![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
After injury, tissue repairs (heals) via what two mechanisms? |
regeneration OR scar formation |
|
|
___________ involves proliferation of residual cells or stem cells and maintains the original tissue type |
regeneration |
|
|
_________ involves fibrosis CT deposition, NOT original tissue type bc tissue has limited regenerative capacity and/or the CT foundation is damaged, creates tissue "patches" where damaged tissue was |
scar formation |
|
|
Tissue are divided into what 3 types based on regenerative capacity? |
1. Labile= stem cells & continuously proliferating mature cells, includes hematopoietic cells & epithelium
2. Stable= quiescent (Go stage) cells, capable of dividing in response to injury, includes parenchyma, smooth muscle, fibroblasts
3. Permanent= terminally differentiated tissues, do NOT regenerate, includes brain & myocardium |
|
|
How do growth factors lead to cell proliferation?
(reminder: macrophages, epithelium, & stroma produce GFs) |
GFs bind to target cell receptors--> activate signal transduction pathway--> up-regulate proto-oncogenes--> cell enters & progresses through cell cycle |
|
|
How are integrins involved in cell proliferation? |
link the extracellular matrix (ECM) to the cytoskeleton---> formation of focal adhesion complexes--> signals nucleus--> proliferation & differentiation occurs |
|
|
What organ has amazing regenerative capacity, & can double itself in one month if necessary?
Via what mechanisms does it proliferate? |
liver
proliferation via 2 ways: 1. proliferation of all residual hepatocytes 2. repopulation from progenitor cells at focal areas
(^triggered by cytokines & growth factors) |
|
|
What are the 3 stages of Hepatocyte proliferation? |
1. priming- cytokines (IL-6) activate/prime hepatocytes
2. growth factor- GFs stimulate primed hepatocytes to enter cell cycle
3. termination- return hepatocytes to quiescence (Go) (antiproliferative cytokines) |
|
|
what are the steps involved in scar formation? |
1. angiogenesis
2. formation of granulation tissue
3. remodeling of connective tissue |
|
|
What role do macrophages play in injury repair? |
-clear offending agents & dead tissue -provide growth factors for cell proliferation -secrete cytokines to stimulate fibroblast proliferation & CT synthesis & deposit
(mostly M2) |
|
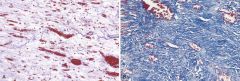
What kind of stain are these? What do the 2 images show? |
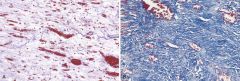
Trichome stain= blue collagen L. formation of granulation tissue, numerous BVs, edema, & loose ECM w/ inflammatory cells & a few collagen fibers R. Mature scar w/ dense collagen |
|
|
What occurs during angiogenesis? |
new BV (capillary sprouts) are developed from existing vessels -stalk cells line new branch (from existing vessel) w/ tip cells are the tip of the stalk -the tip cells migrate & proliferate, causing the new BV (stalk) to grow |
|
|
________ are the growth factors that stimulate the ENDOthelial tip & stalk cells to migrate & proliferate, also stimulate NO production (vasodilation) |
VEGF-A (vascular endothelial growth factors) |
|
|
_______ assist VEGF-A to stimulate proliferation as well as promote migration of macrophages & fibroblasts to injury Also stimulate EPIthelial cells to migrate & cover epidermal wounds |
FGF-2 (fibroblast growth factors) |
|
|
What do Ang 1 & Ang 2 (angiopoietins) do? |
BOTH bind to Tie2 on ENDOthelial cells
Ang 2= dettaches pericytes & promotes destabilization of vessels (so that migration of new vessel can occur)
Ang 1= recruits new pericytes & promotes stabilization of vessels (so that new vessel can proliferate & stabilize) |
|
|
_____ assists Ang 2 in destabilization by degrading extracellular matrix components (further promoting capillary sprouting) |
MMPs (matrix metalloproteinases) |
|
|
__________ provide the scaffold (architecture) for new vessel growth. They also participate in sprouting via interactions w/ integrins on the endothelial cells |
ECM proteins (extracellular matrix proteins)
|
|
|
____________ recruits smooth muscle cells to stabilize newly formed large blood vessels |
PGDF
(pericytes will be recruited to stabilize smaller vessels) |
|
|
Describe Notch signaling |
DlL4 on tip cells binds to Notch receptors on stalk cells---> Notch intracellular signaling domain translocates to the nucleus--> nucleus activates genes that decrease stalk cell response to VEGF--> STOPS proliferation & migration |
|
|
___________ suppresses endothelial proliferation & migration (terminates angiogenisis) & enhances production of ECM proteins= additional stabilization of new vessels |
TGF- beta |
|
|
TGF-beta is also an important in the formation of granulation tissue (next step in scar formation) What does it do? |
stimulates; -fibroblast migration & proliferation -collagen & fibronectin synthesis -formation of loose connective tissue
& decreases ECM degradation |
|
|
Describe the last step of scar formation, remodeling of connective tissue |
-vessel & fibroblast proliferation decreases -progressive vascular regression -fibroblasts transform into myofibroblasts
---> eventual inc. in CT, reorganization, & finally granulation tissue evolves into a scar |
|
|
_________ exhibit some contraction, causing the scar to shrink |
myofibroblasts |
|
|
Initially during scar formation, MMPs are actively remodeling the deposited ECM, then their activity is inhibited by _________ |
TIMPs |
|
|
What is fibrosis? What causes it? What does it lead to? |
-excessive deposition of collagen in tissue
-caused by chronic inflammation/injury
-leads to organ dysfunction, due to change in tissue type, Ex: Fibrosing lung disease, liver cirrhosis, systemic sclerosis |
|
|
What triggers fibrosis? |
TGF-beta
(cell death & ROS activate TGF-beta)
|
|
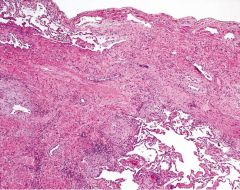
What is this image showing? |
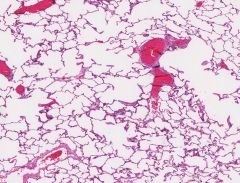
Lung w/ pulmonary fibrosis
(*this is a normal lung) |

