![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
230 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
True or False
Oropharyngeal and esophageal dysphagia often co-occur. |
Yup
|
|
|
|
The top ___ percent of the esophagus is ____ muscle, while the bottom ____ percent is ____ muscle.
|
33%
striated 66% smooth |
|
|
|
The inner layer of muscle in the espophagus is ____ serving to _____ the esophagus
|
circular
squeeze/constrict |
|
|
|
The outer layer ofmuscle in the esophagus is ____ serving to _____ the esophagus
|
longitudinal
shorten |
|
|
|
The UES opens and closes ____, whereas the LES opens and closes ____. Why?
|
quickly
slowly The LES has to remain open until the esophagus is clear |
|
|
|
How long for food to travel (typically) from the mouth to the cervical esophagus? At what rate does it travel from the cervical esophagus to the stomach?
|
1 sec
3-4 cm/sec (slow) |
|
|
|
Ennervation of the upper esophagus by the CNX...
|
goes directly to the muscle fiber (excitatory-Ach)
|
|
|
|
Ennervation of the lower esophagus by the CNX...
|
is via the ENS (enteric), CNX to ENS (excitatory, Ach); then ENS to muscle fiber (both excitatory Ach and inhibiting N0, VIP)
|
|
|
|
Things like to flow...
|
...from high to low.
Pressure, that is. |
|
|
|
Intra-abdominal resting pressure?
|
+5mm Hg
|
|
|
|
Intra-thoracic resting pressure?
|
-5mm Hg
|
|
|
|
LES resting pressure?
|
+25mm Hg
|
|
|
|
The esophagus enters the stomach through the diaphragm at the ____
|
esophageal hiatus
|
|
|
|
True or False
The enteric nervous sytem is embedded in the wall of the GI and is part of the ANS. |
False
It is separate from both the CNS and ANS, lining the intestinal tract and has over 100M neurons. |
|
|
|
Name me some general categories of causes of oropharyngeal dysphagia, say 6:
MINIMS |
Muscular
Iatrogenic Metabolic Infectious Neurologic Structural |
|
|
|
Name me some general categories of esophageal dysphagia
SIMINIC |
Structural
Iatrogenic Motility Infectious Neoplastic Inflammatory Congenital |
|
|
|
Patient N has an esophageal dysphagia problem that is structural. What are five possibilities?
SHEEP |
Schatzki's Ring
Hiatal Hernia Esophageal Diverticula Eosinophilic esophagitis Peptic stricture |
|
|
|
Patient Q comes in saying things are sticking in her throat right here (pointing to the notch at the base of her throat). Is this more likely to be esphageal or pharyngeal dysphagia?
|
Your guess is as good as mine
|
|
|
|
Patient O is complaining of things getting stuck right there (pointing to his chest). Where's the problem likely to be located if it's esophageal dysphagia?
|
At or below where he's pointing.
|
|
|
|
How often is food impaction seen at NUH?
|
3-4 times a week
|
|
|
|
My stomach is protruding above the diaphragm. I have a/an
|
hiatal hernia
|
|
|
|
Your stomach has got a web of tissue localized to the esophageal squamocolumnar junction that's coexisting (almost invariably) with a hiatal hernia. You don't have an LES. What do you have?
|
Schatzki's ring
|
|
|
|
Is schatzki's ring common? If so, how so (percent) and are there any populations it is more common in? If it's acquired, how is it acquired?
|
Yup. 4-15% of radiographic studies show it.
More prevalent with age resulting from chemical injury of eg |
|
|
|
Clinical presentation of schatzki's ring?
|
intermittent dysphagia for solids
|
|
|
|
What's steakhouse syndrome and what disorder is it related to?
|
Schatzki's ring and it's a food impaction.
|
|
|
|
Esophageal dysphagia is most common with esophageal rings of what size?
|
<13 mm
|
|
|
|
Dude! Your esophagus looks like a trachea! What's wrong with you?
|
Eosiniphilic Esophagitis (allergy induced)
|
|
|
|
What foods cause the most impactions?
|
Bread. And meat.
|
|
|
|
What's the likelihood of an impaction with an esophageal diameter (at the point of constriction) of less than 13mm
|
about 100%
|
|
|
|
What's the likelihood of an impaction with an esophageal diameter (at the point of constriction) of about 13-20mm?
|
about 33%
|
|
|
|
What's an esophageal complication of GERD (a type of stenosis)?
|
Peptic stricture
|
|
|
|
What is a peptic stricture?
|
scar tissue forming at the esophageal juncture (collagen and fibrous tissue) as a result of GERD
|
|
|
|
____ of people seeking medical attention for symptoms of GERD have esophagitis.
|
1/3
|
|
|
|
Most common causes of ED?
|
Eosiniphilic Eg
Schatzki's ring |
|
|
|
Does reflux esophagitis have any complications and if so, what are they?
ABBUSE |
Adenocarcinoma
Barrett's Esophagus Bleeding Ulceration Stricture Erosive esophagitis |
|
|
|
____ percent of people with esophagitis have a peptic stricture
|
8-20%
|
|
|
|
How to treat a peptic stricture...
|
dilation
lifelong acid suppression |
|
|
|
True or False
Agh! Hiatal hernia! Well, at least it's not very common so I don't have to worry too much about it. |
False
It's super common, with 60% of elderly enjoying it, especially int he West. Axial type can predispose one to GERD |
|
|
|
Patient Q presents with dysphagia, regurgitation, aspiration, halitosis and hoarseness, as well as a focal neck swelling that gurgles on palpation (Boyce's sign). What does Patient Q have?
|
A Zenker's diverticulum
|
|
|
|
Patient Ohm has a mucosal outpouching of the hyopharyngeal wall proximal to the cricopharyngeus muscle. What does patient ohm have? Will a myotomy help?
|
Zenker's diverticulum?
They seem to. |
|
|
|
There's this semilunar fibrotic narrowing of the esophagus right below the UES. What is it, and are they common?
|
Esophageal web
6-12% of radiographic studies |
|
|
|
Due to poor compliance of the cricopharyngeus there's this constriction that is causing elevation in intrabolus pressure and regurgitation. What is it?
|
Cricopharyngeal bar. It's thick, whereas a web is thin.
|
|
|
|
What are some esophageal motility disorders?
PADS |
Polymyositis
Achalasia Diffuse Esophageal Spasm Scleroderma |
|
|
|
What's motility anyway? What does esophageal motility disorder mean?
|
Function, to do with muscle and nerve. Abnormal peristalsis!
|
|
|
|
If it takes my esophagus 5 minutes to move food down through the GE junction, what's a probable cause?
|
Achalasia (failure to relax)
|
|
|
|
Normal esophageal transit time is..
|
about 8 seconds
|
|
|
|
Oh gosh, ENS neuropathy, resulting in loss of ganglion cells within the esophagus and LES and degeneration of vagal fibers. What's gonna happen?
|
Achalasia
|
|
|
|
Some therapies for achalasia?
|
botox (not so great)
pneumatic dilation (3-4 cm) Laproscopy |
|
|
|
Simultaneous contractions along the the esophagus causes a characteristic pattern called a _____ esophagus, aka ____. Does it affect the smooth or striated portion of the eg?
|
corkscrew esophagus
diffuse esophageal spasm. smooth |
|
|
|
Pain with swallowing is called:
It's associated with? |
odynophagia
ulcerations |
|
|
|
What are some iatrogenic esophagial dysphagias?
CRaPS FuNC |
Caustic (pill)
Radiation Post surgical Sclerotherapy Fundoplication Nasogastric tube Chemotherapy |
|
|
|
How to avoid pill esophagitis?
|
at least 1/2 glass water minimum when taking a pill and please don't lie down immediately.
|
|
|
|
Most common site of injury with pill esophagitis is at the level of __. Why?
|
the aortic arch, not the GE junction.
1. aorta causes extrinsic compression 2. zone of low pressure, at the junction of the smooth and striated muscle |
|
|
|
True or False
Chronic sequellae from radiation can occur years after exposure and can include stricture, fistula and even complete obstruction. |
True
|
|
|
|
What's a cutoff sign?
|
A ratty irregular "cut off" in the esophagus leading to a stenosis. It indicates a neoplastic growth.
|
|
|
|
Neoplastic types of esophageal dysphagia?
SALLy Met FiliP |
Squamous Cell carcinoma
Adenocarcinoma Leiomyoma Lymphoma Metastatic ca Fibrovascular polyp Lipoma squamous Papiloma |
|
|
|
infectious types of esophageal dysphagia?
CHeCHi |
Candida
Herpes simplex (HSV) Cytomegalovirus (CMV) HIV |
|
|
|
Some congenital problems that cause esophageal dysphagia
SAAD |
Stenosis
Atresia Aortic Arch anomalies Duplication |
|
|
|
The clinical approach to swallowing disorders (esophageal) includes:
HETT |
History
Exam Tests Treatment |
|
|
|
Three broad categories of medical treatment for esophageal dysphagia?
MES |
Medical therapy
Endoscopic therapy Surgical therapy |
|
|
|
What are three diagnostic procedures used in the diagnosis of esophageal dysphagia?
|
UGI/Esophagram/TBS
UEE (Endoscopic exam) Esophageal Manometry (Hi res) |
|
|
|
True or false
In hi resolution esophageal manometry the x axis is distance down the UES, the y-axis is time, and color indicates pressure. |
False
x axis is time y axis is distance |
|
|
|
What's the esophagus lined with?
|
Squamous epithelium
|
|
|
|
There's one pharynx to serve several functions, some more important than others. What's the heirarchy?
|
1. respiration
2. swallowing 3. speech |
|
|
|
Three general aspects of respiration are:
|
ventilation (air in and out)
external respiration (gas exchange in lungs) internal respiration (gas exchange in body) |
|
|
|
The ___ and ___ (body structures) function as a respiratory unit
|
thorax
abdomen |
|
|
|
Which zone (subdivision of the respiratory system) brings air into and out of the lungs?
|
conducting zone
|
|
|
|
Which zone (subdivision of the respiratory system) is where gas exchange occurs?
|
respiratory zone
|
|
|
|
The trachea is a tube located within the _____. The tube is lined with ____ and supported by _____ made of _____. It extends from the _____ at the ___ (level of the spine) and bifurcates at about ____ (level of the spine), where it divides into two ____
|
The trachea is a tube located within the THORAX. The tube is lined with MUCOUS MEMBRANE and supported by CARTILAGINOUS RINGS made of HYELIN. It extends from the LOWER BORDER OF THE CRICOID at C6 (level of the spine) and bifurcates at about T5 (level of the spine), where it divides into two BRONCHI
|
|
|
|
The right and left bronchi differ in ____, ____, and ____.
|
angulation, diameter, and length
|
|
|
|
Each bronchus enters the lung through its ____
|
hilus
|
|
|
|
True or False
Respiratory bronchioles are still ciliated and cartilaginous but have alveoli budding off them. |
True
|
|
|
|
How many bronchial divisions take place?
|
20
|
|
|
|
What's the final bronchial termination called (at the blind ends of the tube)
|
pulmonary alveolus
|
|
|
|
The respiratory tract begins superiorly with the _____ and _____. From there, air is conducted into and out of the ____, through the ___ and into the ____ from which it moves into the ____.
|
The respiratory tract begins superiorly with the TWO NASAL PASSAGES and MOUTH. From there, air is conducted into and out of the PHARYNX, through the LARYNX and into the TRACHEA from which it moves into the LUNGS.
|
|
|
|
The ____, ____, and ____ belong to the respiratory conducting zone
|
trachea, bronchi, bronchioles
|
|
|
|
The ___, ___ and ___ belong to the respiratory zone
|
respiratory bronchioles, alveolar ducts, alveolar sacs
|
|
|
|
True or False
An alveolar sac is a pouch-like evagination of the walls of the respiratory broncholes and alveolar ducts. |
False
An alveolus (pl alveoli) is a pouch-like evagination of the walls of the respiratory bronchioles, alveolar ducts and alveolar sacs |
|
|
|
O2-CO2 exchange occurs by ____ in the alveoli. Why (ish)?
|
diffusion
alveoli have large surface areas |
|
|
|
Each alveous shares a wall that is ____ thick with ______ through which _____ takes place
|
one cell thick
vascular capillaries external respiration |
|
|
|
Without ____, the Law of LaPlace predicts that a small alveolus will _____ (called ____)
|
surfactant
collapse atelectasis |
|
|
|
True or False
Surfactant decreases lung compliance |
False
increases it. |
|
|
|
True or False
A small alveolus has a higher collapsing pressure than a larger alveolus. |
True
|
|
|
|
______ generates a pressure that can collapse alveoli.
|
surface tension
|
|
|
|
P=2T/r
What is it? |
The Law of LaPlace
P=pressure T=surface tension r=radius of alveolus |
|
|
|
____ is a mixture of phospholipids that line ____ and do what?
|
surfactant
alveoli reduce their surface tension |
|
|
|
Lungs have 2 surfaces, right?
|
Sure, costal (rib) and mediastinal
|
|
|
|
True or False
There are four right and three left pulmonary lobes |
False
Three right and two left |
|
|
|
Lungs are covered by 2 ____, the ____ and the ____, which are fused together at the ___. Space between them is called ____ or ____.
|
pleurae
pulmonary pleura parietal pleura hilus pleural cavity or intrapleural space |
|
|
|
Is pressure in the intrapleural space positive or negative?
|
negative
|
|
|
|
The change in lung volume for a given change in pressure is called?
|
lung compliance
|
|
|
|
There exists an inverse relationship between _____ of lungs and chest wall and their ______.
|
compliance
elastance (elastic properties) |
|
|
|
If the pressure of the intrapleural space is equivalent to the outside air pressure (and pressure w/in the lungs), what happens
|
A pneumothorax (lung will collapse)
|
|
|
|
Is respiration a pumping action?
|
yup
|
|
|
|
with ____ inhalation, few muscles are used.
|
quiet
|
|
|
|
with ____ inhalation, muscles enlarge the volume of the thorax and decrease pressure within the thorax so air will flow into the lungs.
|
forced
|
|
|
|
with ____, compressive pumping action decreases the volume of the thorax and increases pressure on air within the lungs.
|
exhalation
|
|
|
|
2 ways to decrease thoracic air pressure
|
thoracic (chest wall) enlargement
increase vertical dimension of the thorax (diaphragm) |
|
|
|
2 major muscles of inspiration
|
diaphragm
external intercostals |
|
|
|
3 minor muscles of inspiration
|
scalenae
pectoralis majoris et minoris |
|
|
|
major muscle of expiration
|
internal intercoastals
|
|
|
|
2 minor muscles of expiration
|
transverse thoracic
quadratus lumborum |
|
|
|
4 Abdominal muscles involved in respiration
|
rectus abdominus
oblique externis oblique internis abdominus transversus |
|
|
|
What's happening?
Active musculature expands thoracic volume to decrease internal pressure |
quiet inhalation
|
|
|
|
What's happening?
Relaxation of muscles of inhalation, so ribs and/or diaphragm muscle return to their rest positions, decreasing thoracic volume and increasing thoracic pressure |
quiet exhalation
|
|
|
|
What muscle groups help during active inhalation?
|
scalenes, sternocleidomastoid (elevate thorax)
also pecs |
|
|
|
What muscle groups aid in forced exhalation?
|
internal intercostals
quadratus lumborum, transverse thoracic |
|
|
|
Which lung volume includes the volume that fills alveoli plus the volume that fills the airways during quiet breathing?
|
tidal volume
|
|
|
|
The additional volume that can be inspired above tidal volume is ___, whereas the additional volume that can expired below tidal volume is ___
|
inspiratory reserve volume
expiratory reserve volume |
|
|
|
Volume of gas in lungs after maximal forced expiration is called
|
residual volume
|
|
|
|
Each ____ includes two or more lung volumes.
|
lung capacity
|
|
|
|
Tidal volume + IRV =
|
Inspiratory capacity
|
|
|
|
Tidal volume + ERV + IRV =
|
vital capacity
|
|
|
|
total of all lung volumes
|
total lung capacity
|
|
|
|
ERV + RV, The amount of air left in the lungs after a tidal breath out.
|
functional residual capacity
|
|
|
|
Systems important in swallowing
SPORN! |
Sensory
Pharyngeal/Laryngeal Oral/Nasal Respiratory Neurologic |
|
|
|
What's the boundary between the upper and lower airway
|
larynx
|
|
|
|
The primary airway is through the
|
nose
|
|
|
|
Four main valves in the upper airway
|
oral
nasal pharyngeal tube laryngeal tube |
|
|
|
Normal respiratory rate:
Young: Old: |
Young: 16/min
Elderly: 20/min |
|
|
|
Maintaining airflow pressure is dependent on ___, ____, and ___
|
muscle control, exhalatory forces, and adequate valving
|
|
|
|
What's the most common pattern coordination of respiration and swallowing and what percentage of people use it?
|
Inhale
start to exhale stop and swallow exhale some more 60-80% |
|
|
|
How long does one normally stop breathing (pause) while swallowing?
What's the pause called? |
1/3-2/3 of a second depending on bolus size.
Apneic pause (apnea) |
|
|
|
At what age is coordination of respiration and swallowing less consistent.
|
Under 3 months and over 70 years
|
|
|
|
When the _______ of the bolus reaches the _____, the airway closes. It remains closed until _____
|
leading edge
top of the airway the tail of the bolus passes the AE |
|
|
|
Which types of patients might close the AE earlier during a swallow
|
older patients, (60+)
|
|
|
|
Information about respiration critical for swallowing:
BASE |
B3 BREATHING
Focal point of breathing rate of respiration pneumonia history (last year) S3 SWALLOW rate of swallowing efficiency of swallow no more than 1/2 of swallows interrupted by inhalation A3 ASPIRATION/penetration drooling/buildup of saliva no coughing/gurgly voice/throat clearing chronic bronchial secretions/bronchorrhea E2 EXTRANEOUS dietary intake risky diagnoses |
|
|
|
Curvature of the spine aka
|
kyphosis (inhibits respiration)
|
|
|
|
4 things that can restrict expansion of the lungs, limiting the ability of the lungs to draw in air:
|
paralysis
kyphosis pain (e.g. pleursy) alveolar noncompliance |
|
|
|
Some Restrictive pulmonary conditions. Say, 8.
SAFE PAPP |
Pneumothorax
Atelectasis Pleural Effusion Edema (pulmonary) Asthma Sepsis (leading to Ad Resp Distress Syn) Paralysis Fibrosis (pulmonary) |
|
|
|
____is defined as a state in which the lung, in whole or in part, is collapsed or without air. It is a condition where the alveoli are deflated, as distinct from pulmonary consolidation.
|
atelectasis
The most common cause is post-surgical atelectasis, characterized by splinting, restricted breathing after abdominal surgery. Smokers and the elderly are at an increased risk. Outside of this context, atelectasis implies some blockage of a bronchiole or bronchus, which can be within the airway (foreign body, mucus plug), from the wall (tumor, usually SCC) or compressing from the outside (tumor, lymph node, tubercle). Another cause is poor surfactant spreading during inspiration, causing an increase in surface tension which tends to collapse smaller alveoli. |
|
|
|
perforated pleurae aka
|
pneumothorax
|
|
|
|
Obstructive Pulmonary Conditions aka (2 types)
|
Chronic obstructive pulmonary disease
emphysema chronic bronchitis |
|
|
|
Acute lung injury caused by acidic and particulate gastric contents (GERD)
|
Pneumonitis
|
|
|
|
acute pulmonary inflammation caused by infection: reaction to bacteria and bacterial byproducts. Is it fatal?
|
aspiration pneumonia
Yup, in 20-50% of cases |
|
|
|
___ is a difficulty in breathing caused by a sudden constriction of the muscles in the walls of the bronchioles (as in asthma)
|
bronchospasm
|
|
|
|
the production of more than 100 mL per day of watery sputum
|
bronchorrhea
|
|
|
|
____ refers to the bluish coloration of the skin due to the presence of deoxygenated hemoglobin in blood vessels near the skin surface. It occurs when the oxygen saturation of arterial blood falls below 85%.
|
cyanosis
|
|
|
|
____ or short of breath (SOB) is perceived difficulty breathing or pain on breathing.
|
dyspnea
|
|
|
|
___ is the expectoration (coughing up) of blood or of blood-stained sputum from the bronchi, larynx, trachea, or lungs (e.g. in tuberculosis or other respiratory infections).
|
hemoptysis
|
|
|
|
An abnormal deficiency in the concentration of oxygen in arterial blood. A frequent error is made when the term is used to describe poor tissue diffusion.
|
Hypoxemia
Hypoxia is poor tissue diffusion |
|
|
|
the state of breathing faster and/or deeper than necessary, thereby reducing the carbon dioxide concentration of the blood below normal.
|
Hyperpnea
|
|
|
|
an abnormal or adventitious sound heard when listening to the chest as the person breathes, a coarse rattling sound somewhat like snoring, usually caused by secretion in bronchial airways
|
Rhonchi
|
|
|
|
Assessment of Respiration for Swallowing (4 parts)
HOSP |
History taking (+chart review)
Observations Specific Tasks Planning treatment using assessment |
|
|
|
Is this abnormal? Greater than 2-3 saliva swallows in 5 minutes.
|
Nope. Less than 2-3 saliva swallows in 5 minutes is, though.
|
|
|
|
Specific tasks to check respiration include:
BCMN ahasa |
Breath hold Cough Maneuvers Name repetition
Prolonged voluntary breath hold (1, 3, 5, 10 seconds) Cough and throat clear with and without abdominal support AND with and without shoulder girdle stabilization SG and SSG maneuvers Prolong vowel /a/ (1, 2, 5 sec) repeat name soft, loud, medium Sustain /s/ Repeat /ha/ Sustain /a/ while changing pitch |
|
|
|
If respiratory status is severe, plan to work on:
|
respiration first (not nec. your job); may decide not to work on speech or swallowing immediately
|
|
|
|
If less than half the swallows have ____ between swallowing and respiration, consider working on ____
|
normal coordination
swallow-respiratory coordination |
|
|
|
True or False
Timing of swallow: oral onset and transit should be no more than 2 seconds, otherwise it can be a strain on the respiratory system |
True
|
|
|
|
What should the focus of therapy be?
|
Improving the underlying respiratory problem?
Improve the speed of the swallow? Improving respiratory control? |
|
|
|
the risk of head injury is especially high among__, __, & __
|
15-25 year-olds, persons over 75, kids under 5
|
|
|
|
True or False
For persons of all ages, the risk of head injury among males and females is roughly equivalent. |
False
twice as high for males |
|
|
|
3 most common causes of TBI
|
vehicle-related accident (>50%)
falls (25%) violence (20%) |
|
|
|
3 common successive stages of TBI:
|
Coma
Post-traumatic amnesia Recovery |
|
|
|
An injury that causes swelling in the brain that restricts the flow of blood-borne oxygen,glucose, and other nutrients.
|
hypoxic-ischemic injury
|
|
|
|
Brain damage characterized by microscopic damage throughout many areas of the brain. Shearing of large nerve fibers and stretching of blood vessels in many areas of the brain. The ___ and ___ lobes are particulary susceptible.
|
Diffuse injuries
frontal and temporal |
|
|
|
Brain damage confined to a specific area of the brain and causing localized damage that can often be detected by CT or x-ray
|
Focal brain injury
|
|
|
|
Bruises that cause swelling, bleeding, and destruction of brain tissue. _____ typically affect the ____ and ___ lobes.
|
contusions
frontal & temporal |
|
|
|
Cerebral or intracranial blood leak from damaged vessel in brain tissue.
|
Hemorrhage
|
|
|
|
Occurs in TBI when an artery to the brain is compressed by swelling of surrounding tissues, preventing flow of blood-borne oxygen to the brain.
a macroscopic area of necrotic tissue in some organ caused by loss of blood supply. Supplying arteries may be blocked from within by some obstruction (e.g. a blood clot or cholesterol deposit), or may be mechanically compressed or ruptured by trauma. |
infarction
Infarctions are commonly associated with atherosclerosis, where an atherosclerotic plaque ruptures, a thrombus forms on the surface occluding the blood flow and occasionally forming an embolus that occludes other blood vessels downstream. |
|
|
|
80% of ___ are due to infarction.
|
Strokes/CVAs
|
|
|
|
a form of traumatic brain injury in which blood collects between the dura (the outer protective covering of the brain) and the arachnoid (the middle layer of the meninges). This bleeding often separates the dura and the arachnoid layers.
|
Subdural hematoma
Unlike in epidural hematomas, which are usually caused by tears in arteries, subdural bleeding usually results from tears in veins that cross the subdural space. Subdural hemorrhages may cause an increase in intracranial pressure (ICP), which can cause compression of and damage to delicate brain tissue. |
|
|
|
a buildup of blood occurring between the dura mater (the brain's tough outer membrane) and the skull. Often due to trauma, the condition is potentially deadly because the buildup of blood may increase pressure in the intracranial space and compress delicate brain tissue.
|
Epidural or extradural hematoma
|
|
|
|
bleeding into the subarachnoid space surrounding the brain, i.e., the area between the arachnoid membrane and the pia mater. It may arise due to trauma or spontaneously, and is a medical emergency which can lead to death or severe disability even if recognized and treated in an early stage.
|
subarachnoid hemorrhage
|
|
|
|
True or False
Complications from TBI can develop weeks or months after the initial injury |
True
|
|
|
|
a condition in which abnormal accumulation of cerebrospinal fluid (CSF) in the brain causes increased intracranial pressure inside the skull. This is usually due to blockage of CSF outflow in the brain ventricles or in the subarachnoid space at the base of the brain.
|
hydrocephalus
|
|
|
|
A Focal brain injury characterized by an accumulation or blood or spinal fluid on the surface of the brain, exerting pressure. Symptoms of this chronic secondary complication have a slower onset than those of epidural hemorrhages because the lower pressure veins bleed more slowly than arteries. Thus, signs and symptoms may show up within 24 hours but can be delayed as much as 2 weeks
|
chronic subdural hematoma
|
|
|
|
3 stages of medical treatment for TBI
|
Acute
Subacute Chronic |
|
|
|
Stage of medical treatment wherein the patient is stabilized immediately after the TBI
|
acute
|
|
|
|
Stage of medical treatment wherein the TBI patient is rehabilitated and returned to the community
|
Subacute
|
|
|
|
Stage of medical treatment wherein the TBI patient continues rehabilitation and treats long-term impairments
|
chronic
|
|
|
|
What is...
In cases of hydrocephalus, a one-way valve that is used to drain excess cerebrospinal fluid from the brain and carry it to the peritoneal cavity. This valve usually sits outside the skull, but beneath the skin, somewhere behind the ear. |
ventriculo-peritoneal shunt
|
|
|
|
Two categories of chronic treatment:
|
community based (rehab & return to work/school)
treatment of long-term consequences |
|
|
|
The most common swallowing disorder in TBI cases with brainstem damage
|
DTriPS
cortex is modulation....not sure what that means... |
|
|
|
The ____ during the swallow can cause stress in a compromised respiratory system
|
apneic pause
|
|
|
|
Some oral disorders seen in TBI (3)
|
Rd Lip closure
Rd ROM of OT w/ poor bolus control Abn oral reflexes |
|
|
|
8 "neuromuscular abnormalities" aka swallow disorders associated with TBI during the pharyngeal stage of the swallow
L AE TB AC UES PW VP F |
L AE TB AC UES PW VP F
Rd Lg Elev Rd AE closure Rd TB retraction Rd AC Rd UES opening Rd VP closure Uni/Bi PW paresis/paralysis Rd VP closure Tracheoesophageal fistula |
|
|
|
Any other reasons for dysphagia in a TBI patient other than the TBI itself?
TIPPL |
Tracheostomy too high
Intubation Penetration wounds Puncture wounds Laryngeal fracture |
|
|
|
About ___ of patients with SCI also have a head injury
|
1/3
|
|
|
|
A/An _____ SCI shows no function below the level of the injury, no sensation, and no voluntary movement. (bilateral)
|
complete
|
|
|
|
A/An ____ SCI shows some function below the primary level of the injury
|
incomplete
|
|
|
|
Swallowing problems in SCI patients may be exacerbated by (3)
|
trach
cervical brace mechanical vent |
|
|
|
Injury at C1 or C2 (nature of swallowing difficulty)
|
no sensory awareness of difficulty
|
|
|
|
Injury at C4, 5 and/or 6 (nature of swallowing difficulty)
|
poor laryngeal movment and reduced UES opening, occasional AE closure (not TVF) problems
|
|
|
|
What treatments are typically most helpful for patients with SCI?
|
swallow maneuvers (if no TBI/cognition ok)
sensory enhancement postures not so much bec. of brace etc |
|
|
|
Types of CSI braces? (4)
SHoPS |
Soft collar
Philadelphia collar SOMI (sterno-occipital mandibular immobilization) Halo |
|
|
|
What treatment is most helpful for dysphagia in patients with ACF (anterior cervical fusion)
|
swallow maneuvers such as mendelsohn supraglottic, super-supraglottic
|
|
|
|
True or False
duration of recovery reflects the number of complications with ACF |
Troo
|
|
|
|
If the medulla is affected...
What swallowing disorders? What sorts of symptoms? What to try? |
DTriPS and APS
OT, TB, Lg struggling Try TTS and SS |
|
|

What's A and how much is it?
|
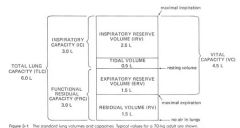
Total Lung Capacity (6.0L)
|
|
|

What's B?
|
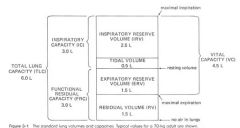
Inspiratory Capacity (3.0L)
|
|
|

What's C?
|
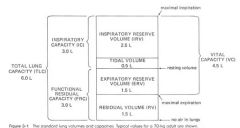
Functional Residual Capacity
|
|
|

What are D & E? Together they make up what?
|
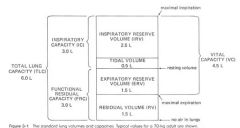
Inspiratory reserve volume and tidal volume.
Inspiratory capacity |
|
|

What's F & G?
What do they make up? |
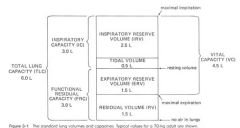
Expiratory Reserve Volume and Residual Volume
Functional Residual Capacity |
|
|

What's H?
What's it made of? |
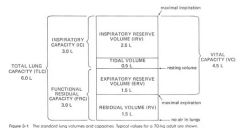
Vital Capacity
IRV + TV + ERV |
|
|
|
Jones et al (1985) argue that simultaneous disorders of the pharynx and esophagus are:
|
so frequent that the complete swallowing chain should be examined in all patients with dysphagia.
|
Jones et al, (1985) Pharyngoesophageal interrelationships: observations and working concepts
|
|
|
According to Jones et al (1985) a cricopharyngeal prominence:
|
may be a clue to esophageal disease
|
Jones et al, (1985) Pharyngoesophageal interrelationships: observations and working concepts
|
|
|
In Logemann & Bytell (1979), the authors argue that anterior floor of mouth resection patients (HN Ca) have problems with:
|
preparation for the swallow and oral transit
|
Logemann & Bytell (1979) Swallowing Disorders in three types of head and neck surgical patients.
|
|
|
Logemann & Bytell (1979) demonstrate that HN Ca pts with tonsil/base of tongue resection have:
|
slowing in preparation for the swallow and in oral and pharyngeal stages of the swallow
|
Logemann & Bytell (1979) Swallowing Disorders in three types of head and neck surgical patients.`
|
|
|
Logemann & Bytell (1979) examined HN Ca pts and found that after supraglottic laryngectomy, patients:
|
show only slight slowing in oral transit and pharyngeal transit (as compared to other types of surgical patients)
|
Logemann & Bytell (1979) Swallowing Disorders in three types of head and neck surgical patients.
|
|
|
According to Logemann & Bytell (1979) what factors other than the amount of tongue resected may be important in determining the extent of postoperative dysfunction in HN Ca pts?
|
oral sensitivity
nature of closure/reconstruction |
Logemann & Bytell (1979) Swallowing Disorders in three types of head and neck surgical patients.
|
|
|
What procedure did McConnel et al (1986) find useful in examining laryngectomy patients
|
Manofluorography
|
McConnel et al (1986) Examination of swallowing after total alryngectomy using manofluorography
|
|
|
According to McConnel et al (1986) which laryngectomy group showed the longest pharyngeal transit times?
|
total laryngectomies with tongue impairment
|
McConnel et al (1986) Examination of swallowing after total alryngectomy using manofluorography
|
|
|
What, according to McConnel et al (1986) offered greater resistance to bolus flow?
|
The postlaryngectomy pharynx
|
McConnel et al (1986) Examination of swallowing after total alryngectomy using manofluorography
|
|
|
What did manofluorography of laryngectomy patients show, according to McConnel et al (1986)?
|
the importance of the tongue in bolus propulsion in the pharynx
|
McConnel et al (1986) Examination of swallowing after total alryngectomy using manofluorography
|
|
|
According to Logemann, et al (1994), what should the focus of swallowign therapy be after supraglottic laryngectomy? What therapy approaches were used?
|
improvement of posterior movment of the tongue base and anterior tilting of the arytenoid to close the airway entrance and improve bolus propulsion. SG & SSG
|
Logemann et al (1994) Mechanisms of recovery of swallow after supraglottic laryngectomy.
|
|
|
Robbins & Levine (1988) determined that left cortical stroke dysphagia was characterized by
|
impaired oral stage function,
difficulty initiating coordinated motor activity apraxia |
Robbins & Levine (1988) Swallowing after unilateral stroke of the cerebral cortex: preliminary experience
|
|
|
Robbins & Levine (1988) determined that right cortical stroke dysphatia was characterized by
|
pharyngeal pooling
penetration aspiration |
Robbins & Levine (1988) Swallowing after unilateral stroke of the cerebral cortex: preliminary experience
|
|
|
Robbins & Levine (1988) argue that distinct patterns of dysphagia after unilateral cortical stroke challenge what:
|
the traditional classification of swallowign as a bilateral and brainstem-mediated activity
|
Robbins & Levine (1988) Swallowing after unilateral stroke of the cerebral cortex: preliminary experience
|
|
|
According to Horner et al (1988) what's a common clinical characteristic of aspirating patients (following stroke)
|
dysphonia
|
Horner et al (1988) Aspiration following stroke: clinical correlates and outcome
|
|
|
In the study conducted by Horner et al (1988), of the stroke patients studied, ___ aspirated. Which were at greatest risk?
|
1/2
Those with combined cerebral-brainstem strokes with bilateral cranial nerve signs |
Horner et al (1988) Aspiration following stroke: clinical correlates and outcome.
|
|
|
True or False
Horner et al (1988) found that compensatory feeding approaches did not prevent aspiration pneumonia |
False
It did. They argue it's just as effective as indirect swallowing therapy, though I'd like to see you enjoy your dinner in mouthfuls of less than a teaspoon. |
Horner et al (1988) Aspiration following stroke: clinical correlates and outcome.
|
|
|
According to Lazarus (1993) what can result in immediate and long term changes in swallow functioning in HN Ca pts?
|
Radiation therapy
|
Lazarus (1993) Effects of radiation therapy and voluntary maneuvers on swallow functioning in head and neck cancer patients.
|
|
|
According to Lazarus (1993) what was effective in improving extent and duration of tongue base retraction, laryngeal elevation, and laryngeal vestibule and true vocal cord closure?
|
SSG & MM
|
Lazarus (1993) Effects of radiation therapy and voluntary maneuvers on swallow functioning in head and neck cancer patients.
|
|
|
Martin et al (1994) found that ____ was usually maintained at the onset of deglutition and ___ before the onset of _____.
|
respiration
halted laryngeal elevation |
Martin et al (1994) Coordination between respiration and swallowing: respiratory phase relationships and temporal integration.
|
|
|
According to Martin et al (1994), what respiratory phase brackets small volume liquid swallowing activity?
|
expiration
|
Martin et al (1994) Coordination between respiration and swallowing: respiratory phase relationships and temporal integration.
|
|
|
True or False
According to Martin et al (1994), Discoordination between swallowing and respiration may increase the potential for aspiration |
True
|
Martin et al (1994) Coordination between respiration and swallowing: respiratory phase relationships and temporal integration.
|
|
|
According to Lazarus et al (1996), oral and pharyngeal motility for swallow can become compromised if what is provided to either what or what?
|
external-beam radiation treatment
larynx or tongue base regions |
Lazarus (1996) Swallowing disorders in head and neck cancer patients treated with radiotherapy and adjuvant chemotherapy.
|
|
|
In Lazarus et al (1996), what sordts of swallow disorders were seen in HN Ca pts treated with radiation and chemo?
|
reduced coordination and abnormal timing of pharyngeal events
|
Lazarus (1996) Swallowing disorders in head and neck cancer patients treated with radiotherapy and adjuvant chemotherapy.
|
|
|
Logemann et al (1994) found that postural techniques were successful in eliminating aspiration ____ in ____ of patients.
|
on at least one volume of liquid in 81%
|
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
Delay in triggering the pharyngeal swallow. What postural change?
|
Head down
|
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
Delayed oral transit time. What postural change?
|
Head lifted
|
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
Reduced laryngeal elevation (liquid enters laryngeal vestibule and is inhaled after swallow)
And the posture recommended by Logemann et all (1994) is? But... |
Head down
other research shows head rotated... right? |
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
Reduced laryngeal closure (Bolus passes through larynx and into trachea during pharyngeal phase of swallow)
|
Head rotated to damaged side, SGS
|
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
Unilateral pharyngeal weakness
And the posture suggested by Logemann et al (1994) is? |
Head rotated to damaged side
|
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
According to Logemann et al (1994), what posture best helps impaired cricopharyngeal opening/reduced anterior laryngeal movement?
|
head rotated
|
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
Reduced pharyngeal clearance
And the correct posture, according to Logemann et al (1994), is? |
lying on side
|
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
According to Logemann et al (1994) patients receiving the least benefit from postures tended to be those:
|
with resections involving more than one structure.
|
Logemann et al (1994) Effects of postural change on aspiration in head and neck surgical patients
|
|
|
Sharp & Genesen (1996) advocate the use of a _____ for identifying and negotiating ethical dilemmas.
|
systematic framework
|
Sharp & Genesen (1996) Ethical decision-making in dysphagia management.
|
|
|
True and False
In the clinical ethics model, according Sharp & Genesen (1996), patient preferences and medical indications take precedence over quality of life and contextual features. |
True
|
Sharp & Genesen (1996) Ethical decision-making in dysphagia management.
|

