![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
What are examples that cause blood destruction?
|
2HPT
・(Immune-mediated) Hemolytic Anemia ・Heinz body anemia ・(Zinc) Toxicosis ・(Hypo)phosphatemia ・(RBC) Parasites ・Thermal |
|
|
IMHA is often ___ to other disorders/events.
|
Secondary
|
|
|
1. IMHA is associated with __(3)__ in horses.
2. IMHA is associated with __(3)__ in cats. 3. IMHA is more common in ___. |
1. Clostridial infections, Penicillin, Neoplasia
2. Mycoplasma haemofelis, FeLV, Neoplasia 3. Dogs |
|
|
Highest incidence of IMHA in dogs is highest in (3 breeds)
|
Cocker spaniel (Poodles & Collies)
(Cocker-Poodle doo (chickens rounded by Collies)) |
|
Dx:
MCV: |
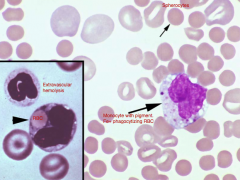
Dx: IMHA (spherocytes)
MCV: Normocytics (MCV normal in spherocytes) |
|
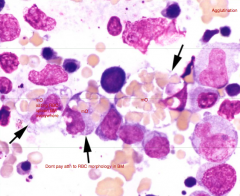
Anemia in animal was NON-REGENERATIVE so a BM aspirate was conducted.
Dx: What supports your answer? Why is it non-regenerative? |
Dx: IMHA (Polychromatophilic cells are being destroyed before going into circulation)
Support: Agglutination [TR] and mO engulfing RBC Why? Polychromatophilic cells are also being destroyed & not released. |
|
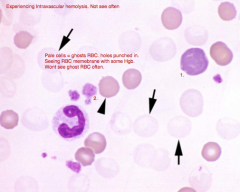
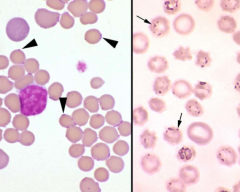
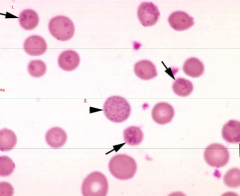
Identify the structures:
1. 2. Dx: |
1. Polychromatic cell
2. Platelets Dx: IMHA |
|
|
What are Ddx for SPHEROCYTOSIS?
|
・Previous mismatched blood transfusion
・Rattlesnake envenomation (→ echinocytes → spicules go away → spherocytosis) ・Bee stings (band 3 clustering) ・Heinz body anemia in horses ・Zinc toxicosis (→ △membrane Ag→ spherocytosis) TB HRZ |
|
|
1. If there is no observable agglutination BUT suspecting IMHA, we may use the ___ to confirm.
2. Agglutination is when ___ is the antibody. 3. True/False. When agglutination is present macroscopically, then no Coomb's test is necessary. |
1. Coomb's test (Direct Antiglobulin Test (DAT)
2. IgM 3. True (automatically an IMHA) |
|
|
What are some disadvantages of using Coomb's test?
|
Many false POSITIVES (Low sensitivity)
Many false NEGATIVES (Low specificity) ([L] of Ab on RBCs) |
|
|
How can we prevent false positives?
|
Wash RBC's 3x (Reads immune complexes/Ab attached to erythrocytes but NO destruction)
|
|
Is Coombs' test indicated?
Dx: |
No
IMHA |
|
|
What laboratory findings will be associated with IMHA?
|
Thrombocytopenia
Leukogram: inflammation +/- Azotemia (prerenal/renal (Hgb toxic to renal)) |
|
|
What other diseases can result with thrombocytopenia?
|
DIC (aPTT & PT prolonged)
|
|
|
1. RBC production is stimulated by...
2. Leukocyte production is stimulated by... 3. What other dz. is usu. in conjunction with IMHA? 4. Animals with IMHA usually die from ___. |
1. EPO
2. Cytokines 3. DIC 4. Thromboembolism (assoc. w/ DIC) |
|
|
What other disease is concurrently associated with IMHA?
|
DIC
|
|
|
In summary, IMHA is associated with what findings?
|
・Regenerative
・Spherocytosis ・+/- Agglutination (if IgM) ・nOilia + L-shift ・Thrombocytopenia |
|
|
What are Ddx for SPHEROCYTOSIS (BIHRT)?
|
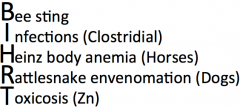
・Rattlesnake envenomation (Dogs) (→ spheroechinocytes → spicules go away → spherocytosis)
・Clostridial infections (Horses) ・Bee stings (band 3 clustering) ・Heinz body anemia (Horses) (membranes collapse (eccentrocyte)/band 3 clustering) ・Zinc toxicosis (→ band 3 clustering → spherocytosis) |
|
|
What is band 3?
|
A major erythrocyte membrane-spanning protein that is responsible for mediating the exchange of chloride (Cl-) for bicarbonate (HCO3-). When clustered, they provide the recognition site for Abs.
|
|
|
1. What is neonatal isoerythrolysis?
2. What other signs are associated with neonatal isoerythrolysis? |
1. Maternal Ab made against the neonates blood group Ab → RBC hemolysis.
2. Hemoglobinemia, Hemoglobinuria, Splenomegaly, Thrombocytopenia, DIC (BF of IMHA) |
|
|
1. Which erythrocyte parasites mechanically cause IV hemolysis?
2. How do the other erythrocyte parasites cause anemia? |
1. Theileria & Babesia
2. By immune-mediated mechanisms (Ab → parasite → complement fixation/phagocytosis → RBC destroyed) |
|
|
What erythrocyte parasite is the most COMMON and serious cause of severe anemia?
|
Mycoplasma haemofelis (T: blood (iatrogenic), arthropods, cat bites, vertically)
|
|
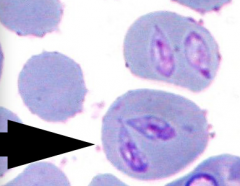
1. Identify the parasite.
2. If anemia is NON-REGENERATIVE, what tests are indicated? |
1. Parasite: Mycoplasma haemofelis (usu. Reg. anemia)
2. FeLV/FIV |
|
|
What factors predispose animals to Mycoplasma haemofelis?
|
Concurrent disease
Immunosuppression (severe) Splenectomy |
|
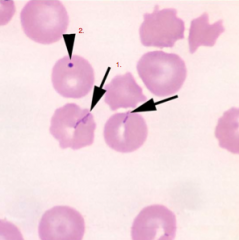
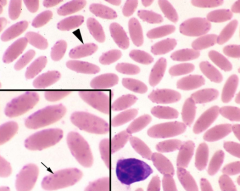
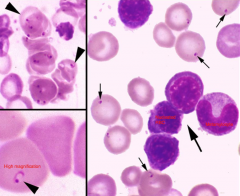
Identify the structures/parasites:
1. 2. What factors predispose animals to Mycoplasma haemocanis? |
1. Mycoplasma haemocanis (opportunist)
2. Howell's Jolly Body (nucleus remnant) Factors: Immunosupression (severe), Splenectomy |
|
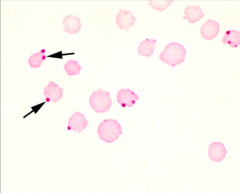
Identify the parasite:
1. What differentiates this parasites from other erythrocyte parasites? What is the common method of transmission? |
1. Mycoplasma wenyonii
Differentiation: M. wenyonii circulates freely or falls off RBC immediately T: Iatrogenic |
|
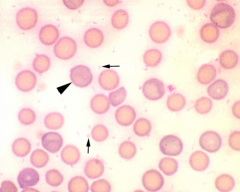
Identify the parasite/structure:
1. 2. Is #2 normal/abnormal in RUMINANTS ? Is #2 normal/abnormal in SMALL ANIMALS? |
1. Mycoplasma ovis (Big O)
2. Basophilic stippling Ruminants: Normal (common with regenerative anemia) Small Animal: Abnormal (associated with Pb poisoning) |
|
Identify the parasite/structure:
1. |
Mycoplasma haemolamae (opportunist)
|
|
|
What is the cause of:
Severe anemia in baby pigs Poor weight gain in adult pigs |
Mycoplasma haemosuis
|
|
What TICK-BORNE rickettsial infections (2) cause FATAL HEMOLYTIC ANEMIA (esp. older animals) by immune-mediated destruction?
|
Anaplasma marginale [picture]
Anaplasma centrale |
|
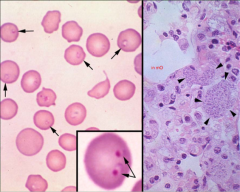
Identify the parasite/structures on this cow's blood film:
1. 2. 3. |
1. Polychromatic cell
2. Basophilic stippling 3. Anaplasma marginale (in large #'s) |
|
|
What TICK-BORNE erythrocyte parasite mechanically causes IV hemolysis (→ hemolytic anemia) and is fairly toxic esp. in cats?
|
Babesia
|
|
What disease can be mistaken for IMHA and can be identified by its TEAR-DROP shape?
|
Babesiosis
|
|
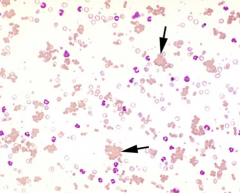
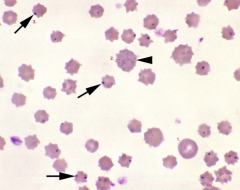
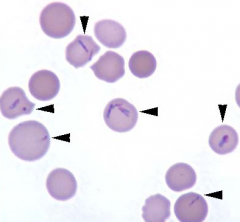
Identify the parasite/structure indicated by the small arrows/arrow-head in this blood film:
Small arrows/arrow-head: |
Small arrows/arrow-head: Babesia
|
|
1. What other erythrocyte parasite mechanically causes IV hemolysis → hemolytic anemia in ruminants (esp. in CATTLE)?
2. What stage of this organism is within RBCs? |
1. Theileriosis
2. Merozoite (piroplasm) |
|
|
FYI: Sickle cells occurs in vitro due to the presence of...
|
air (no significance)
|
|
An important emerging infectious protozoan in domestic cats that is transmitted by ticks and is almost ALWAYS FATAL.
|
Feline cytauxzoonosis
|
|
|
1. What are heinz bodies?
2. What animal is most susceptible to the anemia? 3. Name 3 diseases that this anemia occurs with in cats (DHL). |
1. Oxidatively denatured hemoglobin
2. ***Cats*** 3. DM, HyperTHYROidism, Lymphoma |
|

Dx the condition:
What stain is used to confirm the presence of these structures? |
Dx: Heinz Body Anemia
Stain: New Methylene Blue |
|
|
What is methemoglobinemia?
|
Abnormal hemoglobin in which the Fe of the unoxygenated hemoglobin is in the FerrIC (germaphobe) state rather than the ferrous state (ferric = unable to carry O2/CO2).
|
|
|
Some drugs & chemicals → heinz body anemia also cause ___.
|
methemoglobinemia (see in conjunction)
|
|
|
Name some PLANTS that may cause Heinz body formation:
|
・Onions, Garlic (Allium family)
・Cabbage, Kale, Rape (Brassica) ・***Wilted red maple leaves*** |
|
|
Name some DRUGS/CHEMICALS that may cause Heinz body formation:
|
・Acetaminophen (cats)
・Propylene glycol (NOT ETHYLENE; cat food) ・Zinc ・Cu Se deficiency ・Crude oil ・Moth balls (Naphthalene) |
|
|
What are 2 ways hemoglobin can be oxidized?
|
1. Hemichrome formation (→ aggregates of denatured Hgb)
2. Oxidative damage to sulfhydral groups (CATS more susceptible) |
|
|
Hemichromes complex with ___ resulting in ___ sites for auto-antibodies (cell removed by spleen). This may also lead to the formation of ___.
Name 2 items that may cause the formation of these heinz bodies. |
Band 3/Recognition/Spherocytes
2 causes: Zn toxicosis, Wilted red maple leaf toxicosis |
|
|
Name some PLANTS that may cause methemoglobinemia:
|
***Wilted red maple leaves***
|
|
|
Name some DRUGS/CHEMICALS that may cause methemoglobinemia:
|
・Acetaminophen (Cats)
・NitrITE poisioning (Cows; Nitrates → Nitrites (Toxic)) |
|
|
Name a CONGENITAL DEFICIENCY that may cause methemoglobinemia:
|
NADH-methemoglobin REDUCTASE (enzyme that converts methemoglobin to hemoglobin)
|
|

Pulled blood that appears chocolate brown. What is this diagnostic of?
|
Methemoglobinemia (→ ↑free O2 → ↑O species → Heinz body formation)
|
|
|
What metal accumulates in LIVER of SHEEP (most susceptible) and during stress → heinz body formation?
|
Copper (Cu toxicosis)
|
|
|
Heinz body in (animal) formation arises from ___.
Cats Sheep Horse Cattle |
・Acetaminophen
・Cu Toxicosis ・Wilted red maple leaves ・Nitrite poisoning |
|

Deficiency in the mineral ___ leads to HEMOLYSIS.
|
Phosphorus (hypophosphatemia; ATP is required for normal red blood cell membrane integrity)
|
|
|
Hypophosphatemia → ___ → ___
What are some causes of hypophosphatemia? |
↓ATP (req'ed for norm RBC membrane integrity)/hemolysis
Causes: Postparturient hemogobinuria (CATTLE; due to Ketones) DM & Enteral alimentation (CATS) |
|
|
How do ketones causes heinz body formation?
|
Oxidative damage to hemoglobin.
|
|
|
___ & ___ are 2 bacteria that can cause HEMOLYSIS.
|
Clostridium spp. (Lecinthinase → lysis)
Leptospira spp. (RARE) |
|
|
(Name of agent) IS TO (Disease) as:
Clostridium perfringins Type A IS TO Clostridium haemolyticum IS TO |
・"Yellow lamb disease" (LAMBS & CALVES = young)
・"Bacillary hemoglobinuria/Red water disease" → associated with liver fluke migration (CATTLE) |
|
|
Unlimited water access (cattle/calves (usu.)) → HEMOLYSIS. Why? What is this condition called? In what animals may this be more severe?
|
↓Osmolality of plasma → H20 moving into RBC.
Condition: Water intoxication More severe in: Fe deficiency anemic animals (CALVES) |
|
|
What INHERITED membrane defect is known to occur in Miniature Schnauzers & Alaskan Malamutes?
|
Hereditary stomatocytosis
|
|
|
What enzyme deficiencies contribute to hemolytic anemia?
|
・glucose-6-phosphate dehydrogenase (G6PD) (import. for NADPH)
・Pyruvate Kinase (PK) deficiency in dogs/cats (import. for glycolysis) ・Phosphofructokinase (PFK) deficiency (import. for glycolysis) ・Uroporphyrinogen III co-synthetase |
|
|
What breeds (DOGS) are more susceptible to Pyruvate Kinase (PK) deficiency?
Why does this deficiency lead to HEMOLYTIC ANEMIA? |
Basenji, Beagles, West Highland White Terrier, Cairn Terrier
MOA: Lack of ATP → abnormal RBC membrane integrity → DEATH by age 4 |
|
|
What breeds (CATS) are more susceptible to Pyruvate Kinase deficiency (PK)?
How is a deficiency in cats different from a deficiency in dogs? |
Abyssinian, Somali, DSH
Difference: Cats can live to old age. Dogs die by age 4. |
|
|
What breeds (DOGS) are more susceptible to Phosphofructokinase (PFK) deficiency?
|
English Springer Spaniel dogs (PCV= WRI but hemolytic crises when ALKALEMIC)
|
|
|
The deficiency of ___ → inability to synthesize hemoglobin (spec. Heme)
What does this lead to? |
Uroporphyrinogen III co-synthetase
Outcome: ↑UROporphyrin & COPROporphyrin (bones & teeth → fluorescence & photosensitivity) and ***↓RBC survival***. |
|
|
What do we see in PIGS & CATS with uroporphryinogen III co-sythetase
|
PIGS: No photosensitization
CATS: No anemia |
|
|
What are our options for a non-regenerative anemia/↓production of RBCs?
|
**EARLY** = Blood loss/Destruction
Late = Chronic Ehrlicia, Neoplasia, Toxin |
|
|
MCV = HIGH (macrocytosis)
Non-regenerative anemia In a cat these values suggest: |
FeLV (otherwise tends to be normocytic)
|
|
|
What 2 readings tend to be useless with a non-regenerative anemia?
What 2 diagnostic tools may we need to look at to find out what the issue is? |
・MCV (tends to be normocytic)
・RBC morphology (tends to be normal) ・Diagnostic tools: Biochemical profile, BM aspirate |
|
|
If anemia originates from RBC production then, what will we see in the diagnostic tests?
|
Hypoplasia (↓RBC production)
Aplasia (No RBC production) |
|
|
↓RBC (Hypoplasia)
Neutropenia Thrombocytopenia Non-regenerative anemia Values suggest: What type of anemia is this? |
Anemia originates from BM
Aplastic Anemia (General Marrow Suppression) |
|
|
What are Ddx for APLASTIC anemia (General Marrow Suppression)?
|
・Immune-mediated destruction (early; confirm w/ GC)
・Ehrlicia, FeLV (macrocytosis) ・Drugs & chemicals |
|
|
Name some DRUGS/CHEMICALS that cause Aplastic Anemia (General Marrow Suppression).
|
・Anti-neoplastic/Immunosuppressive drugs
・Toxins: solvent/household cleaning agents (Dogs/Ferrets) ・Estrogen: granulosa cell tumors, sertoli cell tumors, unspayed F ferrets (Dogs/Ferrets) |
|
|
How often do we see Erythroid Aplasia (Pure Red Cell Aplasia)?
What are the 2 main causes of Erythroid Aplasia? |
Occurrence: Rare
Causes: Immune-mediated destruction of RBC precursors (NO DRUGS/CHEMICALS) & FeLV |
|
|
What DRUGS/CHEMICALS cause Erythroid Aplasia?
|
NONE. Always think immune-mediated.
|
|
|
Non-regenerative anemia with Erythroid Hypoplasia can be ___ OR ___.
|
Intrinsic/Extrinsic
|
|
|
Name some INTRINSIC factors that contribute to Erythroid Hypoplasia in non-regenerative anemia.
|

・Myelodysplasia (ineffective production of the myeloid class of blood cells)
・Leukemia (type of cancer of the blood/BM) ・Immune-mediated destruction of erythroid precursors. LIM |
|
|
Name some EXTRINSIC factors that contribute to Erythroid Hypoplasia in non-regenerative anemia.
|
Chronic Renal disease
Inflammatory disease Endocrine disorders (hypothyroidism/adrenocorticism = ↓RBC prod.) ERI |
|
|
The most important EXTRINSIC factor that contributes to Anemia of Renal Disease is the insufficiency of ___.
|
EPO (anemia of renal disease)
|
|
|
What diagnostic assessment will help us diagnose an anemia of inflammatory disease?
|
↑storage Fe (inflammatory dz anemia (Regen.) may be superimposed over Fe deficiency anemia (non-Regen.))
|
|
|
What are the 2 Fe storage complexes?
What is the difference? What is hepicidin? |
Fe storage complexes: Hemosiderin & Ferritin
Diff.: Hemosiderin (insoluble) & Ferritin (soluble) Hepicidin: Hormone that regulates Fe hemostasis |
|
|
Overall what do we see with Anemia of Inflammatory Disease?
|
↑storage Fe → ↓Fe transport & functional pools (limit to EPO)
|

