![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
112 Cards in this Set
- Front
- Back
|
Atrioventricular valves |
- open at the beginning of diastole, allow blood to fill the ventricles - close at the beginning of ventricular contraction to prevent backflips of blood to the atria -mitral and tricuspid |
|
|
Semilunar valves |
-open at the end of ventricular contraction when the pressure in the ventricles exceed the pressure in the pulmonary artery and aorta
-close at the beginning of ventricular relaxation as the pressure in the chambers drops below the pressure in the pulmonary artery and aorta to prevent back flow into the ventricles -aortic and pulmonic |
|
|
Chordae tendinae |
Connect valve leaflets or cusps to papillary muscles
|
|
|
Papillary muscle |
Extension of the myocardium that pull cusps together and downward at the beginning of ventricular contraction to prevent backward expulsion of the AV valves into the atria |
|
|
Tricuspid valve |
- av - has three cusps - largest diameter of all valves |
|
|
Mitral valve |
-has two cusps (bicuspid) -resembles a cone shaped finnel |
|
|
Pulmonic and aortic valves |
Have 3 cup shaped cusps
Behave like one way swinging doors
Pulmonic slightly thinner than aortic |
|
|
Great vessels |
Superior and inferior vena canvae- veins to r atrium
Pulmonary artery- artery to lungs
Pulmonary veins- to left atrium
Aortic artery- to body |
|
|
Coronary artery |
Blood to the myocardium of the heart |
|
|
Coronary artery |
Blood to the myocardium of the heart |
|
|
Diastole |
Relaxation, blood fills ventricles |
|
|
Coronary artery |
Blood to the myocardium of the heart |
|
|
Diastole |
Relaxation, blood fills ventricles |
|
|
Systole |
Contraction, blood pumped out of the ventricles
Ejection of right ventricle slightly earlier than left due to pressure differences |
|
|
atrial contraction |
Right- blood enters from vena cave and coronary sinus
Left- blood enters from 4 pulmonary veins
Atria fills and distend-->opens AV valves
Blood passively fills ventricles
Atrial contraction provides the atrial kick - actively pumps additional blood into the ventricle |
|
|
Atrial kick |
Active pump of approx 25 mls of blood to ventricles |
|
|
Cardiac phase 1 |
Isovolumetric contraction
Ventricular volume is constant
Increase in ventricular pressure closes Av Valves
|
|
|
Cardiac phase 2 |
Increase in ventricular pressure opens semilunar valves and blood is ejected into circulation
Intraventricular volume and pressure deceea |
|
|
Cardiac phase 3 |
Isovoulmetric relaxation
Decrease in ventricular pressure close semilunar valves
Ventricles continue to relax |
|
|
Cardiac phase 3 |
Isovoulmetric relaxation
Decrease in ventricular pressure close semilunar valves
Ventricles continue to relax |
|
|
Cardiac phase 4 |
Decrease in ventricular pressure opens av valves
Permits ventricular filling from the atria |
|
|
The cardiac cycle |
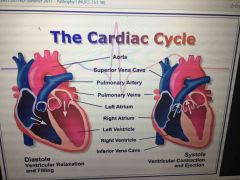
|
|
|
Diastole |
Isovolumetric ventricular relaxation and filling (.4 sec) |
|
|
Systole |
Isovolumetric ventricular contraction and ejection (.3 seconds)
As the pressure in the ventricles becomes greater than atria, av valves shut
There is an isovolumetric contraction of the ventricles
As the pressure increases and becomes greater than the arteries, the semilunar valves open and blood is ejected into circulation |
|
|
S1 |
Closure of av valves (the sound is the turbulence of blood rushing against heart wall) |
|
|
S1 |
Closure of av valves (the sound is the turbulence of blood rushing against heart wall) |
|
|
S2 |
At the end of systole , semilunar valves shutting |
|
|
Physiologic split |
Lub b dub
Because aortic valve has a bigger opening than pulmonic, the pulmonic valve opens sooner and closes later
Split s2- normal |
|
|
Valve closure and cardiac cycle |

|
|
|
S3 |
If ventricular wall compliance is decreases (not stretching like it should), structures in ventricular wall vibrate
Congestive heart failure or valvular regurgitation
May be normal <30 years
Lub dub dub |
|
|
S4 |
During atrial kick, If there is resistance to ventricular filling
De lub dub
Cardiac hypertrophy, disease or injury to ventricular wall |
|
|
Coronary vessels |
Coronary circulation
Part of systemic circulation, branch off aorta via coronary Ostia (to coronary arteries )
Coronary veins Return to the right atrium through ostium called the coronary sinus
|
|
|
Right coronary artey |
Conus- supplies upper r ventricle
Right marginal branch - transverses r ventricle to apex
Posterior descending- supplies smaller branches to both ventricles |
|
|
Right coronary artey |
Conus- supplies upper r ventricle
Right marginal branch - transverses r ventricle to apex
Posterior descending- supplies smaller branches to both ventricles
Posterior septum Posterior heart SA and AV node |
|
|
Left coronary artery |
Left anterior descending (Aka anterior interventricular artery aka the widow maker) - blood to portions of the left and right ventricles and much of the interventricular septum (bundle of his, electrical)
Circumflex artery- blood to left atrium and lateral wall of left ventricle |
|
|
Collateral arteries |
Anastomoses (connection) between two branches of the coronary that develop over time
Epicardium contains more collateral vessels than endocardium
Collateral circulation protects the heart |
|
|
Coronary capillaries |
3300 capillaries per sq mm
One capillary per muscle
Where exchange of oxygen and nutrients takes place
In ventricular hypertrophy, the capillary network doesn't expand--> same number of capillaries must perfuse a larger area--> decreases exchange of o2 and nutrients |
|
|
Cardiac action potentials |
Electrical impulse--> fibers shorten--> muscle contraction--> systole
After action potential--> fibers relax --> return to resting length --> diastole |
|
|
Qualities of heart muscle cells related to conduction |
Intercollated discs
Automaticity- can generate and discharge an electrical impulse
Excitability - can respond to an electrical impulse
Conductivity - ability to transfer an electrical impulse from one cell to another
WITHOUT STIMULATION FROM THE NERVOUS SYSTEM
|
|
|
Automatic inputs into the heart |

Back (Definition) |
|
|
Cardiac conduction |

Back (Definition) |
|
|
Cardiac conduction |

|
|
|
P wave |
Atrial contraction
Av node |
|
|
QRS complex |
Ventricular contraction (Purkinje fibers) |
|
|
T wave |
Repolarizarion phase
Electrical changes during relaxation phase of the ventricles |
|
|
T wave |
Repolarizarion phase |
|
|
Depolarization |
Activation , inside of the cell becomes less negative (positive ions entering the cell) |
|
|
T wave |
Repolarizarion phase |
|
|
Depolarization |
Activation , inside of the cell becomes less negative (positive ions entering the cell) |
|
|
Repolarization |
Deactivation |
|
|
T wave |
Repolarizarion phase |
|
|
Depolarization |
))Activation , inside of the cell becomes less negative (positive ions entering the cell)
Voltage sensitive Na channels open and and allow rapid influx of Na then rapidly close (phase 0-1)
K channels close then reopen slowly
Voltage-sensitive Ca channels have delayed at slower opening relative to Na (phase 2)
Ca responsible for contraction of cardiac muscle
Normal circumstances : < max Amt of Ca released which permits modulation of contractile strength |
|
|
Repolarization |
Deactivation
Return to resting membrane potential is delayed (phase 3)
Makes it impossible to fire a second action potential before the first is complete
Prevents summation and tetany |
|
|
Membrane potential |
Electrical (voltage) difference across the cell membrane
R/t changes in permeability of cell membranes (Na & K) |
|
|
Threshold |
Point at which cells selective permeability to Na & K is temporarily disrupted = depolarization
When the cell fires |
|
|
Hyperpolarization |
I.e. With hypokolemia (low potassium)
Cell becomes more and more negative |
|
|
Cardiac action potentials |

Back (Definition) |
|
|
Fast response |
Occurs in atrial and ventricular muscle cells and the purkinje conduction systems
Uses the fast sodium channels |
|
|
Fast response |
Occurs in atrial and ventricular muscle cells and the purkinje conduction systems
Uses the fast sodium channels
These don't normally initiate a cardiac impulse, if they do they are ectopic beats (generated outside of the designed electrical pattern of the heart) |
|
|
Slow response of the SA AND AV nodes |
Uses the slow calcium channels
Calcium has a role in generating cardiac impulse
Through the pacemaker nodes (SA and then AV) |
|
|
Absolute refractory period |
No stimuli can generate another action potential
Includes phases 0,1,2 and part of 3
The cell cannot depolarize again |
|
|
Absolute refractory period |
No stimuli can generate another action potential
Includes phases 0,1,2 and part of 3
The cell cannot depolarize again |
|
|
Relative refractory period |
Greater than normal stimulus response
Repolarization returns the membrane potential to below threshold, although not yet at the resting membrane potential
Begins when the transmembrane potential in phase 3 reaches the threshold potential level
Ends just before the terminal portion of phase 3 |
|
|
Absolute refractory period |
No stimuli can generate another action potential
From the end of qrs to apex of t wave
Includes phases 0,1,2 and part of 3
The cell cannot depolarize again
Part of repolarization |
|
|
Relative refractory period |
Greater than normal stimulus response
After apex of t wave
Repolarization returns the membrane potential to below threshold, although not yet at the resting membrane potential
Begins when the transmembrane potential in phase 3 reaches the threshold potential level
Ends just before the terminal portion of phase 3
Where arrhythmias happeb |
|
|
Supernormal excitatory period |
A weak stimulus can evoke a response
Extends from the terminal portion of phase 3 until the beginning of phase 4
Cardiac arrhythmia a develop
Resting membrane potential (RMP) |
|
|
Summation |
Prevented by repolarization
Increase in frequency of muscle stimulation that increases strength of contraction which can relate to tetany |
|
|
Tetany |
So many firings the heart can't fill, the heart doesn't have blood to pump out, cardiac output declines |
|
|
Heart rate |
Nl: 60-100
Sinus tachycardia > 100 Less filling time
Sinus bradycardia <60
Increase in heart rate increases oxygen consumption and if it's too fast it gets used up before it gets to the brain and can lead to confusion |
|
|
SNS stimulation |
Occurs when there is a decrease in pressure detected
Norepinephrine released (+ hr, + av contractility, peripheral vasoconstriction) |
|
|
PNS stimulation. |
Occurs when an increase in pressure is detected
Releases acetylcholine (- hr, - av contractility & conductivity) |
|
|
St elevation |
Doesn't return to the line during ecg, MI |
|
|
ST Depression |
Goes below st line, ischemia |
|
|
Echocardiogram |
Ultrasound
Creates a 3D picture of the heart using a transducer
Takes 30-90 minutes
Evaluates how well heart is moving, how well valves are working, size is the heart and its pumping chambers (ventricles), and ejection fraction |
|
|
Stress test |
Treadmill or bike hooked up to ekg
Performed until ischemia, angina or dyspnea occur (or until optimal heart rate is reached and nothing happens)
Should not be performed with significant aortic stenosis, untreated hypertension, CHF, unstable angina
Persantine for pts unable to exercise (dilates coronary arteries) |
|
|
Stress test |
No smoking or alcohol or caffeine prior
No large meals prior
No hot shower/bath after (Vaso vagal response) |
|
|
Stress test |
No smoking or alcohol or caffeine prior
No large meals prior
No hot shower/bath after (Vaso vagal response) |
|
|
Hotter monitoe |
24 hour ecg
Diary of when they feel arrhythmia / swipe card or on cell phone |
|
|
Stress test |
No smoking or alcohol or caffeine prior
No large meals prior
No hot shower/bath after (Vaso vagal response) |
|
|
Hotter monitoe |
24 hour ecg
Diary of when they feel arrhythmia / swipe card or on cell phone |
|
|
Coronary arteriography |
Gold standard
Cardiac Catheterization (coronary angiography) %%%%% Most precise means of measuring CAD
Also gives measures of left ventricular function (LVF) - left ventricular end diastolic pressure (LVEDP) -left ventricular end diastolic volume (LVEDV) -ejection fraction (EF)
For patients with severe angina, recurrent idiopathic chest pain, survivors of cardiac arrest
If coronary artery stenosis >70%--> flow limiting and of clinical significance |
|
|
Blood vessel layers |
Tunica adventitia- outer, connective tissue
Tunica media- middle, smooth muscle, maintains basal tone (^tone= vasoconstriction; Dec tone= vasodilation. )
Tunica intima- inner, smooth single layer of cells permits laminar blood flow
Controlled by SNS and local levels of O2 and CO2 |
|
|
Resistance and capacitance vessels |

|
|
|
Arterial blood pressure |

|
|
|
Cardiac output and blood pressure |

|
|
|
Stroke volume |
amount of blood ejected with ventricular contraction
70ml/beat nl |
|
|
Ejection fraction |
Percent volume of blood ejected with each ventricular contraction-- 55-75% of total ventricular volume
Ef = (sv/ edv) = 70ml/100 ml = 70% |
|
|
End- diastolic volume |
Total volume of blood in L ventricle at end of filling JUST PRIOR TO CONTRACTION
100ml
Function of : venous return to R atrium, - strength of atrial kick during ventricular filling -amount of blood pumped out of ventricle during last contraction |
|
|
Total peripheral resistance |
Aka systemic vascular resistance (svr) or peripheral vascular resistance (pvr)
Reflects the tone (degree of vasoconstriction) of resistance vessels (arteries and atrioles) as well as viscosity of the blood
Vasoconstriction = high bp Vasodilation = low bp |
|
|
Aortic impedence |
Loss of elasticity of aortic wall (stiffens)
Increase with aging and functioning of aortic valve
Aortic narrowing -- left ventricle must generate higher pressure to get blood through , left ventricular hypertrophy |
|
|
Starlings law |

Back (Definition) |
|
|
Preload |
Degree of myocardial muscle stretch
Before the right atrium, the blood that comes back to the Heart
Determined by blood volume
Increases preload , increased stretch, increased force of ventricular contraction (&stronger kick)
Related to degree of compliance of ventricular wall -ischemic heart muscle-decreased compliance -hypertrophied heart muscle- decreased compliance
Heart failure - increase in stretch without increase in force of ventricular contraction |
|
|
Preload |
Degree of myocardial muscle stretch
Before the right atrium, the blood that comes back to the Heart
Determined by blood volume
Increases preload , increased stretch, increased force of ventricular contraction (&stronger kick)
Related to degree of compliance of ventricular wall -ischemic heart muscle-decreased compliance -hypertrophied heart muscle- decreased compliance
Heart failure - increase in stretch without increase in force of ventricular contraction |
|
|
Afterload |
What the left ventricle must push against to get blood out
Determined by: Aortic and pulmonic impedence (aortic stenosis--- increased afterload)
Condition and tone of aorta and resistance offered by systemic and pulmonary arterioles (hypertension-- increases afterload)
Increased afterload = increased cardiac workload= increases o2 consumption |
|
|
Myocardial contractility |

|
|
|
ANS REGULATION OF BP |

|
|
|
Baroreceptors |

|
|
|
Chemoreceptors |

Back (Definition) |
|
|
Renin Angiotesin aldosterone |
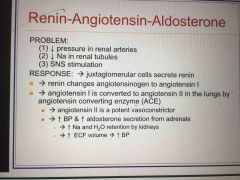
Back (Definition) |
|
|
Antidiuretic hormone (adh) |

|
|
|
Atrial stretch receptors and ANP |

The heart can't rest May be adverse reaction to anesthesia |
|
|
Brain natriuretic peptide (bnp) |

Discovered in brain of a pig
Less than 100 is normal |
|
|
Essential hypertension |

|
|
|
Risk factors for HTN |
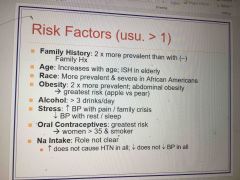
|
|
|
Manifestations of HTN |

Back (Definition) |
|
|
Classifications of blood pressure |

Back (Definition) |
|
|
Causes of hypertension by age |

Back (Definition) |
|
|
Hypertension in the elderly |

Back (Definition) |
|
|
Secondary hypertension |

|
|
|
Malignant hypertension |

|
|
|
Target organ disease |
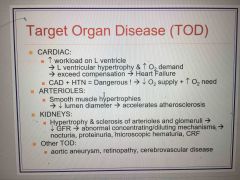
|
|
|
Tx lifestyle modifications |

Back (Definition) |

