
|
tactility, proprioception and pain (and temperature)
|
|
|
What zone/s communicates basic movements/autonomic control and skilled movements?
|
motor descending tracts
|
|
|
Does white or grey matter hold the tracts?
|
white
|
|
|
What are the major descending tracts?
|
corticospinal tract (CsT) and vestibulospinal tract (VsT)
|
|
|
What is the main pathway of pain (and temperature), and is it ascending or descending?
|
spinothalamic tract (StT), ascending
|
|
|
What are the two types of pain and temperature tracts?
|
anterior (light touch) and lateral (pain/temp)
|
|
|
What are the two type of pain/temp tract within the lateral spinothalamic tract and what are some of their features)?
|
neospinothalamic (fast, sharp; localise pain; superficial structures), paleospinothalamic (slow, dull; emotions; deep structures)
|
|
|
Describe the path of the neospinothalamic tract from receptor to cortex
|
III, VP, S1
noci/thermoceptors --> III (A-gamma) fibres --> cross ventral white commissure --> ventral posterior (VP) --> somatosensory cortex (S1) |
|
|
Describe the pathway of the paleospinothalamic tract
|
IV, BRF, MD/IL, In/Cg
noci/thermoreceptors --> IV (C) fibres --> ventral white commissure --> brain stem reticular formation (BRF) --> medial dorsal/intralaminar (MD/IL) --> insula/cingulate cortex (In/Cg) |
|
|
What is the effect of a lesion on a hemisection of spinal cord affecting the spinothalamic tract (StT)?
|
loss pain/temp on contralateral side
|
|
|
what is the main pathway of pain?
|
lateral spinothalamic tract
|
|
|
Which part of the spinothalamic tract maps pain precisely?
|
neoStT
|
|
|
What tract is involved in tactility?
|
dorsal column tract (DCT)
|
|
|
T/F the dorsal column tract runs ipsilaterally to the spinal cord hemisphere.
|
True
|
|
|
What nuclei communicate with the dorsal column tract?
|
cuneate and gracile
|
|
|
What is the function of the dorsal column tract?
|
discriminative touch, vibration, pressure
|
|
|
what is proprioception?
|
position/movement of joints/limbs
|
|
|
what are the two functional modalities of dorsal column tract?
|
tacticle touch and conscious proprioception
|
|
|
which tract is involved with unconscious proprioception, and is it ascending or descending?
|
ascending spinocerebellar tract (ScT)
|
|
|
A lesion to the spinocerebellar tract would have what effect?
|
ipsilateral proprioception loss
|
|
|
what types of touch are mapped by the dorsal column tract?
|
discriminate touch, vibration, pressure
|
|
|
What tract is all about control?
|
descending
|
|
|
What two descending tracts control posture, locomotion of proximal muscles and autonomics?
|
vestibulospinal tract (VsT) - balance
reticulospinal tract (RetST) - visceral reflexes |
|
|
What muscles does the vestibulospinal tract act on?
|
extensors
|
|
|
What does a rigid posture mean?
|
vestibulospinal lesion (as cortex is no longer able to inhibit extensors)
|
|
|
what descending tract/s controls skilled movement?
|
corticospinal tract (CsT) mainly, but also rubrospinal tract (RsT)
|
|
|
What clinially manifests from a lesion of the corticospinal and rubrospinal tracts?
|
loss of voluntary movements, clumsy hands
anti-gravity muscles are affected (classical upper motor neurone lesion) |
|
|
What are the anti-gravity muscles?
|
flexors of upper limb
extensors of lower limb |
|
|
What is/are the peak age range/s of incidence of traumatic spinal cord injury?
|
ages 15-24 and 65-74
|
|
|
do males or females have a higher incidence of non-traumatic SCI?
|
females
|
|
|
what is the prevalence of Non Traumatic Spinal Cord Injury and Traumatic Spinal Cord Injury in Australia?
|
NTSCI - 5.1-80 per million people per year
TSCI - 15-17 per million people per year |
|
|
what is a Jefferson fracture?
|
Compression fracture at C1
|
|
|
What spinal cord injury involves subluxation of vertebral body?
|
flexion rotation injury
|
|
|
what are the most likely spinal levels to be damaged by traumatic causes?
|
C4/C5
|
|
|
What is the standard neurological classification system of spinal cord injury?
|
American Spinal Injury Assocation (ASIA)
|
|
|
what is the sensory pattern of loss in a spinal cord lesion?
|
loss of pain and temp contralaterally
loss of tactile ipsilaterally |
|
|
spinal cord injury above which level will result in substantial loss of sympathetic vascular tone with resultant hypotension?
|
T6
|
|
|
which SCI may be associated with respiratory insufficiency from paralysis of intercostal and abdominal muscles?
|
low cervical and high thoracic injuries
|
|
|
what are the consequences of loss of intercostal muscle function?
|
diphragmatic breathing
impairment of coughing and effective clearance of secretions (commonly leads to atelectasis) V/Q mismatch |
|
|
what is the Brown-Sequard syndrome?
|
hemi-section of spinal cord resulting in motor paralysis and loss of deep touch, vibration and proprioception on the same side as the damage and loss of pain, temp and light touch on the opposite side
|
|
|
which reflexes are often the first to return after spinal shock in an upper motor neurone lesion?
|
anal and bulbo-cavernosus reflexes
|
|
|
how long is the spinal cord?
|
45 cm
|
|
|
what anchors the spinal cord to the sacrum and coccyx below?
|
filum terminale (fibrous band of pia mater)
|
|
|
where are somatic motoneurons located in the spinal cord?
|
Rexed lamina IX
|
|
|
where is the main primary afferent spinal entry zone?
|
medial edge of dorsal horn
|
|
|
which reflex pathway includes one synapse only?
|
stretch reflex pathway
|
|
|
what maintains urinary continence?
|
contraction of trigone, internal and external sphincters
|
|
|
what contracts to expel bladder contents during micturition?
|
detrusor muscle
|
|
|
how does parasympathetic innervation affect the detrusor?
|
causes contraction
|
|
|
what causes relaxation of the detrusor muscle?
|
activation of symp nerves
|
|
|
what innervates the external urethral sphincter?
|
somatomotor nerve fibres within the pudendal nerve (originate in sacral spinal cord)
|
|
|
what are the three levels of CNS control of bladder function?
|
lumbar/sacral spinal cord
micturition centre in pons suprapontine centres |
|
|
which muscles contribute to conscious effort to maintain continence?
|
striated muscles of perineum and pelvic floor
|
|
|
which two events are involved in the micturition reflex?
|
relaxation of external urethral sphincter via inhibition of somatic efferents
contraction of detrusor via parasymp activation |
|
|
what has been found to be associated with poor adjustment to spinal injury?
|
despondency
grieving chronic pain |
|
|
what is associated with good outcome after SCI?
|
young age
female sex higher education level ability to relate well confidence in one's mastery over environment |
|
|
destruction of which elements of neurones leads to death of the neurone?
|
soma
axon |
|
|
what are the two types of neurones?
|
projections (make the message)
interneurones (modify the message) |
|
|
what are the three types of glial cells?
|
astrocytes
oligodendrocytes microglia/macrophages |
|
|
what is the function of astrocytes?
|
nourishment of neurones
synapse cleaner relationship with blood vessels - plug leaks |
|
|
what do oligodendrocytes do?
|
make myelin
anti-regeneration |
|
|
what is the role of microglia?
|
phagocytosis
anti-inflamm/immune response "brain policeman" |
|
|
what is the commonest source of autonomic dysreflexia?
|
bladder
|
|
|
what are the tactile receptors?
|
Meissner (touch, pressure)
Pacinian (deep pressure, vibration) Ruffini (stretch) Merkel (touch, pressure) |
|
|
which receptors sense proprioception?
|
muscle spindles
joint receptors Golgi tendon organs |
|
|
which receptors sense pain and temperature?
|
nociceptors (free receptors)
|
|
|
what fibres are associated with tactile receptors?
|
Abeta (type II) fibres
|
|
|
which fibres are associated with proprioceptors?
|
Ia, Ib, Abeta (II)
|
|
|
which fibres are associated with pain and temperature?
|
Adelta (III), C (IV)
|
|
|
what cells are in the dorsal horn?
|
somatic sensory
|
|
|
where do autonomic cells lie in the spinal cord?
|
intermediate grey matter
|
|
|
which cells are in the ventral horn?
|
somatic motor cells
|
|
|
which tract is associated with pain and temperature?
|
spinothalamic
|
|
|
which fibres are associated with the neospinothalamic tract?
|
III
|
|
|
which fibres are associated with the paleospinothalamic tract?
|
IV
|
|
|
where are the cell bodies of the spinothalamic tract located?
|
dorsal horn
|
|
|
what is the course of the neospinothalamic tract?
|
dorsal horn->ventral posterior nucleus of thalamus->S1
|
|
|
what is the course of the paleospinothalamic tract?
|
dorsal horn->BRF->MD?IL of thalamus->insula/cing cx
|
|
|
what is the result of hemisection of spinothalamic tract?
|
loss of pain/temp contralateral side
|
|
|
where does the spinothalamic tract cross the midline?
|
ventral white commissure
|
|
|
where are the cell bodies of the dorsal column tract?
|
DRG
|
|
|
In a complete lesion, no voluntary motor or sensory function is preserved more than how many segments below the level of the injury?
|
3 segments below
|
|
|
Where do the cell bodies of automatic neurones lie?
|
Outside the CNS
|
|
|
What is the main chemical neurotransmitter of the efferent nervous system?
|
Acetylcholine (except in vascular smooth muscle, which is noradrenaline)
|
|
|
T/F.. Preganglionic neurone subgroups can be controlled by both spinal afferents and descending inputs from brain nuclei
|
T
|
|
|
What are the main spinal excitatory and inhibitory neurotransmitters?
|
glutamate - excitatory
GABA - inhibitory |
|
|
Which inputs does the sympathetic preganglionic neuron (SPN) receive?
|
excitatory and inhibitory
|
|
|
Where do the cell bodies of the preganglionic neurons lie?
|
mainly in the lateral horn
(intermediolateral cell column) of the thoracolumbar grey matter. |
|
|
T/F.. Spinal afferents mainly communicate with sympathetic preganglionic neurones synaptically.
|
False. Spinal afferents only communicate with SPN via interneurones
|
|
|
What is the effect of increased parasympathetic activity on the bladder?
|
contraction of the bladder wall (detrusor muscle)
relaxation of the internal sphincter |
|
|
What is the effect of increased sympathetic activity on the bladder?
|
relaxation of the bladder wall (detrusor muscle)
contraction of the internal sphincter |
|
|
To begin micturition, where are the visceral afferents sent to?
|
sacral spinal cord
|
|
|
Does pudendal nerve activity increase or decrease to relax the external sphincter in micturition?
|
decrease
|
|
|
What stops a non-overfull bladder from leaking?
|
reflex sympathetic activation (keeps detrusor muscle relaxed and external sphincter contracted)
|
|
|
What spinal roots are being tested in reflexes for biceps, brachioradialis, triceps, patellar and achilles respectively?
|
biceps - C5 (C6)
brachioradialis - C6 triceps - C7 patellar - L4 achilles - S1 |
|
|
What is the basic premise of the stretch reflex?
|
neuromuscular spindles are sensitive to stretch and then fire, triggering a deep reflex contraction (deep tendon)
|
|
|
What reflexes return first following spinal shock?
|
urogenital then peripheral
|
|
|
Which reflexes does spinal shock diminish?
|
somatic and visceral reflexes below the insult
|
|
|
How long does spinal shock take to dissipate?
|
~2 weeks
|
|
|
What are some signs and symptoms of autonomic dysreflexia?
|
headache, sweat, goose-bumps, hypertension (episodic)
|
|
|
How long after spinal shock does autonomic dysreflexia occur?
|
weeks-years after
|
|
|
List some signs of lower motor neurone lesions
|
paralysis (weakness), bladder (no work), fasciculation, fibrillations, areflexia, flaccidity, atrophy
|
|
|
List some somatic signs of upper motor neurone lesions
|
bladder (no control), paralysis, no skilled movements, hyperreflexia (clonus, babinsky), spasticity (spring-like, clasp-knife, stance/gait)
|
|
|
What are some features of the pyramidal stance?
|
Flexed upper limb, extended knee, circumducted hip, flexed foot plantar, paresis of face (loss of some voluntary movement), head tilted
|
|
|
What motor cells are involved in the gamma reflex loop?
|
gamma motor cells (effectors)
|
|
|
What are two examples of the stretch reflex?
|
muscle tone and reflex contraction (deep tendon)
|
|
|
When does the golgi reflex occur and why?
|
during over-stretching, to stop the stretch
|
|
|
T/F... no reflex can occur below the lesion in spinal shock
|
True
|
|
|
What lesion could decrease heart rate?
|
A spinal cord transection above T5-6
|
|
|
What spinal lesion level allows for autonomic dysreflexia?
|
T5-6 or above (above heart)
|
|
|
What cranial nerve allows baroreceptors at the carotid sinus to communicate with the brain stem?
|
hypoglossal
|
|
|
What is autonomic dysreflexia?
|
parasympathetic response above lesion and sympathetic response below it
|
|
|
What is nociceptive pain?
|
pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors
|
|
|
What are three features of nociceptive pain?
|
1. rapid onset
2. arising from potentially identifiable pathology 3. often responsive to weak and opioid analgesics |
|
|
What is the push button concept of pain?
|
noxious stimulus --> pain receptor --> pain pathway --> pain perception
|
|
|
Name the 5 ascending tracts involved in pain?
|
spinothalamic
spinomesencephalic spinoreticular spinocervicothalamic postsynaptic dorsal column pathway |
|
|
What is the difference between C and A delta nociceptor fibres?
|
C fibres are unmyelinated, which A delta fibres are myelinated
C fibres respond polymodally (to thermal, mechanical and chemical stimuli). A delta fibres are high threshold mechanoreceptors and mechanothermoreceptors. |
|
|
What are some problems with the cartesian (push button) model of pain?
|
the effect of surrounding circumstances on pain (ie war v sport)
effect of neurosurgery (rhizotomy doesn't always stop pain) referred pain placebo effects amputation pain |
|
|
What is the spinal gate concept of pain?
|
the system can be modified in feedforward or feedback systems (large fibres keep gate closed, small fibres open gate)
modified stimulus response relationship process modifies noxious input |
|
|
What is neuropathic pain?
|
Pain caused by a lesion or disease of the somatosensory nervous system
|
|
|
List some features of neuropathic pain?
|
constant and intermittent components
descriptors - burning, sharp, shooting, electric associated with areas of sensory defecit indicating nervous system pathology often hyperaethesia (abnormal increased sensitivity) often associated with paraesthesia (pins and needles) or dysaesthesia (sensation) often delay in onset |
|
|
Which fibres are involved in nociceptive and neuropathic pain?
|
C fibres for nociceptive, A fibres for neuropathic
|
|
|
Name three functions of astrocytes
|
Nourish neurons, Clean synapses, Plug blood vessel leaks
|
|
|
Which cells make central and peripheral myelin?
|
Oligodendricytes - central, Schwann cells - peripheral
|
|
|
What proportion of cardiac output does the brain usually require?
|
~20%
|
|
|
The proencephalon gives rise to which structures?
|
Cerebral cortex, thalamus, subthalamus
|
|
|
What is the name of the fissure that separates the parietal from temporal lobe?
|
Sylvian fissure
|
|
|
Which reflex is responsible for maintaining muscle tone? Where does it synapse?
|
Stretch reflex, Anterior horn of spinal cord
|
|
|
What is the function of the gamma-reflex loop?
|
To modify the stretch reflex
|
|
|
What are the afferent and efferent fibres of the stretch reflex?
|
Afferent = Ia, Efferent = alpha motor neuron
|
|
|
Which reflex allows withdrawal from painful stimuli? Where does it synapse?
|
Flexor reflex, Synapses with an excitatory interneuron in grey matter of spinal cord
|
|
|
Which reflex stops muscle contraction in response to an overwhelming load? What type of efferent fibre does it use?
|
Golgi tendon reflex, Ib fibre
|
|
|
What level of spinal injury may cause a stereotypical reduction in heart rate and blood pressure?
|
Anything above T5-6
|
|
|
What level of spinal injury may cause problems with micturition?
|
Anything above S2-4
|
|
|
What signs and symptoms are associated with autonomic dysreflexia?
|
Paroxysmal hypertension, bradycardia, throbbing headaches, profuse sweating, flushing of skin above lesion
|
|
|
What is the mechanism behind changes in blood pressure and heart rate in autonomic dysreflexia?
|
Abnormal pain/input below spinal level of injury, Increased local SNA (but fails to ascend), Local vasoconstriction and increased BP, Baroreceptor mediated increase in PSNA that fails to descend below lesion, Reduced heart rate and failure to switch of raised blood pressure
|
|
|
Name six features that can be associated with a lower motor neuron lesion
|
Atrophy, Paralysis, Flaccidity, Areflexia, Bladder doesn't work, Fasciculations and fibrillations
|
|
|
Name six features of an upper motor neuron lesion
|
Paralysis, Hyperreflexia, Spasticity (clasp-knife, No atrophy, No control of bladder(reflexes only,Pyramidal stance with flexion of elbow and extended knee
|
|
|
What type of fibres do meissner, merkel, pacinian and ruffini receptors use?
|
A-beta (type II)
|
|
|
What type of fibres do pain receptors use?
|
A-delta (type III) and C (type IV)
|
|
|
What types of fibres do muscle spindles use?
|
Types Ia, Ib and II
|
|
|
Where would you find the receptors for and what is the function of:
a) Meissner receptors b) Merkel c) Pacinian d) Ruffini |
a) Hairless (glaborous skin) - touch and pressure
b) All skin, hair, myelin - touch and pressure c) Subcutaneous and myelin - deep vibration d) All skin and myelin - stretch |
|
|
Describe the path (with synapse, cross and cell bodies) of the spinothalamic tract.
|
Nociceptors via DRG to synapse in DH of SC > Crosses via anterior white commisure > Ascends as StT (dorsolateral GM)> thenNeoStT > VP thalamus > S1 PaleoStT > BRF > DM thalamus > cingulate cortex and insula, Cell bodies in DRG
|
|
|
Describe the path (with cell bodies, synapse and cross) of the dorsal column pathway
|
Enter via DH of SC > Ascend as cuneate and gracile tracts > Synapse at nucleus gracilis or cuneatus > Cross at sensory decussation of pyramids (above motor) via internal arcuate fibres > Ascend as medial lemniscus > VP thalamus > S1, Cell bodies in DRG
|
|
|
Describe the path (with cell bodies, synapse and cross) of the corticospinal tract
|
M1, parietal cortex and frontal-cingulate>Corona radiata>Internal capsule>Pyramids, cross at pyramidal decussation>Descend as CsT>Synapse in AH of SC, Cell bodies in parietal, motor and frontal-cingulate cortex
|
|
|
Describe the path (with cell bodies, synapse and cross) of the spinocerebellar tract
|
Proprioceptor via DRG>synapse in intermediate GM>ascend in ventrolateral WM>Cerebellum, Doesn't cross, Cell bodies in DRG
|
|
|
Describe the path (with cell bodies, synapse and cross) of the rubrospinal tract
|
Red nucleus (cell body)>Cross in ventral tegmental midbrain>synapse in AH of GM>Somatic muscle
|
|
|
Describe the path (with cell bodies, synapse and cross) of the reticulospinal and vestibulospinal tracts
|
RetsT=BRF (cell body)>Synapse in GM of SC>Exit to SmM or SkM; VsT=Vestibular nucleus (cell body)>Descends to synapse in AH of GM>SkM, Neither cross
|
|
|
What is the function of the dorsal column tract?
|
Touch, vibration, pressure + Conscious (thalamic) proprioception
|
|
|
What is the function of the spinocerebellar tract?
|
Unconscious (cerebellar) proprioception
|
|
|
What is the function of the vestibulospinal tract?
|
Control of posture and autonomics
|
|
|
What is the function of the rubrospinal tract?
|
Assists the CsT with distal skilled movement
|
|
|
What is the function of the reticulospinal tract?
|
Control of posture and autonomics
|
|
|
How will a lesion of the corticospinal tract present?
|
Classical UMN presentation, contraction of anti-gravity muscles (flexors in upper limb, extensors in lower limb), loss of ipsilateral skilled (distal movement)
|
|
|
What type of receptor to preganglionic autonomic neurons act upon?
|
Nicotinic ACh receptor
|
|
|
What are the sympathetic postganglionic receptors for:
a) viscera b) vascular SmM c) adrenal medulla d) sweat glands |
a) NAd
b) NAd c) Nicotinic ACh d) Muscarinic ACh |
|
|
What type of receptors are parasympathetic postganglionc receptors?
|
Muscarinic ACh
|
|
|
Describe the course of sympathetic efferent fibres (beginning with preganglionic fibres)
|
Sympathetic preganglionic cell bodies are in interomediolateral grey matter of SC> ventral horn > exit via ventral root> spinal nerve> white ramus> symp ganglion (ascend, descend or synapse immediately)> postganglionic exit ganglion via grey ramus
|
|
|
Describe the course of parasympathetic fibres
|
Preganglionic nuclei (cranial nerve or S2-S4) (assume S2-S4 for rest)> ventral horn > exit via ventral root> terminal ganglion near effector organ
|
|
|
T/F Sympathetic preganglions are unmyelinated and sympathetic postganglions are myelinated
|
False, The reverse is true
|
|
|
What role does Parasympathetic Nervous System play in micturition?
|
Responsible for contraction of the detrusor muscle and relaxation of the internal sphincter
|
|
|
What effect does Sympathetic Nervous System have on the bladder?
|
Relaxation of the detrusor muscle and contraction of the internal sphincter
|
|
|
Which nerve controls the external sphincter of the bladder?
|
Pudendal
|
|
|
What are the three most common causes of neuropathic pain?
|
Amputation, SC trauma , Diabetes
|
|
|
Name three possible mechanisms of neuropathic pain
|
1) Ectopic activity of nociceptors following trauma due to increased Na channel expression
2) Glutamate release causing Ca influx and increased response to central transmission of pain 3) loss of descending inhibitory pain pathways 4) sprouting or rewiring of damaged nerves |
|
|
What is the definition of neuropathic pain?
|
Pain initiated or caused by a primary lesion or dysfunction in the nervous system
|
|
|
What is the cause of a subdural haematoma?
|
Short-duration angular acceleration causing rupture of dural bridging vessels
|
|
|
What type of force generally causes diffuse axonal injury?
|
Acceleration of a longer duration (than for subdural haematoma) e.g. car crash
|
|
|
What is the cause of progressive damage with brain trauma?
|
Trauma>glutamate release>calcium influx>damage
|
|
|
What is the time course for diffuse axonal injury?
|
Starts ~2 hrs post injury, may continue for a month
|
|
|
T/F Subdural haematoma has a higher mortality rate than diffuse axonal injury
|
True
|
|
|
Long-term exposure to boxing-like trauma may cause which pathological inclusions in the brain?
|
Neurofibrillary tangles and diffuse beta-amyloid plaques
|
|
|
What are the two major causes of spinal cord injury?
|
Motor Vehicle Accident (50%) and sports (20%)
|
|
|
What is syringomyelia? When does it occur?
|
A cavity of CSF that dissects out of the central canal of the spinal cord into the white matter. Generally post-traumatic
|
|
|
What are the common causes of anterior cord syndrome? What are the symptoms?
|
Causes: Ruptured disc or burst-fracture of vertebrae
Symptoms: pain & temp (StT) below lesion, LMN (AH) at lesion level + larger lesion causes UMN (CsT) below lesion |
|
|
What are the common causes and symptoms of Brown-Sequard Syndrome?
|
Causes: Penetrating injury, MS, tumour
Symptoms: Ipsilateral motor UMN weakness (CsT) Ipsilateral touch, vib and prop loss (DcT) Contralateral pain and temp loss (StT)+ Sometimes band of pain and temp loss ipsilat (StT before they cross) |
|
|
What must the first aid management of a spinal cord injury broadly involve?
|
Immobilisation of the unstable spine
Paying attention to airway and breathing Looking for injuries which may not be evident due to loss of pain sensation below the SCI (Source: Essential Readings 6.01:1) |
|
|
What area/s of the spine is damaged in Tetraplegia?
|
Cervical spine
(Source: Essential Readings 6.01:1) |
|
|
What area/s of the spine are damaged in Paraplegia?
|
Thoracic or Lumbar cord or nerve roots within the spinal canal.
(Source: Essential Readings 6.01:1) |
|
|
How do you define the concept of level of spinal injury?
|
The lowermost neurologically intact segment of the spinal cord with normal motor and sensory function.
(Source: Essential Readings 6.01:1) |
|
|
In a complete lesion, how many segments below the level of spinal cord injury can voluntary motor or sensory function be preserved?
|
up to 3 segments.
(Source: Essential Readings 6.01:1) |
|
|
What feature is present in complete sacral spinal cord lesions?
|
Impairment of autonomic function
Loss of bladder and bowel control (Source: Essential Readings 6.01:1) |
|
|
What is Spinal Shock?
|
A state of loss of sensory and motor function and somatic and autonomic reflexes below an acute, abrupt spinal cord injury, that may last days to 4 weeks.
(Source: Essential Readings 6.01:1,4) |
|
|
What level of spinal cord injury can cause loss of sympathetic vascular tone with hypotension?
|
Above T6
(Source: Essential Readings 6.01:1) |
|
|
What spinal cord injuries can cause respiratory insufficiency but not respiratory failure?
|
low cervical (C6,7) or high thoracic due to paralysis of intercostal and abdominal muscles needed in forced expiration/cough.
(Source: Essential Readings 6.01:1) |
|
|
What spinal cord injuries can cause respiratory failure, not just respiratory distress?
|
High cervical cord injury (C5 and above) due to phrenic nerve involvement, causing diaphragmatic paralysis requiring mechanical ventilation.
(Source: Essential Readings 6.01:1) |
|
|
What are some medium term issues of health care in a patient with a spinal cord injury, and how do you treat or prevent their occurrence?
|
Paralytic ileus - naso-gastric aspiration
stress ulceration - proton pump inhibitors paralysed bladder w overdistension - catheterisation thromboembolis - phamacological (heparin?) and mechanical measures Pressure sores - regular pressure relief spasticity and contracture development - re positioning limbs to prevent muscle shortening (Source: Essential Readings 6.01:1) |
|
|
What is the filum terminale of the spinal cord?
|
A fibrous band of pia mater that anchors the spinal cord to the sacrum and coccyx below. From LV1 - SV2 it is loosely surrounded by dura and arachonoid mater, below SV2 the dura mater tightly adheres to its surface.
(Source: Essential Readings 6.01:2) |
|
|
Where does the spinal cord extend from?
|
C1 - L1 vertebra.
(Source: Essential Readings 6.01:2) |
|
|
Where in the spinal cord is a good place to sample CSF with minimal risk of spinal cord damage?
|
LV4/LV5, as the area between the spinal cord end (LV1) and the descent of dura and arachnoid mater to S2 contains a large amount of CSF investing the cauda equina.
(Source: Essential Readings 6.01:2) |
|
|
What spinal level will you find preganglionic sympathetic neruons?
|
C8-L1, intermediate grey area
(Source: Essential Readings 6.01:2) |
|
|
What spinal level will you find preganglionic parasympathetic neurons?
|
S2-S4, intermediate grey area
(Source: Essential Readings 6.01:2) |
|
|
Describe the position of the Rexed laminae on a spinal cord cross section:
a) I-V b) VIII,IX c) VI,VII, X |
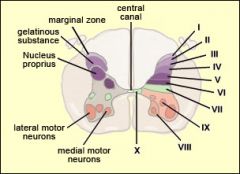
a) dorsal horn
b) ventral horn c) intermediate grey (Source: Essential Readings 6.01:2) |
|
|
What Rexed lamina of the spinal cord are somatic motoneurons locted in?
|
IX
(Source: Essential Readings 6.01:3) |
|
|
What is the medial motor column of the spinal cord?
|
Contains motoneurons innervating the axial muscles of the body, and is present throughout the length of the spinal cord.
(Source: Essential Readings 6.01:3) |
|
|
What is the lateral motor column of the spinal cord?
|
Contains motoneurons innervating muscles of the upper and lower limbs, and is found only in regions of the cervical and lumbar enlargements.
(Source: Essential Readings 6.01:3) |
|
|
What does damage to the ventral horn, somatic motor neurons result in?
|
Lower motor neuron lesion signs =Paralysis, wasting of denervated muscles, absence of muscle tone (flaccidity) and absence of reflexes (areflexia).
(Source: Essential Readings 6.01:3) |
|
|
What does damage to descending motor pathways within the lateral or ventral column of white matter result in?
|
Upper motor neuron lesion signs = Paralysis or paresis, spasticity (hypertonia), exaggerated reflexes (hyper-reflexia).
(Source: Essential Readings 6.01:3) |
|
|
When entering the spine at the dorsal root, do the large myelinated afferents or the small unmyelinated afferents lie more medially?
|
Large myelinated primary afferents enter more medially.
(Source: Essential Readings 6.01:3) |
|
|
What Rexed laminae do second order neurons of the spinal thalamic tract lie in?
|
I or V
(Source: Essential Readings 6.01:3) |
|
|
What is hypovolaemic shock?
|
Circulatory shock as a result of blood loss that causes blood pressure to fall, which is compensated for by an increase in heart rate and increase in peripheral vascular resistance. The skin is cold and clammy.
(Source: Essential Readings 6.01:4) |
|
|
What occurs in the period of time following spinal shock?
|
Reflexes below the level of spinal cord injry become hyperresponsive, leading to an increase in tone and hyperreflexia in limbs and bladder if they are below the lesion.
(Source: Essential Readings 6.01:4) |
|
|
What conditions can spinal shock mask?
|
It may mask hypovolaemic shock associated with injuries (which increases heart rate) and makes it difficult to assess underlying pathology and prognosis due to loss of sensation. Above T6 loss of SNS tone leads to vasodilation and hypotension and can also lead to bradycardia.
(Source: Essential Readings 6.01:14) |
|
|
What is autonomic dysreflexia?
|
Can occur in a a spinal cord injury above T6. Nociceptive input below the spinal injury (e.g. distended bladder) produces a SNS mediated vasoconstriction which dangerously rises the blood pressure. Loss of descending inhibition to SNS means that the only compensatory mechanism which the body can only attempt is to reduce the heart rate via Parasympathetic fibres.
(Source: Essential Readings 6.01:4) |
|
|
What is the trigone in the bladder?
|
An area of smooth muscle at the base of the bladder, below which the bladder opens into the urethra. Contraction of the trigone (and spincters) maintains continence.
(Source: Essential Readings 6.01:5) |
|
|
What innervates the external urethral sphincter of the bladder?
|
Somatomotor nerve fibres within the pudendal nerve, originating in the sacral spinal cord S2-S4.
(Source: Essential Readings 6.01:5) |
|
|
What nerves cause detrusor muscle contraction in the bladder?
|
Parasympathetic cholinergic innervation originating from the sacral spinal cord S2-S4, the pelvic splanchnic nerves.
(Source: Essential Readings 6.01:5) |
|
|
What nerves cause detrusor muscle relaxation in the bladder?
|
Sparse sympathetic adrenergic innervation, from the hypogastric plexus, originating in (mostly) the lumbar spinal cord, T10-L2.
(Source: Essential Readings 6.01:5) |
|
|
Describe the urinary continence reflex.
|
Bladder filling activates stretch receptors in the detrusor, which project to the sacral cord and cause inhibition of PSNS supplying the detrusor (S2-S4, allowing relaxation), and excite the somatic pudendal nerve (S2-S4) to the external urethral sphincter (allowing contraction) .
(Source: Essential Readings 6.01:5) |
|
|
Describe the micturition reflex.
|
High voluntary control. Pontine/Sacral micturition centres cause relaxation of external urethral sphincter via inhibition of the pudendal, and contraction of the detrusor via PSNS activation. The internal sphincter is mechanically pulled open, and urination is accelerated by bladder and urinary afferents to the pontine micturition centre, causing further detrusor contraction.
(Source: Essential Readings 6.01:5) |

