![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
113 Cards in this Set
- Front
- Back
|
What is obstructive jaundice?
|
decreased flow of bile through the liver or biliary duct system
|
|
|
What is Hemolytic Jaundice?
|
when jaundice is caused by an increased break down of RBC producing an increased amount of unconjugated bilirubin in the blood
|
|
|
What is Hepatocellular Jaundice?
|
the inability of the liver to take up bilirubin from the blood, conjugate it, or excrete it (but does have bilirubin in urine)
|
|
|
What is the difference between Conjugated and Unconjugated bilirubin?
|
Unconjugated bilirubin is not water soluable so it attaches to hemoglobin
Conjugated bilirubin is unconjugated bilirubin after it has been broken down to be water soluable (excreted in bile) |
|
|
What is the pathophysiology of hepatitis?
|
Inflammation of the Liver (cell injury) that causes the liver to autolyse leading to necrosis
it is able to regenerate if in the acute phase |
|
|
How are the different types of Viral Hepatitis transmitted?
|
A - fecal oral
B - blood C - blood D - blood (only if you have B) E - fecal oral |
|
|
What are the stages of Viral hepatits?
|
Acute (icteric)
chronic (convalescent stage) |
|
|
What are the different causes of Hepatitis?
|
Viral
Toxins Chemicals |
|
|
What are the symptoms of viral acute hepatits?
|
JAUNDICE
FLU like Sx Lethargy Irritability Myaligia Arthralgia Anorexia Itching Indigestion N/V Abdominal pain Diarrhea or Constipation Fever Appetite Loss 1-4 months |
|
|
What are the symptoms of viral chronic (convelescent) stage hepatitis?
|
Begins with the resolution of jaundice
Fatigue Flatulence Abdominal Pain indigestion 2-6weeks prognosis is poor if edema or encephalopathy develop |
|
|
What are the characteristics of Chronic hepatitis?
|
inflammation of the liver lasting longer than 3-6months
|
|
|
What is the treatment for Chronic Hepatitis B?
|
mainly in males
Epivir Intron A for 16 weeks |
|
|
What is the treatment for Chronic Hepatitis C?
|
Usually progresses to end stage cirrosis
IFN-alfa ribavirin |
|
|
What are the complications of Hepatitis?
|
Acute viral hepatitis usually recovers without Complications
Fulminant Hepatic Failure Chronic Hepatitis Cirrhosis Hepatocellular Carcinoma |
|
|
What is fulminant hepatic failure?
|
severe impairment or necrosis of the liver cells and potential liver failure
Occurs b/c of: Cx of Hep B Toxic reactions to Rx and congenital metabolic disorders |
|
|
What is important to understand about Toxic and Drug induced hepatitis?
|
the type and extent of necrosis depends on the degree of exposure
Necrosis begins 2-3 days after acute exposure |
|
|
What is important to understand about alcoholic Hepatitis?
|
can be acute or chronic
Caused by parenchymal necrosis resulting from heavy alcohol ingestion most frequent cause of cirrhosis of the liver |
|
|
Name the types of Autoimmune Hepatitis?
|
Wilson's Disease
Hemochromatosis Primary Biliary Cirrhosis Non-alcoholic Fatty Liver Disease and Non-alcoholic steatohepatitis |
|
|
What is Wilson's disease?
|
a genetic neurological disease accompanied by chronic liver disease leading to cirrhosis
|
|
|
What is Hemochromatosis?
|
a systemic disease that includes the malabsorption of iron (too much iron)
|
|
|
What is Primary Biliary Cirrhosis?
|
Chronic inflammation of the liver with genetics and environment playing a role
|
|
|
What is Nonalcoholic Fatty Liver Disease?
|
a group of diseases in which there is hepatic steatosis (accumulation of fat in the liver)
It can lead to scarring and inflammation which and increase the chance of liver cancer and liver failure |
|
|
What are the diagnostic tests and treatment for Nonalcoholic Fatty Liver Disease?
|
Diagnostic Tests:
Elevated liver tests (ALT AST) Eventually decreased albumin Increased bilirubin and PT Treatment: Weight reduction |
|
|
What are the diagnostic tests for hepatitis?
|
AST (inc then dec with jaundice being resolved)
ALT (same) GGT (inc levels) Alkaline phosphatase (inc) Serum proteins (dec albumin) Serum Bilirubin (inc) Urinary Bilirubin (Inc) Urinary Urobilinogen (inc 2-4 days before jaundice) PT (prolonged) |
|
|
What is the general care for hepatitis?
|
no specific therapy for acute viral hepatitis (managed at home)
emphasis on resting the body (dec the demands on the liver) Relieve Itching - antihistamines, emollients, and lipid creams Parenteral Vit K for prolonged PT Avoid Chlorpromazine, ASA, Tylenol Antiemetics: Dramamine, Tigan, NO Phenothiazines Sedatives:Benadryl |
|
|
What is the drug therapy focused on for Hepatitis B?
|
Dec viral load
Dec liver enzymes Dec rate of disease progression Dec rate of drug resistant HBV |
|
|
What are the long term goals for hepatitis?
|
Prevention of cirrhosis and hepatocellular cancer
|
|
|
What is the drug therapy for Hepatitis B?
|
A Interferon
Nucleoside analogs: Epivir Hepsera |
|
|
How does A interferon work?
|
Multiple effects on viral replication cycle
SQ administration S/E: Flu-like Sx Depression Hair thinning Diarrhea Insomnia |
|
|
How do nucleoside analogs work?
|
when active viral replication exists, these drugs work by inhibiting viral DNA synthesis
they have beneficial effects in terms of reducing viral load, decreasing liver damage, and decreasing liver enzymes |
|
|
What is important to understand about Epivir?
|
first line of treatment and is taken for a year, but sometimes resistance is developed which is why Hepsera is prescribed
|
|
|
What are the goals of treatment for Hepatitis C?
|
Directed at eradicating the virus
Reducing viral load Decreasing progression of disease |
|
|
What drugs are used to treat hepatitis C?
|
Pegylated A Interferon with Ribivirin or Copegus
|
|
|
What are the side effects of Ribivirin?
|
Anemia
Anorexia cough rash puritis dyspnea insomnia teratogenicity |
|
|
How can you prevent Hepatitis A?
|
Hep A Vaccine (preexposure) IM
Immune Globulin (pre/post) giving temporary passive immunity |
|
|
How do you prevent Hepatitis B?
|
Immunization (most effective)
Hepatitis B IG |
|
|
What is important to understand about Hep B immunization?
|
part of routine vaccine for newborns, adolescents, and adults in major risk groups
Promotes synthesis of specific antibodies against Hep B given at 0,1,6months IM Recombivax HB (using recumbent DNA of HBsAg), Engerix-B |
|
|
What is important to understand about Hep B IG?
|
given with 24 hours of exposure
contains antibodies to HBV |
|
|
How can you prevent Hepatitis C?
|
no vaccine to prevent HCV
CDC doesn't recommend IG or antiviral agents for post exposure |
|
|
What is cirrhosis of the liver?
|
chronic progressive disease of widespread fibrosis (scaring) and nodule formation
|
|
|
What is the pathophysiology of cirrhosis?
|
irreversible injury
Hepatocyte necrosis causes collapse of the reticulin network (liver supporting structure) distorting the vascular bed and nodules are formed |
|
|
What are the types of cirrhosis?
|
Alcoholic (Laennec's) cirrhosis (micronodular, or portal) - fat accumulates
Postnecrotic (macronodular or toxin induced) - from Hep Biliary - r/t obstruction Cardiac - r/t R sided HF |
|
|
What are the risk factors for Cirrhosis?
|
Excessive alcohol ingestion
Viral Hepatitis for post necrotic Use of drugs (Tylenol, methotrexate, or isoniazid) Hepatic Congestion (cardiac type causes it to back up) |
|
|
What are the early manifestations of cirrhosis?
|
Onset is usually insidious
GI: anorexia, dyspepsia, flatulence, N/V, change in BM Abdominal pain Fever Lassitude Weight loss enlarged liver or spleen |
|
|
What are the late manifestations of cirrhosis?
|
Spider angiomas
palmar erythemia hematologic problems endocrine problems peripheral neuropathy **Jaundice: functional derangement of liver cells: compression of the bile ducts by overgrowth of connective tissues min or severe depending on liver damage Puritis if biliary tract is obstructed |
|
|
What are the complication of cirrhosis?
|
Portal HTN causing Esophageal varicies &Gastric varicies
Peripheral edema ascites Internal Hemorrhoids Hepatorenal syndrome Hepatic Encephalopathy Caput Medusae (ring of varices around the umbilicus) |
|
|
What is portal HTN characterized by?
|
increased venous pressure in portal circulation
Splenomegaly Ascites Large collateral veins Esophageal varicies Systemic hypertension the primary mechanism is increased resistance to blood flow through the liver |
|
|
What are the characteristics of esophageal varicies?
|
complex of tortuous veins at lower end of esophagus developing in areas where collateral and systemic circulations communicate
contain little elasticity and are fragile can bleed (life threatening complication) |
|
|
What can cause esophageal varicies to bleed?
|
alcohol
rough food acid regurgitation pressure to varicies |
|
|
Where are gastric varicies located?
|
in the upper portion of the stomach
|
|
|
What causes internal hemorrhoids in cirrhosis?
|
the dilation of the mesenteric veins and rectal veins
|
|
|
What is the treatment for esophageal and gastric varices?
|
Goal: avoid bleeding/hemorrhage
Avoid alcohol, ASA, and irritating foods Respiratory infection promptly treated (coughing causes bleed) Drugs: Sandostatin VP, Terlipressin NTG B adrenergic blockers |
|
|
What is the treatment for bleeding in esophageal and gastric varices?
|
stablize patient
manage airway provide IV therapy Give frozen plasma Packed RBC Vit K Zantac (dec GI acidity) Protonix Lactulose (prevent ammonia break down) Neomycin (dec bacteria) |
|
|
What kind of conservative treatment can be done for esophageal and gastric bleeding?
|
Endoscopic sclerotherapy
Endoscopic ligation Balloon Tamponade Shunting procedures (for secondary bleeding) |
|
|
What is endoscopic sclerotherapy in varices?
|
treatment for acute/chronic bleeding
Morrhuate is used to thromoses and obliterate the distended veins |
|
|
What is Endoscopic ligation in varices?
|
banding of varices and have fewer complications than sclerotherapy
|
|
|
What is balloon tamponade in varices?
|
controls hemorrhage by compression of varices using Sengstaken-Blakemore tube
|
|
|
What is the long term management in varices?
|
B adrenergic blockers
repeated sclerotherapy/band ligation Portosystemic shunts Propanolol (reduces portal pressure) |
|
|
What are the non-surgical shunts?
|
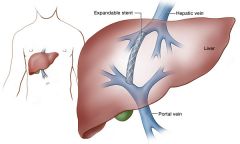
Transjugular Intrahepatic Portosystemic shunt (TIPS)
Shunts between systemic and portal venous system redirecting portal blood flow decreases portal venous pressure and decompresses varices |
|
|
What are the surgical shunting procedures?
|
Portacaval shunt
Distal splenorenal shunt (warren shunt) |
|
|
How does the portacaval shunt work?
|
decreases bleeding episodes
doesn't prolong life shunt causes ammonia to be diverted from the liver to the brain causing encephalopathy (death) |
|
|
How does the distal splenorenal shunt work?
|
leaves portal venous flow intact and dec the incidence of encephalopathy
with time it dec blood flow to the liver |
|
|
Why does edema occur with cirrhosis?
|
decreased colloidal pressure from impaired liver synthesis of albumin
Inc portacaval pressure from the portal hypertension occurs in ankle and presacral area |
|
|
What is ascites?
|
accumulation of serous fluid in peritoneal or abdominal cavity
abdominal distention with weight gain |
|
|
How do you treat ascites?
|
high CHO, low Na diet (2g/day)
Diuretics: Aldactone, Diuril, lasix (monitor K) Paracentesis: removing fluid temp from abdominal cavity Peritoneovenous shunt |
|
|
What is a peritoneovenous shunt?
|
continuous reinfution of ascitic fluid from the abdomen to the vena cava (not first tx)
Cx: thrombosis, infection, fluid overload, DIC |
|
|
What is hepatic encephalopathy?
|
Neuropsychiatric manifestation and terminal complication on liver disease
accumulation of ammonia in the brain because it isn't filtered by the liver |
|
|
How is hepatic encephalopathy graded?
|
0-4
4 being the most advanced (coma or not oriented) |
|
|
What are the manifestations of hepatic encephalopathy?
|
neurologic and mental responsiveness ranging from sleep disturbances to lethargy to deep coma
Asterixis (flapping tremors) Fetor Hepaticus |
|
|
What is fetor hepaticus?
|
musty, sweet odor on pt's breath caused by an accumulation of digestive by-products that the liver is unable to degrade
|
|
|
What is the treatment for hepatic encephalopathy?
|
Drugs: try to reduce the bacterial growth (breaks down amino acids into ammonia) by an antibiotic and laculose (makes GI acidic not allowing growth)
Nutritional therapy: Inc CHO, Inc Calories, dec fats, low protein (reduce ammonia) |
|
|
What is hepatorenal syndrome?
|
functional renal failure with:
azotemia oliguria intractable ascites with no structural abnormality of the kidney Splanchnic and systemic vasodilation and decreased arterial blood volume (r/t portal htn) renal vasoconstriction occurs with renal failure |
|
|
What are the diagnostic studies for cirrhosis?
|
Hx/physical
Labs: Liver Fx tests serum electrolytes CBC PT serum albumin stool for occult blood (varices) analysis of acidic fluid liver biopsy |
|
|
What is the treatment for cirrhosis?
|
Rest
B-complex vitamins Avoidance of ETOH, ASA, tylenol, and NSAIDS |
|
|
What are the nursing implementation for cirrhosis?
|
Health promotion
Acute intervention with bleeding varices and hepatic encephalopathy (monitor constipation - can worsen the coma, give laxatives) |
|
|
What is Acute pancreatitis?
|
acute inflammatory process of the pancreas r/t autodigestion of the pancreas caused by:
injury to the pancreatic cells activating the pancreatic enzymes biliary tract disease (women) alcoholism (men) hypertriglyceridemia |
|
|
What is the main symptom of acute pancreatitis?
|
Abdominal Pain **
located in RUQ or midepigastrium radiates to back sudden onset severe, deep, piercing, steady aggravated by eating onset when recumbent not relieved by vomiting |
|
|
What are other symptoms of acute pancreatitis?
|
Flushing
Cyanosis Dyspnea Edema N/V Bowel sounds decreased or absent Crackles- BS Discoloration of abdominal wall (grey spots r/t trypsin) Low grade fever Leukocytosis Hypotension tachycardia jaundice Abdominal tenderness |
|
|
What are the complications of acute pancreatitis?
|
Pseudocyst
Abscess Pulmonary: pleural effusion, atelectasis, pneumonia CV: hypotension Tetany (caused by hypocalcemia) |
|
|
Why are there pulmonary Cx in acute pancreatitis?
|
because exudate with trypsin (pancreatic enzyme) is moved through the lymph to the diaphragm and lungs
|
|
|
What is a pseudocyst?
|
cavity surrounding the outside of the pancreas filled with necrotic products and liquid secretions
may resolve spontaneously within a few weeks or may perforate causing peritonitis Treated by internal drainage procedure |
|
|
What are the symptoms of pseudocyst?
|
Abdominal pain
palpable epigastric mass N/V anorexia elevated serum amylase |
|
|
What is a pancreatic abscess?
|
a large fluid containing cavity within the pancreas resulting from extensive necrosis in the pancreas
|
|
|
What are the symptoms of a pancreatic abscess?
|
Upper abdominal pain
abdominal mass abscess may become infected or may perforate into adjacent organs fever leukocytosis requires surgical drainage |
|
|
What are the diagnostic tests of acute pancreatitis?
|
Abdominal/endoscopic US
x ray contrast CT (best for visualization of Cx) Endoscopic retrograde cholangiopancreatography (ERCP) |
|
|
What are the objectives for treatment for acute pancreatitis?
|
relieve pain
prevent or alleviation of shock dec pancreatic secretions Fluid and electrolyte balance prevention/treatment of infection removal of the precipitating cause |
|
|
What is the conservative treatment for acute pancreatitis?
|
Supportive:
Hydration Nutrition therapy Pain management (IV morphine + antispasmotic agent) Management of metabolic Cx Shock: plasma or plasma volume expanders (dextran or albumin) Fluid and Electrolyte: Lactated ringers solution Ongoing Hypotension: Inatropin Suppression of enzymes: NPO, NG suction |
|
|
When is surgery indicated in acute pancreatitis?
|
presence of gallstones
uncertain diagnosis unresponsive to conservative therapy abscess, pseudocyst, or severe peritonitis |
|
|
What surgical therapy can be done for acute pancreatitis?
|
ERCP
endoscopic spincterotomy laparoscopic cholecystectomy |
|
|
What drugs are given to treat acute pancreatitis?
|
IV morphine
NTG or papaverine Antispasmodics Carbonic anhydrase inhibitors (dec secreations) Antacids (neutralizes GI) H2 receptor blockers (dec HCL2) |
|
|
What nutrition therapy is given for acute pancreatitis?
|
NPO
IV lipids (monitor triglycerides) small frequent feedings Inc CHO, low fat, inc protein Supplemental fat soluable vitamins No alcohol |
|
|
What are the types of chronic pancreatitis?
|
Chronic obstructive pancreatitis
Chronic non-obstructive pancreatitis can occur with or without acute pacreatitis |
|
|
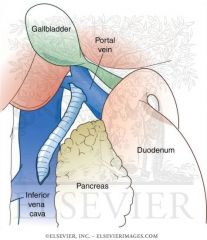
What are the causes of Chronic obstructed Pancreatitis?
|
biliary disease: inflammation of the sphincter of oddi associated with cholelithiasis (gall stones)
Cancer of ampulla of vater, duodenum, or pancreas |
|
|
What is chronic non-obstructive pancreatitis characterized by?
|
inflammation
sclerosis mainly in the head of the pancreas and around the pancreatic duct protein blocks ducts and it calcifies (alcohol induced) |
|
|
What are the clinical manifestations of Chronic pancreatitis?
|
Constipation
Mild jaundice with dark urine Steatorrhea Frothy urine/stool DM **Abdominal pain(burning cramp like) |
|
|
What are the complications of chronic pancreatitis?
|
Pseudocyst formation
pleural effusion Bile duct or duodenal obstruction pancreatic ascites Splenic vein thrombosis Pseudo-aneurysm Pancreatic cancer |
|
|
What are the diagnostic tests for chronic pancreatitis?
|
Based on S/S, lab results, and imaging
Labs: serum amalyse/lipase (inc) Inc bilirubin Inc alkaline phosphatase mild leukocytosis elevated sedimentation rate ERCP visualization of pancreatic/common bile duct (can unblock too) Stool samples CT MRI MRCP Transabdominal US EUS Secretin stimulation test |
|
|
How does a secretin stimulation test work?
|
secretin is administered
normally HCO3 is increased in chronic pancreatitis HCO3 is decreased |
|
|
What is the treatment for chronic pancreatitis?
|
prevention of attacks (during acute attacks, follow acute therapy)
relieve pain control pancreatic exocrine and endocrine insufficiency Bland low fat high CHO diet Bile salts (helps with absorption of fat soluable vit and prevents further fat loss) Control DM No alcohol Pancreatic enzyme replacement Acid neutralizing and acid inhibiting drugs |
|
|
When is surgery indicated for chronic pancreatitis?
|
biliary disease is present
obstruction or pseudocyst develops it diverts bile flow or relieves ductal obstruction |
|
|
What is the nursing care for chronic pancreatitis?
|
Dietary control
DM control Pancreatic enzymes with meals Antacids taken after meals |
|
|
What are the two forms of Gallbladder disease?
|
Cholelithiasis (gall stones)
Cholecystitis (inflammation usually associated with gall stones) |
|
|
What are the risk factors for gall bladder disease?
|
Women, multiparous women, and persons over 40
estrogen therapy Sedentary lifestyle Family tendency Obesity Navajo and Pima indians |
|
|
What are the causes of Cholecystitis?
|
gall stones or biliary sludge
In absence of obstruction: trauma, extensive burns, or recent surgery Bacteria (e. coli) Adhesions, Neoplasms, Anesthesia, opiods Inflammation |
|
|
How does the inflammation present in cholecystitis?
|
confined to mucous lining or entire wall
gall bladder is edematous and hyperemic may be distended with bile or pus: cystic duct my become occluded |
|
|
What is the pathophysiology of cholelithasis?
|
develops when the balance that keeps cholesterol, bile salts, and Ca in solution is altered caused by infection and disturbances in metabolism of cholesterol
|
|
|
What components of bile make the stones in cholelithiasis?
|
supersatuation of cholesterol (most common)
Bile salts Bilirubin Ca Protein |
|
|
What decreases bile flow creating a block?
|
Immobility
Pregnancy inflammatory or obstructive lesions |
|
|
Where are the stones normally formed in cholelithiasis?
|
may remain in the gall bladder or migrate to cystic or common bile duct
if blockage occurs in cystic duct, bile can continue to flow into the duodenum directly from the liver If blockage occurs in the gallbladder, it cannot escape the stasis and leads to cholecystitis |
|
|
When does pain occur in cholelithiasis?
|
when stone passes through ducts
small stones are more likely to lodge into the ducts and cause obstruction |
|
|
What are the manifestations of Gall Bladder disease?
|
pain can be after a heavy meal or lying down
indigestion moderate to severe pain RUQ fever jaundice |
|
|
What is the treatment for Cholecystitis?
|
pain management
Fluid and electrolyte balance antibiotics |
|
|
What are the treatments for cholelithiasis?
|
endoscopic sphincterotomy (widens duct)
Lithotripsy (dissolves with drugs) Lithrotriptor (shock waves) |

