![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
What is the action of insulin on the liver?
Key words: triglyceridogenesis, Glycogenolysis, glycogenesis, lipolysis, LDL formations, ketogenesis |
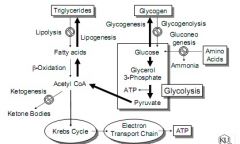
INHIBIT: glycogenolysis, lipolysis, ketogenesis
PROMOTES: glycogenesis, triglyceridogenesis & LDL formation |
|
|
What is the action of insulin on skeletal muscle?
|
PROMOTES protein synthesis:
-Increases amino acid transport -Increases ribosomal protein synthesis INCREASES glycogenesis: -Increases myocyte glucose uptake -Inhibits glycogenolysis |
|
|
What is the action of insulin on Adipose Tissue?
|
INCREASE TG storage
-Lipoprotein lipase is induced and activated by insulin to mobilize TGs from lipoproteins(which reside in blood) -Intracellular (adipocyte) lipase is inhibited -The net effect is to increase fat storage |
|
|
|
|
|
What are the differences b/w human, pork, and beef insulins in terms of the number of aa differences and relative immunogenic potency?
|
Beef insulin differs from human insulin @ 3 aa positions, whereas pork differs only by one.
BEEF > PORK > HUMAN |
|
|
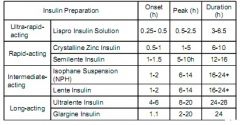
Note the connection b/w solubility and onset-duration following SubQ administration for Isophane NPH insulin. How does the presenceof protamine in the NPH(neutral prtamine Hagedorn) formulation dealy onset and prolong the action of insulin?
|
Form a depot that slowly releases into the blood. Protamine is arginine rich peptide. Enzymes digest protamine to get to insulin.
|
|
|
What is the mechanism of action of Crystalline Zinc Insulin Formulation?
|
Human insulin crystal dissolve rapidly after S.C. injection - gives rapid onset and shorter duration
|
|
|
What physical features characterize an Ultralente formulation?
|
Large crystals of insulin with high zinc content. Relatively insoluble
|
|
|
Amorphous(non-crystalline) insulin precipitated at high pH with zinc. Readily soluble and rapidly absorbed; onset and peak effect are rapid.
|
Semilente
|
|
|
Intermediate acting. Give combo percentages. Provide rapid absorption with sustained action. Therapeutic
|
Lente
70% Ultralente ++ 30% Semilente |
|
|
What is the reason for the switch of two amino acids in Lispro(Humalog)? Which two aa are switched and on which chain?
|
Blocks aggregation-improves solubility. 28 and 29 of the B chain. Pro-Lys switched to Lys-Pro.
|
|
|
Explain Glargine. Soluble at which pH?
|
Soluble in solution at pH4, but precipitates after S.C.(pH 7), forming a microprecipitate depot. Insulin slowly dissolves from the depot providing peakless basal insulin replacement
|
|
|
Is Detemir long or short acting?
what structural feature causes this? What does it bind to? |
Long action. Addition of 14-carbon fatty acid binds plasma albumin, increasing DOA.
|
|
|
What is a feature of all sulfonylureas?
|
Feature a urea function with a sulfonyl group directly attached to one of the urea nitrogens.
|
|
|
A first generation sulfonylurea with a chloro group that blocks oxidation to the carboxylic acid, which prolongs DOA.
|
Chlorpropamide
|
|
|
Second generation sulfonylureas have this feature. Purpose?
|
Large non-polar substituent on the benzene ring. Improves potency
|
|
|
Sulfonylurea MOA?
|
interact w/ various pancreatic beta-cell receptors to block ATP-gated K+ channels. This depolarizes the cell, opening Ca++ channels. Ca influx induces beta-cell insulin secretion
|
|
|
What first generation provided the core for the second generation sulfonylurea?
|
Acetohexamide
|
|
|
This generation of Sulfonylureas have no metabolites that exhibit useful theraeutic activity
|
2nd gen
|
|
|
Name 2nd gen Sulfonyls.
|
Glipizide. Glyburide
|
|
|
Meglitinides(Repaglinide):
a) MOA b) duration and potency compared to Glyburide c) how metabolized |
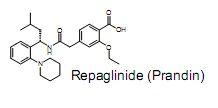
a) Binds to a unique site as well as sites in common with sulfonyls. Closes ATP-dependant K+ channels in Beta-cell membranes. Depolarizes to open Ca channels. Insulin secreted.
b) more rapid and shorter acting and 10X more potent(free of prolonged hyperinsulinemia seen with various sulfonlyureas). c) Glucoronidation |
|
|
Second Meglitinides that was approved in 2000. Free of prolonged hyperinsulinemia.
|
Nateglinide(Starlix)
|
|
|
GIve some importatn components of metformin's action
|
1. inhibits gluconeogenesis
2. increases anaerobic glucose use in the small intestine 3. increases aerobic glucose use in other tissues. OVERALL increases glucose utilization |
|
|
Does not induce hypoglycemia at any reasonable dose. Not protein bound or metabolized, but undergoes rapid renal elimination. Active in pts unresponsive to sulfonylureas. DOA 12-12 hours
|
Metformin
|
|
|
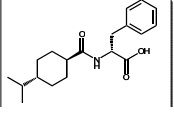
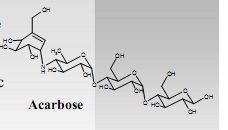
A pseudotetrasaccharide with the ABILITY TO COMPETITIVELY INHIBIT ALPHA-GLUCOSIDASE VIA THE BASIC SECONDARY AMINE OF THE CARVSINE UNIT.
|
|
|
|
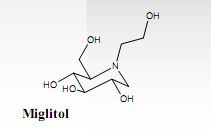
A small molecule alpha-glucosidase inhibitor that is rapidly abosorbed into the blood following oral admin.
|
|
|
|
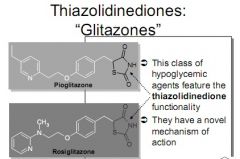
Lowers blood glucose levels by improving target tissue(adipose, skeletal muscle, and liver) sensitivity to insulin(also referred to as insulin enhancers. Name two drugs and class
|
|
|
|
What do Thiazolidinediones bind to? What does this do in the presence of insulin. What follows?
|
|
|
|
|
|
|
|
|
|
What makes estrogen susceptible to sulfation or glucoronidation?What makes estrogen susceptible to sulfation or glucoronidation?
|
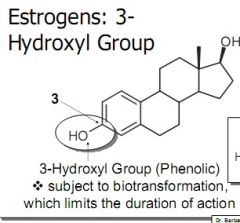
3-Hydroxyl Group
|
|
|
A water soluble estrogen conjugate administered orally for its estrogenic effects and that requires intestinal sulfatases for in vivo activation
|
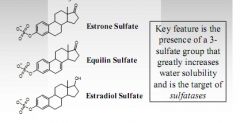
sulfate group present. From Mare's urine
|
|
|
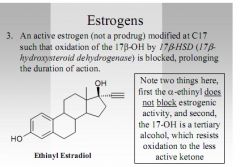
An Active estrogen(not a prodrug) modified at C17 such that oxidation of the 17B-OH by 17B-HSD) is blocked, prolonging duration of action
|
|
|
|
A long acting lipophilic ester prodrug of a natural estrogen employed IM for prolonged estrogenic actions.
|
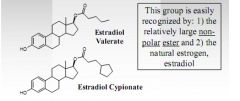
|
|
|
A semi-synthetic estrogen prodrug that requires P450-mediated dealkylation(or demethylation) to give active species.
|
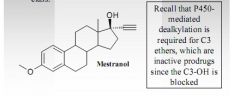
|
|
|
A totally synthetic estrogen(as opposed to semi-synthetic estrogen) that is employed in estrogen-sensitive breast cancer. Five examples given in lecture
|
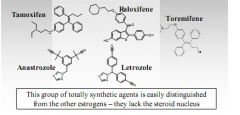
|
|
|
A natural product( flavonoid) present in certain vegetables(such as soy) that has weak estrogenic activity( a phytoestrogen).
|
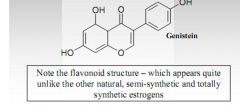
|
|
|
What is the name(chemical and common) of a selective estrogen receptor modulator(SERM) that lacks uterine and mammary effects, but prevents bone loss and lowers cholesterol in post menopausal women?
|
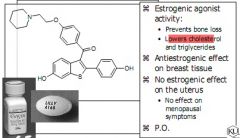
Exhibit mixed agonist/antagonist activity at estrogen receptors.
|
|
|
The progestin with the lowest oral bioavailability due to rapid first pass metabolism in the liver
|
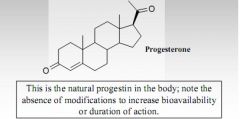
|
|
|
A long acting highly lipophilic progestin prodrug used IM in oil.
|
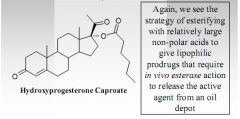
|
|
|
Orally very active progestins(employed in oral contraception) that are less susceptible to 3-keto-4-ene reduction than progesterone.
|
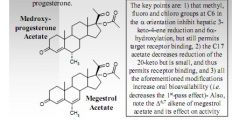
|
|
|
A 19-norandrostane C13-etyl derivative that requires metabolism by the intestinal mucosa and/or liver to give the active species. Considered a pro-progestin
|
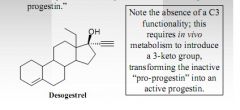
|
|
|
An oral contraceptive that resists 17beta-OH metabolic and bacterial oxidation to the 17-keto. Five examples given in class
|
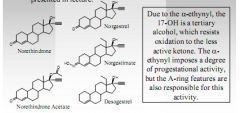
|
|
|
A progestin derivative that resists 20-keto reduction to the less active(and readily conjugated) alcohol.
|
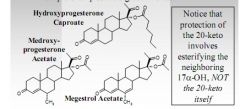
|
|
|
A progesterone receptor antagonist that possesses abortifacient properties with a N,N-dimethylamino-phenyl fucntion that mediates, in large part, the progesterone receptor antagonism.
|
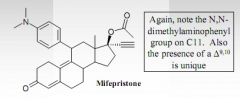
|
|
|
The natural androgen that undergoes significant first pass metabolism in the liver, and therefore exhibits low oral bioavailability
|
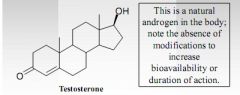
|
|
|
An ester prodrug that exhibits primarily androgenic effects and is administered IM for prolonged action
|
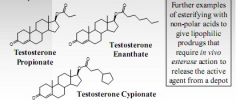
|
|
|
The orally active androgen that provides the greatest androgenic activity
|
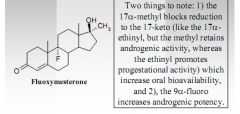
|
|
|
The orally active drug that provides the greatest anabolic over androgenic activity.
|
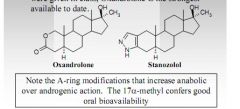
|
|
|
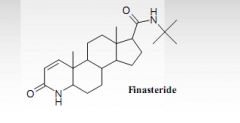
A 5-alpha-reductase competitive inhibitor that is employed to treat BPH and male pattern baldness(androgenic alopecia) by decreasing the xversion of testosterone to dihydrotestosterone
|
|
|
|
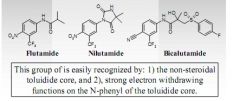
a non-steroidal androgen receptor antagonist employed in the Rx of prostate cancer.
|
|
|
|
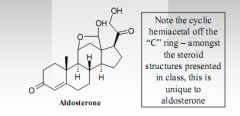
The natural adrenocorticoid with the highest potency for retaining sodium in humans
|
|
|
|
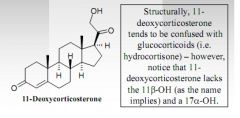
A mineralocorticoid with 1/10th the potency of aldosterone d ue to the absence of the hemiacetal bridge(11B-Oh and 18-aldehyde absent)
|
|
|
|
The primary natural glucocorticoid in humans
|
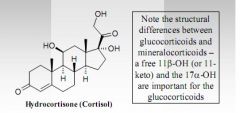
|
|
|
A glucocorticoid ester prodrug useful for IV admin.
|
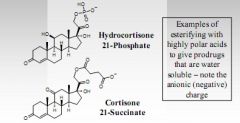
|
|
|
An ester of the 21-hydroxyl group of cortisone, that gives a highly liphophilic produrg for IM depot admin.
|
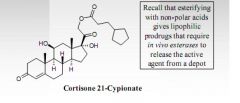
|
|
|
A semisynthetic glucocorticoid with roughly 4X the anti-inflmmatory action of hydrocortisne(cortisol_), but only slightly less salt-retaining activity than hydrocortisone
|
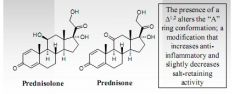
|
|
|
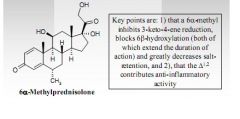
A semi-synthetic glucocorticoid with prolonged DOA resulting from inhibition of 3-keto-4-ene reduction due to a methyl substituent and increased anti-inflammatory activity over hydrocortisone due to a delta1,2-alkene.
|
|
|
|
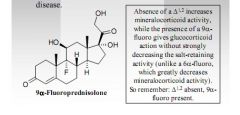
A semi-synthetic glucocorticoid w/ mineralocorticoid activity; used in treating Addison's disease
|
|
|
|
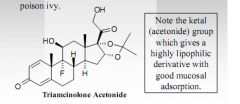
A semi-synthetic ketal glucocorticoid w/ substantial topical anti-inflammatory activity largely due to its high lipophilicity; useful for treating poison ivy
|
|
|
|
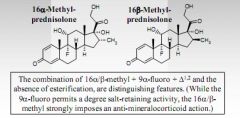
A glucocorticoid that exists in two isomeric forms. Both demonstrate 30-35X the anti-inflammatory action of hydrocortisone with greatly reduced salt-retaining activity
|
|
|
|
A semi-synthetic glucocorticoid ester prodrug widely used in inhalers for asthma and/or allergic rhinitis
|
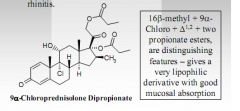
|
|
|
what are three organs involved in Vit D production?
|
Skin, liver, and kidneys
|
|
|
If an excess for vitamin D3 is present in the body, what organ plays a key role in eliminating this excess? What
chemical modification of vitamin D3 facilitates this elimination? |
Kidneys. Hydroxylation at C24 blocks receptor binding (inactivates) and increases the polarity (aqueous solubility) for renal elimination.
|
|
|
What organ forms active Vit. D
|
Kidneys
|
|
|
Note the structural differences b/w the storage, active and inactive forms of Vit. D3
|
All have the basic D3 core structure, but the storage
form has a single hydroxyl at C25, while the active form features a second hydroxyl at C1- a key feature for good receptor binding. As noted above, the inactive forms are hydroxylated at C24, a modification that decreases receptor binding. Generally speaking, the polarity (aqueous solubility) increases from storage to inactivation/elimination via the renal route. |
|
|
A guy comes to you claiming...
A guy comes to you claiming he was diagnosed with hypocalcemia and that his physician recommends supplementation with oral vitamin D and calcium. Unfortunately, this chap is very frugal, and has decided to “self- medicate” with 7-dehydrocholesterol purchased from Aldrich at $72.60 for 25 g through a chemist friend. (He figures that at 10mg/day this supply is good for 6.8 years.) He reveals that he works strictly graveyard shifts, sleeps during the day, and prefers the dark (no, his name is not Count Dracula). Using the chart on page 4 of the Calcium Modulation handout, do you think this gentleman’s approach will be successful? Why or why not? |
UV irradiation is req. for B-ring fission of 7-dehydrocholesterol to give Cholecalciferol(D3)), which leads to storage then active form
|
|
|
Which of the vitamin D preparations
presented in lecture are appropriate for treating hypocalcemia in combination with oral calcium supplements in a patient with frank liver disease (impaired liver function)? |
The key point is that any vitamin D
preparation given to a patient with depressed liver function should not depend on hepatic bioactivation. Calciferol [25(OH)D3], Calcitriol [1,25(OH)2D3] and Paricalcitol are reasonable choices. |
|
|
Suppose a genetic defect leads to very low
expression of vitamin D 1α-hydroxylase. Which of the vitamin D preparations given in lecture are appropriate for treating hypocalcemia in such an individual? |
This question now assumes that kidney
bioactivation is compromised; agents that avoid vitamin D 1α-hydroxylase mediated activation should work. Dihydrotachysterol [DHT], Calcitriol [1,25(OH)2D3] and Paricalcitol are reasonable. |
|
|
Why is calcitonin-salmon preferred over
human calcitonin? |
CT-Salmon has greater potency (about 50X)
and a longer half-life than human CT. |
|
|
Are there any considerations or concerns
regard ongoing use of calcitonin-salmon? |
Being a foreign peptide, systemic allergic
reactions are possible and/or neutralizing antibodies can render the agent inactive. |
|
|
What benefit does CT-Salmon have
beyond controlling hypercalcemia and disorders of bone remodeling? |
Potent analgesic effect
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|
|

|
|
|

|
|
|
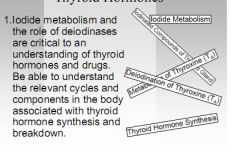
3.It is important to know and understand the
different options for natural and synthetic thyroid drug treatment, as well as the identities of antithyroid drugs: |

|
|
|
|
|
|
Cholesterol:
Be familiar with drug therapy options to decrease plasma cholesterol and LDL levels, to increase triglyceride clearance and to decrease VLDL formation. Understand mechanism of action for each class. |

|

