![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
What is systemic inflammatory response syndrome (SIRS)?
|
2 or more of:
- fever - ↑ or ↓ WBC (leukocytosis or leukopenia) - ↑ heart rate (tachycardia) - ↑ (tachypnea) |
|
|
What is sepsis?
|
SIRS + infection
|
|
|
What is severe sepsis?
|
sepsis + hypotension
(corrected by administration of fluids) |
|
|
What is septic shock?
|
severe sepsis + persistent hypotension
(drugs to increase vascular tone required) |
|
|
What is multiorgan dysfunction syndrome (MODS)?
|
septic shock leading to
- clotting disorders or failure of renal, hepatic, cardiac, or cognitive function - accumulation of products of metabolism that cannot be cleared (eg: lactic acidosis) |
|
|
What are 3 complications that make the sepsis = SIRS + infection rule?
|
1. SIRS can occur in the absence of infection
eg: systemic autoimmunity, systemic allergic reactions, severe burn wounds or trauma 2. microorganisms in the blood do not always cause SIRS eg: some bacteria might enter the bloodstream following tooth brushing 3. sepsis can occur in the absence of viable microorganisms in the bloodstream ie: systemic presence of microbial products is sufficient |
|
|
While bacteria are the most common cause of sepsis, which 3 other things can cause sepsis as well?
|
viruses
fungi parasites |
|
|
What has been the recent trend in the incidence of Gram-negative sepsis and Gram-positive sepsis?
|
↓ cases of Gram-negative sepsis
↑ cases of Gram-positive sepsis due to the increased incidence in pneumonia and the use of intravascular devices |
|
|
Primary infections of which 4 regions account for more than 80% of all cases of sepsis?
|
Chest
Abdomen Genitounitary system Bloodstream |
|
|
What are 5 risk factors for sepsis?
|
1. Age: being > 40 y/o
2. Underlying diseases: neutropenia, solid tumors, leukemia, cirrhosis of the liver, diabetes, AIDS, serious chronic conditions such as COPD 3. Surgery or instrumentation: catheters 4. Prior drug therapy: immunosuppressive drugs, broad-spectrum antibiotics 5. Other: childbirth, abortion, trauma, burns, intestinal ulceration |
|
|
What does the structure of lipopolysaccharide (LPS) consist of?
|

- Repeating O antigen subunits
- Core polysaccharide - Lipid A (the toxic part) |
|
|
What are two important receptors that LPS binds to?
|
CD14
TLR4 (Toll-like receptor 4) |
|
|
What do the superantigens produced by some Gram-positive organisms, including pathogenic streptococci and staphylococci, do?
|
These superantigens are exotoxins that activate large populations of T cells in an antigen-independent manner, by binding with both MHC II on the antigen-presenting cell and certain beta chains of the T cell receptor. This leads to a cytokine storm resulting in sepsis. ("toxic shock syndrome")
|
|
|
Some pattern recognition receptors (PRRs) can be activated by endogenous molecular patterns called damage-associated molecular patterns (DAMPs) that are released during tissue damage (eg: severe burns, trauma). Explain.
|
During sepsis, bacteria release PAMPs including N-formyl peptides and bacterial DNA. Similarly, during trauma, mitochondria release DAMPs including N-formyl peptides and CpG-containing mitochondrial DNA. That's because bacteria evolved into mitochondria!
Like PAMPs, the DAMPs are recognized by neutrophils, and might cause a systemic inflammatory response similar to sepsis, but you can't call it sepsis because there are no infectious agents involved. |
|
|
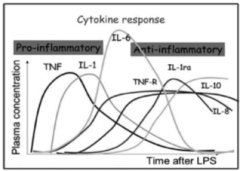
LPS leads to production of which 3 major sepsis mediators in the ensuing cytokine storm?
|
TNF-α: key player in inflammatory response
IL-1: induces fever IL-6: initiates the acute phase response |
|
|
Draw the relationship of the three main sepsis mediators following LPS injection in mice, and the associated symptoms.
|

|
|
|
Describe 3 effects the pro-inflammatory cytokine storm has on vascular endothelium.
|
1. Systemic increase in vascular diameter, leading to vasodilation and drop in blood pressure (partly due to induction of NO in endothelial cells)
2. increase in vascular permeability leading to vascular leak and loss of plasma volume 3. increase in expression of adhesion molecules, which bind to the surface of phagocytes and now can enter tissues |
|
|
Compare and contrast local infection and systemic infection (sepsis) of Gram negative bacteria
|
Macrophages activated to secrete TNF-α in the tissue
-> Incr'd release of plasma proteins into tissue, phagocyte and lymphocyte migration into tissue, and platelet adhesion to blood vessel wall -> Phagocytosis of bacteria, local vessel occlusion, plasma and cells drain to local lymph node -> Removal of infection; adaptive immunity Macrophages activated in the liver and spleen secrete TNF-α in the bloodstream -> Systemic edema causing hypovolemia (causing collapse of vessels), hypoproteinemia, and neutropenia, followed by neutrophilia -> Disseminated intravascular coagulation leading to wasting and multiple organ failure -> Death |
|
|
What is the kinin-kallikrein cascade activated by, and what are its effects?
|
Activated by: endothelial injury
Effects: drop in blood pressure Kallikrein is activated to generate kinins such as bradykinin, which lowers BP |
|
|
What is the complement cascade activated by, and what are its effects?
|
Activated by: microbes (eg: alternative pathway activation by LPS)
Effects: C5a causes chemotaxis, mast cell activation, production of histamine, vasodilation |
|
|
What is the coagulation cascade activated by and what are its effects?
|
Activated by: endothelial injury
Effects: thrombin/platelet clots causing DIC (disseminated intravascular coagulation), preventing blood flow and O2 delivery to vital organs. Consumption of clotting factors and platelets leads to bleeding in skin and mucous membranes Activation of Hageman factor (Factor XII) leads to activation of thrombin and formation of fibrin strands. |
|
|
What is the fibrinolysis cascade activated by, and what are its effects?
|
Activated by: endothelial injury
Effects: clot resolution, plasmin formation, and fibrin degradation, but this pathway is inhibited during sepsis via the coagulation and complement pathways, therefore is insufficient to suppress DIC |
|
|
How do the 4 plasma protein cascades of interest in sepsis interact?
|

|
|
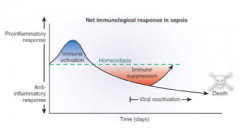
How are late stages of sepsis associated with immune suppression?
|
Because of homeostasis, waves of pro-inflammatory cytokines (TNF-α, IL-1, IL-6) are followed by anti-inflammatory cytokines (IL-10) and antagonists of pro-inflammatory cytokines (TNF-R, IL-1ra) that take over and cause immune suppression or paralysis.
This compensatory anti-inflammatory response syndrome (CARS) creates risk for reactivation of viruses and secondary infection. |
|
|
What are 4 broad clinical manifestations of sepsis?
|
1. Non-specific symptoms: fever, chills, fatigue, malaise, anxiety, confusion, increased heart rate, increased respiration
2. Multi-organ dysfunction 3. Virus reactivation (CMV, HSV) and secondary infection (Staphylococcus aureus, Clostridium difficile) 4. Death: in 30% of sepsis cases |
|
|
Describe the lungs in severe sepsis and septic shock
|
early fall in arterial PO2, acute respiratory distress syndrome (ARDS - capillary leakage into alveoli), tachypnea (rapid breathing), hyperpnea (increased depth of breathing)
|
|
|
Describe the kidneys in severe sepsis and septic shock
|
oliguria (low urine output), anuria (lack of urine output), azotemia (increased nitrogen-containing waste products in blood), proteinuria (protein in urine)
|
|
|
Describe the liver in severe sepsis and septic shock
|
elevated serum bilirubin, alkaline phosphatase, jaundice
|
|
|
Describe the digestive tract in severe sepsis and septic shock
|
nausea, vomiting, diarrhea, hemorrhage and bleeding
|
|
|
Describe the heart in severe sepsis and septic shock
|
cardiac output initially normal or elevated but heart failure may ensue
|
|
|
Describe the skin in severe sepsis and septic shock
|
initially warm or flushed (warm shock), but when cardiac output falls, peripheral vasodilation may be replaced by vasoconstriction in an attempt to redirect blood to vital organs, leading to pale and cold skin (cold shock), and blue/purple hands and feet
|
|
|
Describe the brain in severe sepsis and septic shock
|
confusion, delirium, stupor, coma -- even for patients that survive sepsis, the long-term effects on cognitive functions can be substantial
|
|
|
Describe systemic effects in severe sepsis and septic shock
|
lactic acidosis (due to lack of O2), generalized edema, bleeding tendency in the skin and mucous membranes (due to consumption of clotting factors and platelets during DIC), high stress hormones
|
|
|
What is the 1st of 3 priorities in treatment of sepsis?
|
Immediate stabilization of the patient
- protection of airway (intubation, mechanical ventilation) - blood pressure and tissue perfusion (fluids, vasopressors) - cardiac output - kidney function (dialysis) |
|
|
What is the 2nd of 3 priorities in treatment of sepsis?
|
Clearing of microorganisms from blood
- appropriate antimicrobials |
|
|
What is the 3rd of 3 priorities in treatment of sepsis?
|
Removal of the original focus of infection
- drain exudate - remove foreign body - remove infected organ - debride or amputate gangrenous tissue |
|
|
What are 4 other strategies that have been tried for sepsis treatment with limited success?
|
1. Inhibit LPS
2. Inhibit TNF or other cytokines 3. Inhibit inflammation (NSAIDs, corticosteroids) 4. Inhibit coagulation (activated protein C) |

