![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
_________; -occurs in the ileum near the ileocecal valve -result of failed involution of vitelline duct -mucosal lining contains ectopic pancreatic/gastric tissue
What do complications arise d/t? |

Meckel Diverticulum
ectopic gastric tissue--> secretes acid---> ulceration, bleeding, perforation |
|
|
_________; -MC in males -Inc in pts w/ Turners syndrome & Trisomy 18 -genetic predisposition -deficiency in nitric oxide synthase
What does this deficiency cause? |
Congenital hypertrophic pyloric stenosis
*NO necessary to inhibit sm muscle contraction is absent in pyloric muscularis propria--> uninhibited muscular contraction--> hypertrophy of pyloric sphincter |
|
|
How do pts w/ congenital hypertrophic pyloric stenosis present? |
at 3-6 wks w/ projectile NONBILARY vomiting & firm (1-2 cm) upper abdominal mass (= hypertrophied sm muscle)
*usually need abdominal surgery w/i first 6 months of life |
|
|
__________; -MC in males -present in 10% of Down Syndrome cases -genetic predisposition -Inactivation mutations in RET gene -defective migration of neural crest cells
What does this defect cause? |
Hirschsprung Disease (Congenital Anganglionic Megacolon)
segment of distal bowel & rectum lacking ganglion cells----> absent peristalsis in aganglionic segment--> functional obstruction--> dilation of proximal colon (= megacolon) |
|
|
How do pts w/ Hirschsprung disease present?
Dx? |
Present w/ failure to pass meconium, constipation/obstruction w/ abdominal distent, & BILIOUS vomiting (^ ALL d/t functional obstruction)
Dx confirmed by absence of ganglion cells on rectal biopsy |
|

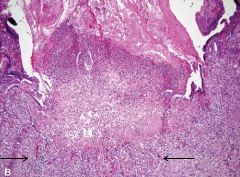
If a pt w/ Hirschsprung disease does not undergo surgical removal of the obstruction (arrow), what complications may arise? |
enterocolitis fluid & electrolyte disturbances perforation---> peritonitis
(gross img of megacolon on other side) |
|
|
_________ is characterized by the triad of: 1. Incr. Lower Esophageal Sphincter (LES) tone 2. Incomplete LES relaxation 3. Aperistalsis of the esophagus
What symptoms does this produce? |
Achalasia * continuous peristalsis prevents sphincter relaxation & food passage
sx: dysphagia for solids & liquids difficulty belching chest pain
(mild inc risk of malignancy) |
|
|
There are 2 types of achalasia. Describe Primary Achalasia |
degeneration of myenteric ganglion cells in the esophagus--> degenerative changes in the extraesophageal or dorsal motor nuclei of vagus nerves--> prevention of parasympathetic relaxation
-causes unknown |
|
|
Describe Secondary Achalasia |
d/t: chagas disease (Trypanosoma cruzi infection) Diabetic autonomic neuropathy Infiltrative disorders (sarcoidosis, amyloidosis) Lesions of the dorsal motor nuclei of vagus nerve (polio) Immune-mediated destruction of ganglion cells (after HSV, etc) |
|
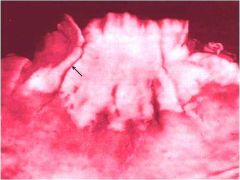
Img of longitudinal/ linear lacerations (arrow) involving the GE jxn. What disorder causes superficial (mucosal) GE & lower esophageal tears? |
Mallory-Weiss Syndrome
*associated w/ vomiting secondary to alcohol intoxication (most Gastroesophageal (GE) tears d.t vomit, trauma, & medical instrumentation)
*tears results in upper GI bleed & hematemesis
-no surgical intervention required (tears are superficial) |
|
|
________________ -causes deeper (transmural) esophageal tears -assoc. w/ excessive food & alcohol intake & bulimia -requires IMMEDIATE surgical intervention--> 25% mortality |
Boerrhaave syndrome
*more severe than Mallory-Weiss d/t deeper lacerations |
|
|
Clinical manifestations of esophagitis |
dysphagia odynophagia (painful swallowing) hemorrhage stricture perforation |
|
|
Chemical esophagitis is commonly seen in; -children after accidental ingestion of household cleaning products -adults after attempted suicide -"pill-induced esophagitis" (pill stuck--> erodes)
What are some responsible agents? How does it present morphologically? |
corrosive agents; lye (strong alkali), used in suicide attempt) sulfuric acid, HCL (strong acids)
morphology varies w/ conc/severity of agent- acute inflammation & granulation tissue--> fibrosis (strictures) & ulceration--> extensive necrosis (esp in lye intake)--> perforation |
|
|
Infectious esophagitis is MC seen in immunosuppressed individuals
What opportunistic agents are involved? |
Herpes Simplex Virus (HSV) Cytomegalovirus (CMV) Candida
*all of which can lead to inflammation, ulceration, & necrosis |
|
|
HSV responsible for infectious esophagitis, is likely to produce what distinct morphological characteristics seen? |
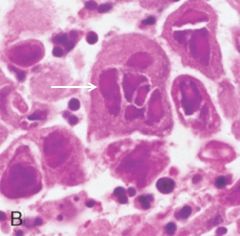
multinucleated (giant) squamous cells w/ viral nuclear inclusions (arrow) & intracellular molding |
|
|
What gross changes would HSV cause? |

multiple overlapping ulcers in the distal esophagus |
|
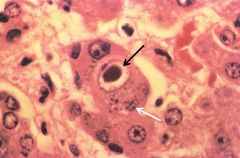
What agent? Distinct morphological characteristics? |
CMV esophagitis - enlarged cells w/ basophilic staining intranuclear inclusions (black arrow) & basophilic cytoplasmic inclusions (white arrow) |
|
What agent? Distinct characteristics? |
Candida esophagitis - multiple raised white psuedomembranes overlying intact squamous epithelium (arrow) |
|
|
Reflux esophagitis (GERD) if caused by reflux of gastric contents into lower esophagus. What are the predisposing factors? |
dec LES tone d/t; gastric distention, hiatial hernia alcohol, tobacco, CNS depressants
inc intra-abdominal pressure d/t; obesity (MC cause!), pregnancy coughing, straining, bending |
|
|
GERD is MC in individuals > 40
What are the sxs & complications? |
sxs: pyrosis (heartburn) regurgitation of sour-tasting gastric contents dysphagia
complications: ulcerations w/ hematemesis stricture formation barret esophagus |
|
|
How does reflux esophagitis (GERD) present morphologically? |

-scattered intraepithelial eosinophils (arrow) -basal zone hyperplasia -mucosal ulcers (if severe) |
|
|
_______ is a complication of chronic GERD characterized by intestinal metaplasia w/i the esophageal mucosa
*associated w/ an Inc risk of esophageal adenocarcinoma whether or not dysplasia is present |
Barrett Esophagus
Biopsy reveals presence of mutations shared w/ esophageal adenocarcinoma
^ # of carcinogenic mutations Inc when dysplasia present |
|
|
What is the presence of dysplasia associated w/ in Barretts esophagus? |
prolonged symptoms longer segment involved Inc age & caucasian |
|
|
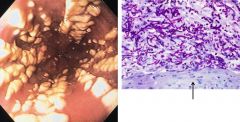
Barrett Esophagus is dx by endoscopy w/ biopsy. What do they show? |
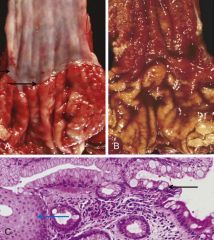
(L = normal smooth white esophageal mucosa & GE jxn (= arrows)) R endoscopy = GE jxn replaced by red velvety barrett mucosa, GE jxn not well demarcated |
|
What morphologic changes occur in Barret esophagus?
(bottom img) |
intestinal metaplasia--> change from normal squamous epithelium (L side, blue arrow) to columnar epithelium containing goblet cells (R side, black arrow)
*presence of goblet cells = key dx factor!!!
(goblet cells normally only present in intestines) |
|
|
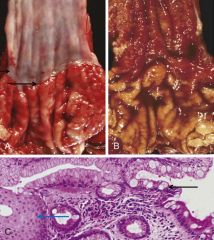
What is the transition from intestinal metaplasia to adenocarcinoma in Barretts esophagus? |
(black arrow) transition btwn intestinal metaplasia---> low grade dysplasia- w. nuclear stratification & hyperchromasia-> high grade dysplasia - w. nuclear enlargement & hyperchromasia & cribiforming (yellow arrow= back to back gland formation)--> adenocarcinoma |
|
|
Most esophageal adenocarcinomas arise from Barret esophagus & in Male pts *most are d.t inactivation of p16 (CDKN2A) (tumor suppressor)
What are the additional risk factors? |
obesity (inc likelihood of GERD) tobacco use low fresh fruit & veg diet Dec rate of Helicobacter pylori infection (atrophy of mucosa--> dec risk of esophagitis) |
|
|
Sxs of Adenocarcinoma include; odynophagia, dysphagia weight loss hematemesis chest pain * overall 5 yr survival < 25%
What are the morphologic changes? |
*occurs distal 3rd of esophagus--> invades to gastric cardia -hyperchromatic neoplastic cells form glands w/ mucin production (yellow arrow) |
|
|
Squamous Cell carcinoma MC occurs in rural/underdeveloped areas, in male adults > 45
What are the risk factors? |
alcohol & tobacco use*** (#1 cause) caustic esophageal injury achalasia diets deficient in fruits/vegs radiation |
|
|
Squamous cell carcinoma of the esophagus may occur d/t overexpression of cyclin D1, loss of function E-cadherin mutation*, HPV infection, or _________ |
Mutagenic chemicals: acetaldehyde polycyclic aromatic hydrocarbons (charcoal) nitrosamines fungal-derived complounds |
|

Squamous cell carcinoma occurs in the middle 3rd of the esophagus presents as ulcer w/ stricture (50% of time- img). What sxs does it produce? |
dysphagia, odynophagia (obstruction) (^pts often switch to liquid diet) cachexia LN metastases (common & poor prognosis) 5 yr survival < 20% |
|
|
How does Squamous cell carcinoma present morphologically? |
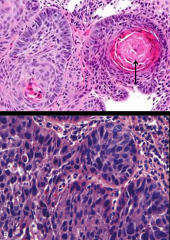
moderate w/ dysplasia (bottom) to well differentiated squamous cells (top) w/ keratin pearl (arrow) formation |
|
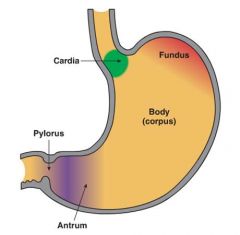
There are 4 regions of the stomach, which cell types does each contain? |
Fundus & Body- chief cells- secrete pepsinogen parietal cells- secrete HCL
Antrum- G cells- secrete gastrin |
|
|
_________ involves inflammation of gastric mucosa & neutrophils are present |
Acute gastritis |
|
|
_________ involved gastric injury, & inflammatory cells are NOT present |
Gastropathy |
|
|
Gastric acid & peptic enzyme are normally present in the stomach & do not cause gastric damage d.t protective factors. What may lead to damage? |
Inc gastric injury d/t; H. pyolori NSAID, alcohol, tobacco gastric hyperacidity duodenal-gastric reflux or Dec defenses d/t: ischemia shock NSAID |
|
|
Both gastropathy & mild acute gastritis lead to edema, vascular congestion, foveolar cell hyperplasia, epigastric pain, & N/V.
Gastritis may become more severe as....... |
Acute erosive hemorrhagic gastritis
characterized by; erosions & hemorrhage pronounced mucosal neutrophilic infiltrate hematemesis melena (tar black stool d.t upper GI bleed) |
|
|
Stress-related mucosal disease occurs d.t; severe trauma extensive burns major surgery serious medical conditions
What are the diff types of ulcers it can cause? |
stress ulcer- anywhere in stomach, seen w shock, sepsis, & severe trauma
curling ulcer- in proximal duodenum, seen w burns & trauma
cushing ulcer- in stomach, duodenum, & esophagus, seen w CNS trauma or strokes |
|
|
Pathogenesis of Stress-related mucosal disease |
*MC d.t mucosal ischemia d.t systemic hypotension or splanchnic vasoconstriction or hypersecretion of gastric acid d.t CNS trauma-> stimulation of vagal nuclei--> inc gastric acid or systemic acidosis--> dec mucosal pH |
|
|
Stress-related mucosal disease results in mucosal injuries ranging from erosions to ulcers, often w hemorrhage in the mucosa & submucosa (mucosa can heal completely w/i few days, may require blood transfusion of hemorrhage severe)
How do stress ulcers present morphologically? |
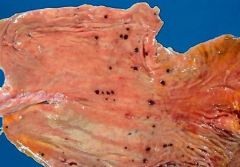
stomach (gross photo) w multiple small (< 1 cm) round dark brown to black ulcers (color d.t acid digestion of extravasated blood) |
|
|
Chronic gastritis is d/t chronic inflammation of gastric mucosa, pts present w;
upper abdominal pain Nausea, occasional vomiting (less severe, more persistent sxs than acute gastritis)
What are the MC causes? |
#1 = Helicobacter pylori gastritis #2 = automimmune gastritis
(chronic bile reflux, mechanical injury, & systemic disease (crohns, amyloidosis) are much less common) |
|
|
H. pylori (spiral bacilli) infections are mc in;
-individuals > 60 yrs in US -children (birth) outside the US, rural areas -low socioeconomic status, crowded households -african american or mexican american
How is it transmitted? |
fecal-oral route |
|
|
H. pylori infection usually starts as antral gastritis (initial inc in acid & risk for ulcers) & progresses to involve the ________ & _______ and become multifocal atrophic gastritis
What is multifocal atrophic gastritis assoc w? |
gastric body & fundus
assoc w dec parietal cell mass & dec acid secretion & intestinal metaplasia & inc risk of gastric adenocarcinoma (but dec risk of esophageal adenocarcinoma) |
|
|
H. pylori virulence is via; flagella urease (lowers pH) adhesins CagA (toxins)
Which of these factors is strongly assoc w risk of adenocarcinoma? |
CagA
&& genetic polymorphisms that INCREASE expression of TNF, IL-1B or DECREASE IL-10 are also associated w/ an inc risk of gastric CA |
|
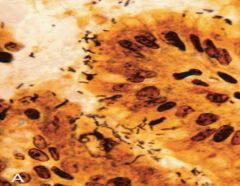
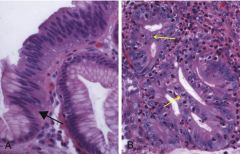
Spiral-shaped H. pylori are abundant in the ______________ (seen in this Warthin-Starry silver stain) |
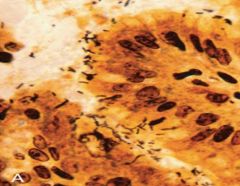
mucus overlying epithelial cells on the antrum surface & neck
*if extend to body & fundy--> patchy mucosal atrophy |
|
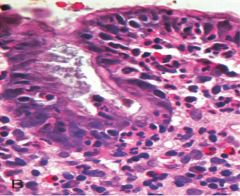
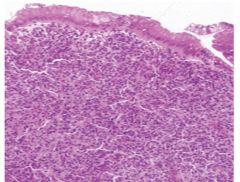
What H. pylori morphological features can be seen in this image? |
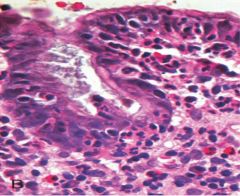
intraepithelial & lamina propria neutrophils
*plasma cells, lymphocytes, & macrophages may also be present |
|

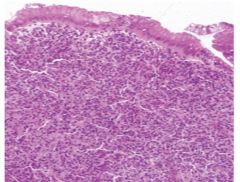
The presence of ____________ & ___________ are characteristic of H. pylori gastritis |

lymphoid follicles w/ germinal centers (yellow arrows = MALT*) & subepithelial plasma cells w/i lamina propria |
|
|
How is H. Pylori gastritis dx? |
Urea breath test: baseline 13CO2 is obtained pt ingests 13C-urea new breath sample analyzed for 13CO2--> Inc in 13CO2 = + for H. pylori
(serologic Ab & stool Ag tests, & gastric bx may also be used) |
|
|
Unlike H. pylori gastritis, Autoimmune gastritis (2nd MC cause of chronic gastritis, only 10%) usually spares the ___________ & is assoc w hypergastrinemia.
Describe the pathogenesis |
spares the antrum (involves the body & fundus)
pathogenesis: Autoreactive CD4+T against parietal cells--> destroy gastric glands--> secondary loss of chief cells--> --->---> eventual mucosal atrophy w/ intestinal metaplasia |
|
|
Pts are usually dx around age 60 & progress to gastric atrophy w/i 2-3 decades. Abs against parietal components are present early on & used for dx.
What parietal components are targeted? How does this manifest clinically? |
abs against H+K+ATPase & intrinsic factor
clinical: Achlorhydria B12 deficiency (d/t lack of intrinsic factor) ^ leads to megaloblastic/pernicious anemia, peripheral neuropathy, subacute combined cord degeneration, & cerebral dysfunction |
|
|
How does chief cell loss & mucosal atrophy w/ intestinal metaplasia present clinically? |
chief cell loss--> decr serum pepsinogen I
mucosal atrophy w/ intestinal atrophy--> inc risk of gastric adenocarcinoma |
|
|
How does Autoimmune gastritis present morphologically?
(primary mucosal atrophy occurs in the body & fundus w/ G cell hyperplasia in the antrum) |
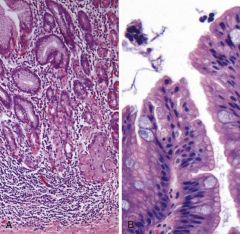
L= mononuclear infiltrates w/i lamina propria & glandular atrophy w/ loss of rugal folds R= intestinal metaplasia= goblet cells w/i foveolar epithelium |
|
|
Peptic ulcer disease (PUD) refers to chronic mucosal ulceration of the proximal duodenum or stomach (usually gastric antrum). What are the common causes? |
#1= H. pylori (incidence dec in developed countries)(chronic gastritis*) NSAIDs (inc cause in pts > 60) Cigarette smoking |
|
|
PUD results from an imbalance btwn defense mechanisms & damage.
What are the defense mechanisms & damaging factors? |
defense mechanisms: mucus secretion mucosal blood flow prostaglandins
damage: H. pylori Inc HCL production Immune-mediate injury toxic chemicals |
|
|
How does PUD present clinically? |
N/V bloating, bleching weight loss epigastric burning/aching pain pain worsens at night & btwn meals pain relieved by alkali & food (buffers)
|
|
|
What are some serious complications of PUD? |
bleeding *MC (1/4 ulcer deaths) perforation (2/3rds of ulcer deaths) obstruction (causes extreme pain & vomiting) |
|

PUD ulcers are solitary, oval "punched-out" & level w/ surrounding mucosa. What histologic changes does PUD cause? |
ulcer bed shows fibrinopurulent exudate w necrotic, fibrous, & granulation (arrows) tissue
(fibrous scars usually beneath granulation) |
|
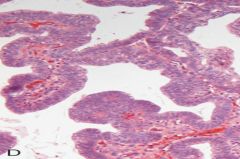
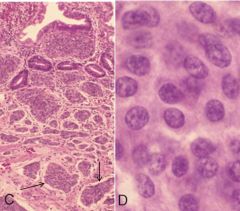
What does this img show? What are the key features? |
Gastric Adenoma (adenomatous polyp)
-dysplastic columnar epithelium w/ nuclear enlargement, hyperchromasia, epithelial crowding & psuedostratification w/ nuclei in upper epithelium |
|
|
Gastric adenoma; -gastric antrum polyp w/ columnar dysplasia -male 50-60 yrs -occurs in pts w chronic gastritis w/ atrophy & intestinal metaplasia -pre-malignant lesion
What is the risk of adenocarcinoma related to? |
risk of adenocarcinoma relative to size, esp > 2 cm |
|
|
Most gastric adenoma polyps are solitary, however there may be multiple in pts w ________ |
multiple in pts w Familial Adenomatous Polyposis |
|
|
90% of all gastric cancers are Gastric Adenocarcinoma. What are the two types?
Tumor stage is the best prognostic indicator w/ 5 yr survival < 30% (bad) |
Intestinal-type Diffuse-type |
|
|
H. pylori, cigarette smoking, dietary factors (smoked meats & nitrite preservatives) inc risk of both types.
What genetic factors are related to each? |
Diffuse-type: loss of E-cadherin
Intestinal-type: loss of function APC mutation & gain of function beta-catenin proto-oncogene mutation |
|
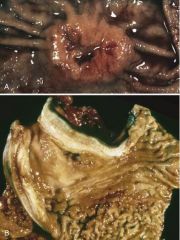
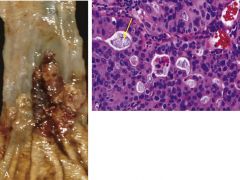
Which type is each img? What are the key features? |
top= Intestinal-type--> elevated borders w/ central ulceration, exophytic or ulcerated tumor mass
bottom= Diffuse-type--> wall thickened & rigid, rugal folds lost, "leather bottle" linitis plastica appearance, no mass |
|
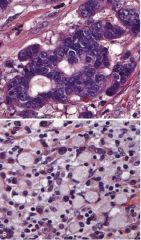
Which type is each img? What are the key features? |
top= Intestinal-type--> hyperchromatic columnar cells forming glands that are infiltrating through desmoplastic stroma
bottom= Diffuse-type--> signet-ring cells w/ large cytoplasmic mucin vacuoles & peripherally displaced crescent shaped nuclei, infiltrating stroma (no glands) |
|
|
Which type? MC in high-risk areas (Japan) Dec incidence in US & other low risk places develops from flat dysplasia & adenomas MC in males |
intestinal-type |
|
|
Which type? Incidence similar in all places no precursor id'd equal in male & females |
Diffuse-type |
|
MC type of gastric lymphoma?
d/t H. pylori inflammation---> _______ activation |
MALT lymphoma (lymphoma infiltrates mucosa & obliterates gastric glands)
NF-kB activation---> MALT lymphoma |
|
|
(antibiotic) eradication of H. pylori will lead to MALT lymphoma remission UNLESS....... |
unless NF-kB activation is d/t one of 3 different translocations |
|
|
_______________ are assoc w; endocrine cell hyperplasia (hormone produce) autoimmune chronic atrophic gastritis MEN-I Zollinger-Ellison Syndrome (gastrin production) Carcinoid syndrome (serotonin production)
*peak incidence in 60's (age) |
Gastric carcinoid tumors |
|
|
How do gastric carcinoid tumors appear grossly? |

yellow or tan, very firm, & well circumscribed |
|
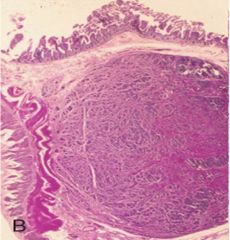
Gastric carcinoid tumors may arise in the mucosa or submucosa (img). How do they appear histologically? |
(img = mucosa) -tumors nested into dense fibrous tissue or w/i lymphatic channels (arrows), glands, sheets, or trabeculae -oval uniform cells w/ scant cytoplasm & minimal anaplasia |
|
|
Immunohistochemical stains of gastric carcinoid tumors are usually positive for........ |
synaptophysin & chromogranin A |
|
|
The most important prognostic factor for gastric carcinoid tumors is location. What are the various locations & outcomes? |
foregut tumor- rarely metastasize, cured by resection
midgut tumor- multiple & aggressive*
hindgut tumor (rectum, colon, appendix)- usually found incidentally, appendiceal always benign, rectal may present w pain & weight loss, no metastasize |
|
|
A carcinoid tumor arising from which of the following locations is most likely to metastatize?
a. jejunum b. rectum c. appendix d. stomach
|
jejunum (midgut) |

