![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
GI tract cellular components
|
Smooth muscle
Epithelium Neurons Bacteria Immune cells Blood vessels |
|
|
Basic processes of the GI tract:
|
Ingestion
Digestion, secretion and absorption Motility |
|
|
A few cell types accomplish all intestinal functions:
|
Muscle cells
Neurons Epithelial cells Immune cells Interstitial cells of Cajal, myofibroblasts, glia, stem cells |
|
|
GI Muscle cells
|
Contraction - Propulsion
Two types of muscle cells in the intestine A. Skeletal muscle - esophagus B. Smooth muscle – BVs, CM, LM and MM Small mononucleated cells form muscle layers Distinct from skeletal muscle - graded response to excitatory and inhibitory inputs (neural, chemical, mechanical) Tone: maintained contractile state of cell Active relaxation (VIP, NO) |
|
|
GI Neurons
|
Peripheral Nervous System
Somatic sensory Afferent - sensory signals from intestine Autonomic Nervous System Parasympathetic Sympathetic Enteric Nervous System autonomous within intestinal wall |
|
|
enteric nervous system
|
organized into ganglia.
Regulation of motility, blood flow and secretion - absorption. Complex, integrated sensory and motor pathways. But not pain. |
|
|
GI pain
|
Pain is a key symptom of intestinal pathology.
Contrast the normal with painful/inflamed states: Lack of sensation of intestinal activity Minimal knowledge of events Visceral/intestinal/gastric pain Severe, poorly localized Crampy, alternating OR unremitting |
|
|
GI Epithelial cells
|
An epithelial mucosa constitutes the physical barrier between the lumen and the body.
Functions include secretion, absorption, lubrication, protection. |
|
|
mucosa
|
The epithelial cell is the principal cell of the mucosa
Dynamic – constantly growing*, hence dividing and maturing; dying Functional - secretory/absorptive *Target in chemotherapy, radiation enteritis Intestinal mucosa - simple columnar epithelium |
|
|
GI immune cells
|
The largest component of the immune system
The lumen – the outside is inside Challenges include: Antigens, bacteria, physical damage Immune cells are resident in the mucosa Eosinophils, neutrophils, monocytes/macrophages, T cells, mast cells |
|
|
liver functions
|
Metabolism
Detoxification Glycogen storage Bile production |
|
|
Gall bladder
|
Muscular sack
Stores and concentrates bile Releases bile into duodenum in response to a meal. Cholecystokinin from enteroendocrine cells. |
|
|
Pancreas islets
|
Hormone production and secretion (endocrine pancreas)
|
|
|
pancreas acini
|
Digestive enzyme production and secretion (exocrine pancreas)
|
|
|
Motility
|
the appropriate and timely passage of ingested material along the intestinal tract
|
|
|
Sphincters create functional compartments
|
regulated via neuronal input and smooth muscle contraction
|
|
|
GI innervation
|
Intrinsic (enteric) innervation regulates function
Extrinsic innervation modulates, conveys information to the CNS |
|
|
Achalasia symptoms
|
– dysphagia, regurgitation, chest pain
Lack of esophageal peristalsis Incomplete relaxation of LES, LES hypertrophy Increased resting tone of LES |
|
|
LES
|
lower esophogeal sphincter
|
|
|
peristaltic reflex
|
oral-contraction
anal-relaxation |
|
|
layering of GI tract
|
longitudinal muscle
myenteric plexus circular muscle submucosal plexus mucosa |
|
|
Gastro-esophageal reflux disease
|
Exposure of esophagus to gastric juice (heart burn)
Transient(sudden) LES relaxations Loss of LES tone Impaired esophageal clearance of stomach contents Treatment: PPI, antacids, H2 receptor antagonists |
|
|
Regions of the stomach
|
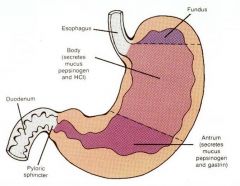
|
|
|
Gastroparesis
|
Delayed gastric emptying
Nausea, vomiting, bloating, early satiety, pain Idiopathic, diabetes vagus nerve is damaged and the muscles of the stomach and intestines do not work normally |
|
|
Mechanisms of gastroparesis
|
Autonomic (parasympathetic and enteric) neuropathy – impaired relaxation of pyloric sphincter
Antral hypomotility – interstitial cells of Cajal Gastric hypersensitivity- early satiety, pain and nausea |
|
|
stimuli for emesis
|
distention, irritation of GI tract
drugs, motion and intracranial pressure, strong noxious perceptions |
|
|
emesis risk for health
|
- aspiration(foreign materials - lungs), electrolyte imbalance
|
|
|
emesis process
|
Glottis closes
LES relaxes Reverse peristaltic waves Abdominal muscles contract |
|
|
achalasia etiology
|
is unknown but suspected to involve loss of inhibitory muscle motor neurons (NO and VIP)
Treatment – Heller myotomy(cut muscle), Botulinum toxin, dilation |
|
|
IBS
|
Characterized by chronic abdominal pain and altered bowel habits in the absence of any organic cause
3:1 female Pain relieved by defecation Duration of months Altered motility patterns Enhanced gastro-colic reflex Alternating symptoms |
|
|
Post-infectious IBS
|
Subset of IBS patients suffer severe gastroenteritis prior to symptom onset.
Walkerton, ON. Previous immune stimulation resets the balance of neural signalling in the gut |
|
|
Treatment of IBS
|
Dietary adjustment- fibre supplement
Serotonin signaling Very high placebo response – role of the CNS in regulating symptoms |
|
|
Mechanical Obstruction of the Intestine
|
Obstruction
Mechanical Developmental Inflammatory – eg stricture (IBD) Tumour Adhesions Inappropriate connection of adjacent intestinal segments (eg, splenic flexure of colon to mid-jejunum), or intestine-other organ (colon-bladder) |
|
|
Strangulation
|
Associated with herniation of the abdominal muscle
inguinal hernia Entrapment and constriction of the intestine causes obstruction, ischemia and occasionally gangrene |
|
|
Hirschprung’s disease
|
Non-propulsive region causing functional obstruction in infant
distended colon upstream of band of constriction, risk of toxicity Histological Diagnosis absence of enteric ganglia – no enteric neurons in constricted segment Surgical excision and anastomosis (different connection). Stem cells |
|
|
Difference between CD-UC
|
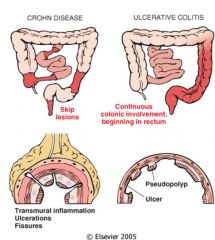
|
|
|
IBD
|
Crohn’s disease (CD) and ulcerative colitis (UC)
Pain, bleeding, diarrhea, fever Impaired growth, anemia, weight loss Cause is unknown Genetic susceptibility Possible environmental factors IBD likely arises from exposure of a genetically susceptible individual to an environmental trigger. prevelance increases far equator developed nations mostly |
|
|
CD location
|
anywhere from mouth to anus
ileum most common, Crohn’s colitis is possible typically terminal ileum |
|
|
CD characteristics
|
Skip lesions in ileum
Cobblestoning of normal mucosa with surrounding fissured, inflamed tissue Stricturing disease - surgical resection due to redundancy of ileum disease may recur |
|
|
CD nutrients
|
can lead to “short gut” syndrome.
Basic absorption of nutrients requires adequate small intestinal length (=area) B12 absorption unique to ileum |
|
|
CD immunology
|
CD4 IFN-y, TNF bad
CD4 IL10, TGFB good |

