![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
The primitive heart tube (mesoderm) forms by ________ gestation. Neuroectoderm migrates in & contraction can be seen even early at ________ |
heart tube form- 22 days
contraction as early as -20 days |
|
|
At_________ the heart "loops" and by ________ septation begins |
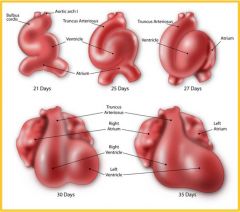
22-24 days- heart loops 26 days- septation begins |
|
|
Septation downward forms the _________ septum, made up of 2 layers the ostium secundum & septum primum. What do these form? |
atrial septum
foramen ovale |
|
|
Fetal blood flows through the foramen ovale in what direction? |
R---> L |
|
|
Septation upward forms the ________ septum. |
ventricular spetum |
|
|
A spiral downward migration from the outflow tract (truncus arteriosus) aligns the ventricles with the developing ________________ |
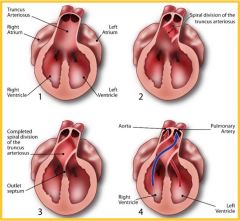
great arteries |
|
|
The truncus arteriosus develops into the _________ |

aortic arches |
|
|
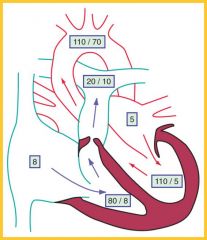
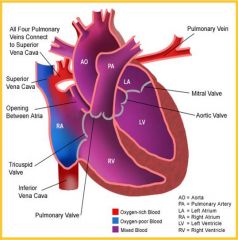
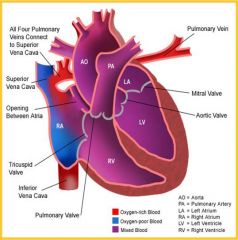
Fetal oxygenation occurs at the ___________ not at the lungs |
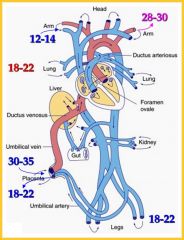
placenta
(KNOW this image*) |
|
|
Fetal Hb (HbF) has a (higher/lower) pO2 than adult & a (higher/lower) saturation |
lower pO2 (around 30 instead of 50)
higher saturation (HbF has a much higher affinity) |
|
|
What rapid changes occur in the Fetal-Neonatal transition? |
-pulmonary vascular resistance drops & flow inc (inc pO2, more air goes to lungs) -Inc flow--> inc venous return--> enlarges L atria & closes foramen ovale -Systemic resistance inc (forcing more blood to lungs) -ductus arteriosus flow reverses |
|
|
What slower changes occur in the Fetal-Neonatal transition? |
-closed foramen ovale -ductus venosus closes = ligamentum venosum -ductus arteriosus closes= ligamentum arteriosum -L ventricle grows & thickens (now pumps blood to entire body) |
|
|
3 most common genetic associations w/ congenital heart disease (CHD) |
trisomy 18 (Edwards Syndrome) trisome 21 (Down Syndrome) 45, XO (Turner Syndrome) |
|
|
what CHD? -bicuspid aortic valve -paradoxically split S2 -decreased pulse intensity -early systolic ejection click or ejection murmur RUSB -symptoms often unnoticed |
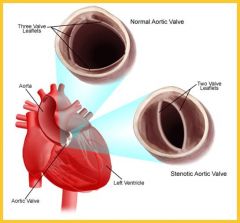
Congential aortic stenosis
(valve doesn't open wide enough) |
|
|
Although congenital aortic stenosis is usually not problematic, what are some treatment options?
(GOOD OUTCOME for this disease) |
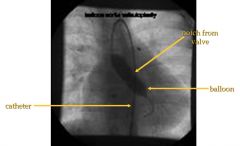
-balloon valvuloplasty (image) (place catheter up femoral a & blow up balloon to expand valve)
-aortic vavle replacement |
|
|
what CHD? -disparity in extremity pulses -mild may present as leg pain/weakness in teens -severe LE sats will be low -longterm left ventricular hypertrophy & notching of ribs
|
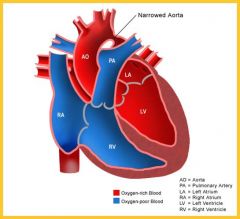
Coarctation of the aorta (R ventricle feeds into descending aorta via patent ductus areriosus) |
|
|
Coarctation of the aorta has much better outomes if treated early. If treated late it may lead to CV disease & premmature death. What are the treatments? |
-immediate PGE1 (keepts ductus arteriosus open during surgery)
-surgical repair (remove coarctation & resect) |
|
|
what CHD? -usually asymptomatic -severe causes cyanosis or CHF -sharp pulmonic ejection click -split S2 -low pitched systolic ejection murmur (LUSB) -right ventricular hypertrophy (RVH) -spiked p wave on EKG
|
Pulmonic valve stenosis |
|
|
In severe cases of pulmonic valve stenosis where CHF may occur, what are the treatment options? |
-Balloon valvuplasty (through femoral vein (not artery) |
|
|
What CHD? -often asymptomatic (if small) -large shunts easily identified -L--> R shunt -wide fixed-split S2 -mumur if small -low-pitched mid-diastolic rumble (LLSB) |
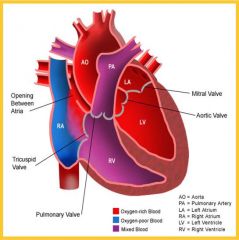
Atrial septal defect (ASD)
(increased flow from RA to RV) |
|
|
Large atrial septal defects are usually noticed early & have good outcomes w/ tx. Asymptomatic patients with Qp:Qs of ______ or greater should also be treated. What are the treatment options? |
Qp:Qs of 2:1 or greater
-surgical or transcatheter closure (shunt through femoral v. then opens like umbrella closing)
|
|
|
what CHD? -normal at birth -symptoms develop later at Rpulm drops -L--> R shunt -cyanotic if Rpulm:Rsyst = 1 (bidirectional shunt) -blowing holosystolic murmur -if large dyspnea, feeding difficulty, poor growth, heart failure, dusky w crying -biventricular hypertrophy EKG -peaked or notched p waves EKG |
Ventricular Septal Defect (VSD)
(2nd most common CHD) |
|
|
Outcome for ventricular septal defects is good if small or repaired early. If not they can lead to pulmonary complications. What are the tx? |
-surgical repair
-palliative PA banding to delay repair (if muscular or "swiss cheese" VSD, may want to delay) |
|
|
What CHD? -similar symptoms to VSD -growth retardation (if large) -wide pulse pressure -heaving apical impulse -continuous machinery-like murmur -may close in first year -incr risk of bacterial endocarditis if large -CHF if large |
Patent Ductus Arteriosus (PDA) |
|
|
What are the treatment options for patent ductus arteriosus? |
-surgical closure -transcatheter (coil) embolization (coil clogs/fibrosis & causes closed block) |
|
|
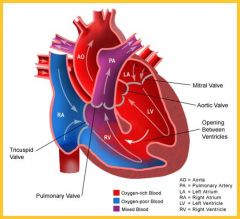
what CHD? -L--> R shunt -cyanosis w/ RVH & incr RV outflow obstruction -dyspnea/fatigue w/ exertion -"Tet" spell (paraxysmal hypercyanotic attacks)--> metabolic acidosis -loud harsh systolic murmur -single S2 or soft P2 -delayed growth |
tetralogy of fallot
(descending septum doesn't meet ascending septum) |
|
|
Tetralogy of Fallot should be treated asap to prevent growth & development problems. What are the treatment options? |
-PGE1 (palliative to maintain ductal flow) -Tet spell management (keep calm) -surgical palliation/correction (aortic pulmonary shunt)
|
|
|
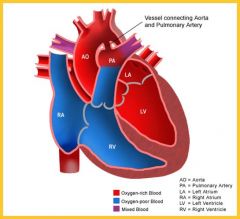
What CHD? -VERY cyanotic -tachypnea -severe hypoxemia, worsens as DA closes -CXR: Egg on a string (egg shaped heart, narrow mediastinum) |
transposition of great arteries (descending septum stays straight, vessels align w/ wrong ventricles) |
|
|
Transposition of the great arteries is fatal if untreated, if foramen ovale & ductus close completely there is no oxygenation of systemic blood. What are the treatments? |
-PGE1 (if not completely closed to keep open)
-atrial septostomy (allows mixing but messy)
-arterial switch (Jatene procedure) (^BEST option, actually remove & reattach vessels to right place) |
|
|
Which CHD's cause cyanosis? |
(5 T's & an H) -Tetralogy of Fallot -Transposition of great arteries -Truncus arteriosus -Tricuspid atresia -Total anomalous Pulmonary Venous Return -Hypoplastic Left Heart |
|
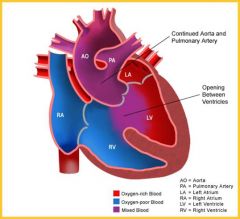
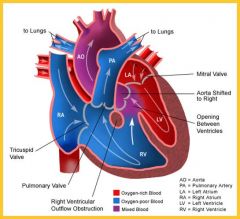
What CHD? |
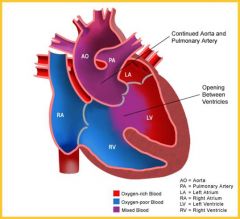
truncus arteriosus
(single outflow, single ventricle, high risk R HF) |
|
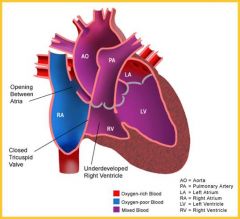
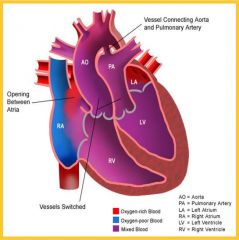
what CHD? |
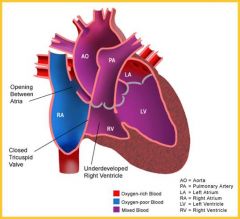
tricuspid atresia
(underdeveloped RV, two ventricles not separated) |
|
What CHD? |
Total anamalous pulmonary venous return (all pulmonary veins in wrong place, complete mixing of oxygenated & unoxygenated blood) |
|
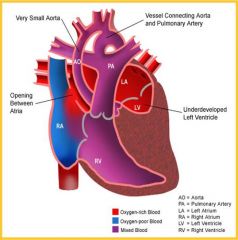
What CHD? |
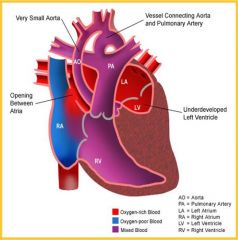
Hypoplastic left heart
(tiny left heart, no right to left connection) |

