![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
145 Cards in this Set
- Front
- Back
|
What percentage of Australians have osteoarthritis?
|
20%
|
|
|
What is the most common joint disease in the world?
|
Osteoarthritis
|
|
|
T/F: Osteoarthritis is a disorder or hyaline cartilage
|
FALSE - disease of WHOLE JOINT
|
|
|
What are some pathological features of OA?
|
Cartilage loss
Bone remodelling/sclerosis Capsular thickening and distension Synovial inflammation Muscle atrophy and weakness |
|
|
T/F: OA occurs when the dynamic equilibrium between the breakdown and repair of joint tissues is overwhelmed
|
TRUE
|
|
|
What are the criteria for diagnosis of OA in the hip?
|
Hip pain and at least 2 of the following:
1. Erythrocyte sedimentation rate < 20mm/hr 2. Radiographical femoral or acetabular osteophytes 3. Radiographic joint space narrowing |
|
|
What are the criteria for diagnosis of OA in the hand?
|
Hand pain, aching, or stiffness and 3 of the following features:
1. Hard tissue enlargement of 2+ joints out of 10 2. Hard tissue enlargement of 2+ DIP joints 3. Fewer than 3 swollen MCP joints 4. Deformity of 1+ of 10 selected joints |
|
|
When diagnosing OA in the hand, what are the 10 "selected joints"
|
On both hands:
2nd and 3rd DIP 2nd and 3rd PIP 1st CMC |
|
|
What accounts for most cases of idiopathic hip OA?
|
Femoroacetabular impingement
|
|
|
What percentage of women and men over 70 have symptomatic hand arthritis?
|
26% women
13% men |
|
|
Increased BMI is associated with increased prevalence of OA in which joints?
|
Knee
Hip Hand |
|
|
Losing 5kg will reduce chance of developing OA by how much?
|
50%
Also slows progression |
|
|
In persons with history of prior knee injury, what is their lifetime risk of knee OA?
|
57%
|
|
|
What 'causes' OA ?
|
1. Systemic factors increase vulnerability of joint to OA
[age, gender, bone density, nutrition, genetics] 2. Mechanical factors facilitate progression to OA |
|
|
What mechanical factors facilitate progression to OA ?
|
Malalignment
Muscle weakness Alterations in structural integrity of joint environment Loading affected by injury or obesity |
|
|
In OA, what structures within the joint can be responsible for pain?
|
Joint capsule, ligaments, outer 3rd of meniscus, periosteal and subchondral bone, synovium, soft tissues
|
|
|
T/F: There are pain fibres in cartilage
|
FALSE.
CARTILAGE IS AVASCULAR AND ANEURAL |
|
|
Fill gap with MEN/WOMEN:
1. OA of knees more common in ______ 2. OA of hips more common in ______ |
1. OA of knees more common in WOMEN
2. OA of hips more common in MEN |
|
|
T/F: OA usually develops slowly, with mechanical pain arriving first
|
TRUE
|
|
|
T/F: Once progressed to OA, will continue to have symptoms for life
|
FALSE.
Symptoms can be intermittent - can have years pain-free |
|
|
T/F: OA affects pairs of joints (e.g. both hands) equally
|
False.
Often asymmetric |
|
|
Other than osteoarthritis, what types of arthritis can affect the hip, knee or hand?
|
Rheumatoid arthritis
Psoriatic arthritis Sarcoidosis Other seronegative spondyloarthropathies [ankylosing spondylitis, reactive arthritis, arthritis ass'd with IBD] |
|
|
What would cause bowing of the tibia in OA?
|
Lost joint space - sclerotic changes of bone
|
|
|
Disability is more prevalent in disease of which joint within the knee?
|
Patellofemoral j.
|
|
|
Which joint affects hand functionality the most?
|
1st carpo-metacarpal joint
|
|
|
What are the CHARACTERISTIC symptoms of OA?
|
- Mechanical pain (occurs w activity, relieved w rest)
- Pain usually gradual in onset - Morning stiffness absent or lasts under 30 min - If severe, pain can be present at night and at rest [Some other symptoms: crepitus, joint swelling, reduction in ROM, lower limb j's may buckle] |
|
|
What clinical signs would you see on PEx of OA?
|
Tenderness over joint line
Crepitus with movement of joint Bony enlargement of joint Reduced ROM Joint swelling Joint deformity Instability of joint |
|
|
What are Heberden's and Bouchard's nodes?
Are men or women pre-disposed to these? |
Bony enlargement due to OA in joint.
Heberden = DIP Bouchard = PIP [More frequently found in women post-menopause] |
|
|
What are the radiographic features of OA?
|
Osteophyte formation
Joint space narrowing Subchondral sclerosis Subchondral cysts |
|
|
T/F: The shorter the wavelength, the lower the energy
|
FALSE.
Short wavelength = high energy |
|
|
List the following from low to high energy:
Visible light UVC UVA1 UVA2 UVB |
[low E]
Visible UVA1 UVA2 UVB UVC [high E] |
|
|
How do you calculate "exposure dose" of UV?
|
Exposure dose = irradiation x time
|
|
|
The ozone layer absorbs which EMR spectrums?
|
UVB and UVC.
It does not absorb UVA or visible light |
|
|
T/F: UVB transmission varies exponentially with ozone concentration
|
TRUE
|
|
|
What percentage of UV radiation is "diffuse"
|
50% UV back-scatters (even if standing in shade, will still get UV)
|
|
|
In the lower atmosphere, are low or high energy wavelengths more easily scattered?
|
High energy
|
|
|
Which spectrum of UV penetrates further into the skin?
|
UVA.
[Since UVB is very energetic, it will be easily diverted.] |
|
|
T/F: Need 1000x more UVA to cause sunburn than UVB
|
TRUE.
NOTE - while UVB more energetic and thus easily diverted, its greater energy can cause more cell damage once penetrates skin |
|
|
What does photoaddition mean?
|
Same dose UV – doesn’t matter if in 10 secs or 10 mins
|
|
|
Can DNA damage trigger UV immunosuppression?
|
Yes
|
|
|
What is the mechanism involved in UVB carcinogenesis?
|
DIRECT DNA DAMAGE:
Formation of pyrimidine dimers in DNA (pholesions). These are repaired by the nucleotide excision repair pathway. Excessive sun exposure overwhelms this pathway --> faulty repair --> mutations OXIDATIVE DNA DAMAGE: 8-oxo-guanosine (8oxoG) |
|
|
What is an action spectrum?
What is the action spectrum for DNA damage the same as? |
The most effective wavelengths for producing a certain response.
DNA damage action spectrum same for sunburn and tanning |
|
|
What skin conditions (other than cancer) occur with chronic UV exposure?
|
Telangiectasia (permanently dilated blood vessels)
Solar lentigines ie. freckles Solar elastosis (elastin fibres clump together just under epidermis) Solar keratoses (rough scaly spots) |
|
|
What dose of UV is needed for immunosuppression?
|
1/3 MED
|
|
|
UV has suppressive effects on which cells?
|
Langerhans cells
T lymphocytes Mast cells Macrophages |
|
|
On an average day (even if wearing sunscreen), the skin screens out which spectrum of UV better?
|
UVB
|
|
|
What are some defences against UV damage?
|
1. SKIN THICKENING
moreso epidermal thickening single UVB exposure can double skin thickness 2. MELANIN absorbs UV and visable light Quenches free radicals 3. DNA REPAIR Photolesions repaired within 2 hrs |
|
|
Sensitivity to sunburn is determined by what?
|
Melanin pigment in skin
Skin thickness |
|
|
T/F: Because dark skin has melanin, it is protective against immnosuppression.
|
FALSE. Does not protect against immunosuppression.
|
|
|
Can use UVB to treat:
|
Psoriasis, eczema, hand dermatitis
Vitiligo Cutaneous T cell lymphoma Graft versus host disease |
|
|
Can use high doses of UVA1 to treat:
|
Eczema
Scleroderma SLE (improves arthralgia, fatigue and skin) |
|
|
How does visible light treat unconjugated bilirubin?
|
Photoisomerisation of bilirubin to water soluble lumirubin (not as toxic as bilirubin.. Doesn’t get into brain
|
|
|
What is photodynamic therapy?
|
Shining visible light in presence of a photosensitiser (eg, drugs, porphyrins) to cause burning, blistering - can treat superficial skin cancers
|
|
|
How can you decrease compressive load in managing OA?
|
Education
Weight loss Exercise/physical therapy Orthoses |
|
|
Overweight patients with symptomatic OA of the knee are recommended to lose how much weight?
|
At least 5% of body weight
|
|
|
Patients with symptomatic OA of the knee are recommended to do what?
|
Lose at least 5% body weight if overweight
Participate in low-impact aerobic fitness exercises Quadriceps strengthening Range of motion/flexibility exercises are an option |
|
|
What is the point of exercise in managing OA?
|
Combination of strength training and aerobic conditioning leads to improvements in strength, proprioception, pain and function
[can't just be a sheet of exercises though] |
|
|
T/F: Lateral heel wedges and/or braces are useful in mechanical interventions of knee OA
|
False. Neither can be recommended.
|
|
|
What percentage of adults with OA use complementary/alternative medicine?
|
30-47% of older adults with osteoarthritis use CAM.
|
|
|
T/F: Glucosamine and/or chondroitin sulfate or hydrochloride are effective alternative treatments in OA
|
FALSE. Recommended that they are NOT prescribed.
|
|
|
What is the analgesic of choice for mild to moderate pain from OA?
|
Oral paracetamol up to 4g/day
[NSAIDs should be added or substituted in patients who respond inadequately] |
|
|
When might opioids be used as analgesics in OA?
|
Opioid analgesics are useful alternatives in patients in whom NSAIDs are contraindicated, ineffective and/ or poorly tolerated.
|
|
|
Should needle lavage be used in symptomatic OA of the knee?
|
NO
|
|
|
T/F: intra-articular corticosteroids for short-term pain relief for patients with symptomatic OA of the knee is suggested
|
TRUE
|
|
|
T/F: We recommend performing arthroscopy with debridement or lavage in patients with a primary diagnosis of symptomatic OA of the knee.
|
We recommend AGAINST performing arthroscopy with debridement or lavage in patients with a primary diagnosis of symptomatic OA of the knee.
|
|
|
For knee and hip OA, when is total joint replacement indicated?
|
Night pain unresponsive to anti-inflammatory drugs
Major inability or difficulty to perform activities of daily living Unacceptable reduction in the ability to walk or work |
|
|
From what do squamous cell carcinomas commonly develop?
|
From a solar keratosis [pre-malignant lesion]
|
|
|
T/F: SCC can develop from previous skin diseases (s.a. TB, leprosy)
|
TRUE
|
|
|
What happens if SCC not recognised early?
|
Can METASTASIZE
to local lymph nodes --> distant organs --> can ultimately kill Pt |
|

What is this and why?
|
BCC
- Presents as pearly nodules with blood vessels coursing over them - May ultimately ulcerate |
|

What is this and why?
|
SCC.
Develop in skin as nodules which ulcerate |
|
|
What is the treatment for SCC?
|
Excision
|
|
|
What is the treatment for BCC?
|
topical imiquimod, excision, radiotherapy, curettage and cautery, liquid nitrogen, photodynamic therapy
|
|
|
How does melanoma present?
|
Usually as black nodules or plaques in skin, which may ulcerate.
|
|
|
What percentage of melanomas spontaneously regress?
|
10%
|
|
|
What is amelanotic melanoma?
|
Melanoma in which pigmentation is minimal
|
|
|
From what to melanomas commonly develop?
|
from acquired or congenital naevi
|
|
|
T/F: by the time melanomas have metastasised, they are usually incurable
|
TRUE.
Metastasise early. First to lymph nodes and then to distant organs [lungs, liver, brain] |
|
|
How is melanoma treated?
|
Wide excision (usually required grafting)
If secondary skin mets, intra-arterial line perfusion |
|
|
What is the fifth most common cause of cancer death in AUstralia?
|
Melanoma
|
|
|
T/F: Rates of non-melanoma skin cancer increase with increased tanning ability
|
FALSE.
Rates of non-melanoma skin cancer decrease with increased tanning ability |
|
|
What type of sun exposure has been linked to melanoma?
|
Intermittent intense sun exposure (e.g. sunbaking)
|
|
|
What is dysplastic naevus syndrome?
|
Individuals have numerous large irregular moles - commonly develop melanoma.
Familial. |
|
|
Which is the most common skin cancer
|
BCC
|
|
|
What is imiquimod? On which type(s) of cancer is it used?
|
Immune response modifier - stimulates attack on tumour.
Superficial and nodular BCC. Doesn't work on morphoeic BCC |
|
|
Side effects of imiquimod?
|
Erythema
Pain, itch Crusting Infection Scarring Systemic interferon effects (flu like symptoms) |
|
|
Tenderness of Actinic Keratoses suggests what?
|
Progression to SCC
|
|
|
What is EFUDIX?
Side effects? |
Uracil analogue; interferes with DNA synthesis.
SIDE EFFECTS: Inflammation Photosensitivity Eye irritation Allergy Systemic absorption |
|
|
Non-melanoma skin cancer will affect what percentage of men and women by age 70?
|
70% men
60% women |
|
|
What is the incidence of melanoma in NSW for men and women?
|
Men: 1 in 25
Women: 1 in 40 cf. QLD --> 1 in 16 |
|
|
What is the SPF of a hat?
|
2-3
|
|
|
T/F: Immune protection correlates with UVA protection
|
TRUE
|
|
|
What is the relationship between smoking and skin cancer?
|
Surgical side effects of smoking
-->wound healing, flap/graft survival, infection Up to 2x risk of AKs, SCC Incr. risk of morphoeic BCC |
|
|
T/F: Low dietary fat linked with UV-induced skin cancer
|
FALSE
High dietary fat linked with UV-induced skin cancer |
|
|
What is the relationship between stress and skin cancer?
|
Increased photocarcinogenesis in chronically stressed mice
|
|
|
What is the relationship between COX inhibitors and skin cancer?
|
? Less NMSC and melanoma in people taking aspirin/NSAIDs
45% reduction in BCC/SCC w celecoxib |
|
|
What are T4 endonuclease V liposomes
|
Enhance DNA repair
Decr. AKs, BCCs in xeroderma pigmentosum patients |
|
|
What is nicotinamide?
|
Activte form of vitamin B3
Precursor of NAD Affects DNA repair enzymes; apoptosis; cellular metabolism Nicotinamide is UV protective in mice and humans |
|
|
What are the main functions of articular cartilage?
|
1. Minimise contact stresses across joints (distributes load)
2. Dissipates some of energy imparted on joint during weight bearing 3. Allows almost frictionless movement b/w 2 articulating surfaces |
|
|
What produces cartilage?
|
Chondrocytes.
Responsible for synthesis and catabolism of ECM |
|
|
T/F: Chondrocytes are aneural, alymphatic but have blood supply
|
FALSE.
Aneural, alymphatic AND avascular |
|
|
How do chondrocytes get nutrients?
|
Diffusion of nutrients from synovial fluid
|
|
|
What percentage of cartilage is water? How is water kept there?
|
80% water.
Kept there by polyanionic proteoglycans which are trapped in network of inextensible collagen fibres |
|
|
What does persistant loading of cartilage do to chondrocytes?
|
Exhausts their capacity to respond metabolically.
-->Disruption of matrix -->Proteolytic cartilage breakdown |
|
|
What are osteophytes?
|
Compensatory growths of bone on the side of joints.
Arises from concomitant pathological changes in subchondral bone. |
|
|
What are the characteristic pathological features of CARTILAGE in an osteoarthritic joint?
|
Disruption collagen fibrillar network
Increased hydration Areas chondrocyte replication Regions cell death Disruption cartilage surface (fibrillation, deep clefts) Vascular invasion of zone of calcified cartilage Tidemark and loss of PGs from matrix |
|
|
T/F: Major trauma to joints and supporting ligaments has strongest association with development of OA
|
TRUE
|
|
|
T/F: OA is negatively associated with osteoporosis
|
TRUE
|
|
|
What are some secondary causes of joint degeneration?
|
Episodes of infection or chronic inflammation
|
|
|
Regular NSAID use is associated with what 'unwanted' effects?
WHY? |
Dyspepsia
Gastric damage Ulcers and bleeding Renal insufficiency [due to inhibition of cytoprotective prostaglandins in gut and of synthesis of vasodilator prostaglandins in kidney] |
|
|
T/F: Aspirin is associated with lowest degree of bleeding out of all the NSAIDs
|
FALSE. highest degree of bleeding
|
|
|
What does aspirin a potent inhibitor of?
|
Platelet COX.
Inhibits synthesis of pro-aggregatory thromboxane A2 |
|
|
Which COX enzyme is inducible in inflammatory cells?
|
COX-2
|
|
|
T/F: COX-2 inhibitors don't have quite the same efficacy as traditional NSAIDs but their gastric side effects have much lower incidence
|
FALSE.
COX-2 inhibitors have comparable efficacy with traditional NSAIDs but their gastric side effects have much lower incidence |
|
|
What is uric acid? In what form does it exist in body?
|
Waste product produced by breakdown of purine nucleotides.
In plasma - mainly as urate ion In acidic urine - 50% urate, 50% uric acid |
|
|
What proportion of uric acid clearance is by the gut?
|
1/3
|
|
|
How is uric acid predominantly cleared?
|
1. Urate carried in plasma
2. Transported to kidneys 3. Filtered 4. Complex handling by renal tubule [reabsorption, secretion, post-secretory reabsorption] 5. Final result = cleared by kidney |
|
|
What happens if urate level rises to supersaturation range?
|
Crystals of sodium urate gradually form in restricted distribution (mainly joints and other connective tissue sites)
|
|
|
Is hyperuricaemia enough to cause crystal formation?
|
NO.
Need favourable balance of nucleating factors with crystal growth inhibitors |
|
|
What produces an acute attack of gout?
What characterises an acute attack of gout? |
the interaction between the crystal and the inflammatory system
(crystal formation generally doesn't cause symptoms) Characterised by abrupt onset over hours of intense pain, usually ass'd with erythema and swelling of involved joint |
|
|
How does chronic gouty arthropathy arise?
|
Usually after several years of acute intermittent attacks.
Heralded by development of tophi+ prolonged attacks. |
|
|
How is gout diagnosed?
|
Finding monosodium urate crystals in synovial fluid
OR From material removed from tophus |
|
|
Why does joint destruction occur in chronic gout?
|
Intraosseous tophi and chronic synovitis
|
|
|
Which inflammatory cell type is involved in reacting to monosodium urate crystals in gout?
|
Neutrophils
|
|
|
Uric acid can exist in which two forms?
|
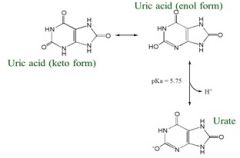
Equilibrium between keto and enol forms.
H+ dissociates from enol form (this is what happens in plasma) |
|
|
In what structures are purines found?
|
Bases e.g. adenine, guanine, hypoxanthine
Nucleotides [remove phosphates first] e.g. ATP, ADP, AMP, GTP, IMP, … Nucleosides [remove ribose first] e.g. adenosine, guanosine |
|
|
T/F: Humans have lost the pathway that breaks down uric acid
|
TRUE
|
|
|
What are some beneficial effects of uric acid?
|
Hypothesised to be an important BIOLOGICAL ANTIOXIDANT (scavenges ROS)
May promote SALT RETENTION under low salt conditions |
|
|
What do uric acid levels depend on?
|
1. Rate of purine nucleotide synthesis and breakdown
2. Dietary purine intake 3. Rates of uric acid excretion |
|
|
What proportion of urate comes from dietary purine breakdown?
|
30%
|
|
|
In which pathway is PRPP important?
a) Salvage pathway b) De Novo synthesis |
BOTH!
|
|
|
Which pathway promotes uric acid production and why?
a) Salvage pathway b) De Novo synthesis |
b) De Novo
loading up with nucleotides that add to the breakdown load |
|
|
Which pathway limits uric acid production and why?
a) Salvage pathway b) De Novo synthesis |
a) Salvage pathway
recycles purines |
|
|
What happens in De Novo Biosynthesis
|
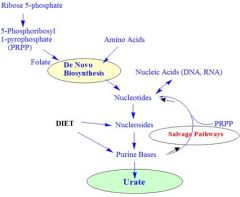
Purines are synthesised on a ribose phosphate backbone
Add 2 phosphates to ribose-5-phosphate to get PRPP which is used as a substrate for purine nucleotides |
|
|
What do the salvage pathways do?
|
Divert purine bases from uric acid synthesis
Recover purine bases for use as purine nucleotides |
|
|
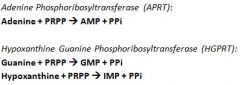
What is Lesch Nyhan Syndrome?
|
X-linked syndrome, deficient in salvage pathway enzyme HGPRT
Have serious problems with CNS development and function and ↑ uric acid production (-->Gout) Mental retardation, self mutilation, growth retardation, chroeoathetosis, spasticity [due to disturbed NT synthesis] |
|
|
What is the impact of ethanol on uric acid production?
|
When we drink, we intake huge concentrations of ethanol (10mM+) so we generate a significant amount of AMP
AMP can be broken down to produce uric acid |
|
|
Clinically, when would we lower uric acid levels?
|
To prevent acute gout attacks
To eliminate tophi To suppress uric acid/ urate in context of tumour lysis syndrome ?? to reverse hyperuricemia in ischemic heart disease, metabolic syndrome |
|
|
T/F: Treating acute gout involves lowering serum uric acid levels
|
FALSE!
Lowering serum uric acid does NOT help ACUTE GOUT – may in fact prolong or trigger attacks |
|
|
How is gout treated?
|
Focus on suppressing acute inflammation – NSAIDs, COX-2 inhibitors (celecoxib) or colchicine (inhibits phagocytosis via microtubule effect)
|
|
|
How are serum uric acid levels lowered?
|
1. BLOCK URIC ACID SYNTHESIS
[by blocking xanthine oxidase with allopurinol] 2. CONVERT URIC ACID TO ALLANTOIN, a water-soluble breakdown product [via uricase] 3. PROMOTE URINARY EXCRETION [via uricosurics] |
|
|
How does blocking xanthine oxidase with allopurinol reduce serum uric acid levels?
|
Xanthine oxidase (XO) promotes hypoxanthine->xanthine->uric acid
Allopurinol is hypoxanthine analog Allopurinol converted to alloxanthine by XO But alloxanthine remains tightly bound in XO’s active site -->XO has undergone SUICIDE INHIBITION by binding and converting allopurinol |
|
|
T/F: Uricase highly effective in mobilising uric acid from tophi
|
TRUE
|
|
|
What do uricosurics do?
|
promote renal excretion of uric acid by blocking reabsorption
|
|
|
What is a potential complication of using uricosurics to reduce plasma levels of uric acid?
|
Get increase RENAL LEVELS of uric acid!
--> greater risk of renal disposition, renal calculi, renal failure |

