![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
AIMS
|
Understand how the Heart and Circulatory System develops throughout life Explain the organising principles of the Heart and Circulatory Systems Describe the co-ordination mechanisms of the Heart and Circulatory System Identify how the Heart and Circulatory System function normally
|
|
|
Functional anatomy of the heart
|
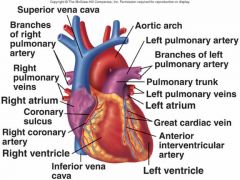
A 4 chambered structure, enclosed within a membrane- the pericardium
Walls of the heart composed of myocardium – specialised muscle cell The chambers are separated by walls of connective tissue – septa The only access between atria and ventricle is via the valves Right side (atria + ventricle) and left side function as 2 separate pumps |
|
|
Normal physiology of the heart
|
The epicardial surface is smooth and glistening
The heart weighs between 7 and 15 ounces (200 to 425 grams) and is a little larger than the size of your fist A human being's heart is about the size of that human being's fist. As the body develops, the heart grows at the same rate as the fist |
|
|
Location of the heart
|
Located in the middle of the chest behind the breastbone, between the lungs, the heart rests in a moistened chamber called the pericardial cavity which is surrounded by the ribcage. The diaphragm, a tough layer of muscle, lies below
|
|
|
The Pericardium
|
The pericardium is the fluid filled sac that surrounds the heart and the proximal ends of the aorta, vena cava and the pulmonary artery
Keeps the heart contained in the chest cavity Prevents the heart from over expanding when blood volume increases Limits heart motion |
|
|
Pericardium
|
2 layers: fibrous pericardium and the serous pericardium
Fibrous pericardium is tough, dense connective tissue that anchors it to the diaphragm, great vessels and sternum. Flexible enough to allow heart some movement e.g. during exercise The serous pericardium: forms a double layer around the heart Outer layer (parietal) lines the inner surface of the fibrous pericardium The inner layer (visceral) – also known as epicardium – ‘upon the heart’ – is attached to the muscle layer of the heart Between the two layers – a thin ‘potential’ space containing serous fluid - the pericardial cavity Holds the two thin layers together and prevents friction between the two layers when the heart contracts |
|
|
Heart Wall
|
Epicardium: (visceral pericardium) an exposed layer of simple squamous epithelium underlain by loose connective tissue
Myocardium: This is the muscular wall of the heart. It primarily consists of cardiac muscle, but also contains blood vessels and nerves. Additionally, the myocardium is associated with the fibrous skeleton of the heart. This is the framework of connective tissue that provides the origins and insertions for the cardiac muscle cells. Also, it helps electrically isolate the chambers of the heart from one another Endocardium: smooth glistening white sheet of simple squamous epithelium lining the internal spaces of the heart (i.e. the chambers) and is continuous with the endothelial lining of the blood vessels – smooth lining prevents activation of clotting cascade |
|
|
The heart chambers
|
2 upper chambers: the atria 2 lower chambers: the ventricles
Heart divided longitudinally by the interatrial and interventricular septa NB Towards the front of the interatrial septum there is a characteristic depression known as the fossa ovalis This represents the position of a previous opening between the two sides of the heart in the foetal stage of development This opening is known as the foramen ovale Prior to birth this opening permitted blood to be shunted directly from the right atrium into the left atrium, diverting blood from the foetus's non operational lungs |
|
|
The atria
|
Atria have thin, flaccid walls corresponding to their light workload
They do not need much muscle because they primarily serve as receptacles for the blood returning from the systemic and pulmonary circuits Most of this blood flows into the ventricles due to gravity They need only to contract to send a small amount of blood to the nearby ventricles |
|
|
The ventricles
|
The thick interventricular septum separates the left and right ventricles
The left ventricle is 2-4x as thick as the right ventricle because of its greater workload Also present in the ventricles are the papillary muscles. These protruding muscular pillars are connected to thin, white, fibrous connective tissue cords, the chordae tendineae, which in turn attach to the leaflets of their respective atrioventricular valves |
|
|
Function of the heart valves
|
Heart valves function to ensure a one-way flow of blood through the heart
The heart valves open and close passively because of pressure differences on either side of the valve When pressure is greater behind the valve, the leaflets are blown open and the blood flows through the valve. When pressure is greater in front of the valve, the leaflets snap shut and blood flow is stopped |
|
|
Valves close under pressure
|
AV valves:
the high pressure in the ventricle closes the valve Only opens when atrial pressure becomes greater than ventricular pressure Semi-lunar valves Close under very high pressure – the peak of arterial pressure. They have some backflow Form the boundary between the larger diameter of the ventricle and the smaller diameter of the artery – requires a high velocity of blood flow to get blood through these valves – hence need stronger connective tissue |
|
|
Stopping backflow into the atria
|
valves that prevent backflow from the ventricles into the atria - the 2 atrioventricular valves
The tricuspid valve is found between the right atrium and the right ventricle. It's given its name because it contains 3 valve flaps or cusps The valve between the left atrium and the left ventricle has 2 flaps and is thus known as the bicuspid valve. The bicuspid valve is also frequently referred to as the mitral valve Attached to the flaps of the AV valves are strings of collagen called chordae tendineae. These strings are also attached to papillary muscles that bulge from the ventricle floor |
|
|
The tricuspid and mitral valve
|
The tricuspid and mitral valve
The papillary muscles and chordae tendineae prevent the valve flaps from flipping upward into the atria – eversion of the valve Chordae tendineae are connective tissue and extend from edges of the valve to the papillary muscles – the myocardium of the ventricles |
|
|
Atrioventricular valves
|
As blood flows from the left atrium into the left ventricle, the mitral valve is open and the chordae tendineae are slack and the papillary muscles relaxed
As blood flows from the left ventricle into the aorta the mitral valve is closed and the chordae tendineae and papillary muscles are tensed - preventing the prolapse of the mitral valve and the backflow of blood from the left ventricle into the left atrium |
|
|
Semilunar valves
|
▪ prevent backflow from the aorta and pulmonary trunk into the left and right ventricles respectively
▪ 3 cup-like flaps that expand and cover the exits from the ventricles when they fill with blood ▪ the pulmonary semilunar valve prevents backflow from the pulmonary trunk into the right ventricle ▪ aortic semilunar valve prevents backflow from the aorta into the left ventricle ▪ no chordae tendineae and papillary muscles. Because of their structural design, they are less likely to experience any form of prolapse |
|
|
Semilunar valve function
As Ventricles contract and intraventricular pressure rises, blood is pushed up against semilunar valves, forcing them open. |
As ventricles relax and intracentricular pressure falls, blood flows back from arteries, filling the cusps of semilunar valves and forcing them close
|
|
|
Path of blood flow through the heart
|
For convenience - considered starting at right
Blood enters the right atrium via: Superior vena cavae Inferior vena cavae The coronary sinus Via AV valve (tricuspid valve) into Right Ventricle To Lungs via the pulmonary trunk vessel through the pulmonary valve Left and right pulmonary arteries to left and right lungs Oxygenation 4 pulmonary veins take blood to left atrium Into left ventricle via AV valve (bicuspid) From left ventricle into aorta via aortic (semi lunar) valve First branch of aorta - coronary arteries Aortic arch, thoracic aorta, abdominal aorta |
|
|
Heart sounds
|
Do not hear opening of valves – relatively slow process
Valve closure more sudden producing pressure differentials across the valve. Vibration of the valve travel through surrounding fluids and tissues in all directions across the chest. Best heard at surface at chest- but at different locations to the valve Four sounds in any cycle, although the first two are more prominent |
|
|
Heart sounds
|
Ventricles contract – closure of AV valves. Vibration low in pitch and of relatively long duration – ‘lub’ – First heart sound – Korotkoff sound
▪ 2nd heart sound – ‘dup’ – closure of semi lunar valves at the start of ventricular relaxation. Valve closure very fast – short vibration period. ▪ Can split sounds if aortic valve closes before pulmonary valve ▪ 3rd sound – blood entering relaxed ventricles through the AV valve – common in young people ▪ 4th sound – atrial contraction – heard just before the 1st sound |
|
|
Heart murmurs
|
Abnormal heart sounds, or murmurs, are associated with heart disease
▪ Blood flow through the valves should occur in a smooth fashion (laminar blood flow) ▪ if blood flow through a valve is turbulent, then an abnormal sound will be produced ▪ Turbulent blood flow will occur if the valve fails to fully open (stenotic valve) or if the valve fails to fully close (insufficient valve) ▪ A Stenotic Valve has an abnormally narrow opening that impedes the smooth, laminar flow of blood ▪ An Insufficient Valve (incompetent valve) is a leaky valve that allows blood to flow backwards (regurgitate) into the adjacent chamber |
|
|
Coronary Arteries
|
▪ Blood is supplied to the heart by its own vascular system – the coronary circulation
|
|
|
Arteries of the heart
|
▪ The aorta branches off into two main coronary arteries - branch off into smaller arteries, which supply oxygen-rich blood to the entire heart muscle.
▪ The right coronary artery supplies blood mainly to the right side of the heart. The right side of the heart is smaller because it pumps blood only to the lungs. ▪ The left coronary artery, which branches into the left anterior descending artery and the circumflex artery, supplies blood to the left side of the heart. The left side of the heart is larger and more muscular because it pumps blood to the rest of the body |
|
|
Coronary circulation
|
Coronary circulation essential as myocardium has greatest oxygen demand of all tissues
8 ml / 100 g of heart tissue per minute at rest Supply of blood = 1/20th of total output although 1/200th of body weight Coronary vessels deliver most blood when heart is relaxed Blood collected from left ventricle via cardiac veins that merge to form the coronary sinus. Empties into the upper section of right atrium The coronary sinus is created from the great cardiac vein; the middle cardiac vein and the small cardiac vein Blood collected from right side of heart is via anterior cardiac vein that empties into anterior part of right atrium |
|
|
Factors influencing coronary blood flow
|
▪ Demand from myocardium for oxygen. During exercise or stress additional oxygen is supplied by increased coronary blood flow. The change in blood flow is proportional to oxygen need. Intrinsic mechanism
▪ Neural mechanisms: parasympathetic stimulation ↓ heart rate – ↓ O2 consumption and ↓ coronary flow / sympathetic stimulation ↑ heart rate and myocardial contractility - ↑ O2 consumption and blood flow ▪ Aortic pressure: any ↑ in aortic pressure from contraction of heart muscle results in ↑ coronary blood flow |
|
|
The coronary circulation
|
▪ The coronary circulation exhibits collateral circulation and multiple anastomoses ▪ Having multiple routes for blood to reach certain areas provides a way to help ensure
the health of cardiac tissue ▪ If there are 2 vessels feeding an area and one is blocked, the other can still provide oxygen and nutrients to the cells in the area ▪ NB - end arteries. They are arteries that lack significant anastomoses or collateral circulation ▪ Blockage of coronary arteries can cause ischemia - a loss of blood flow ▪ Temporary and reversible ischemia produces a sense of pain known as angina pectoris ▪ Prolonged ischemia (perhaps due to a coronary blockage) can lead to myocardial cell death - in other words, a myocardial infarction |
|
|
Myocardial infarction
|
▪ When cholesterol plaque accumulates to the point of blocking the flow of blood through a coronary artery, the cardiac muscle tissue fed by the coronary artery beyond the point of the blockage is deprived of oxygen and nutrients
|
|
|
Cardiac Muscle
99% of cardiac muscle cells are the contractile cardiac muscle cells ▪ They generate the force that pumps blood through the systemic and pulmonary circuits ▪ The remaining 1% lack the elaborate sarcomeres and other contractile machinery and have a separate specialized function ▪ They are the autorhythmic cells of the heart |
▪ the cardiac muscle cell is the predominant cell type of the myocardium ▪ cardiac muscle cells are short, fat, branching and uninucleate compared with the
skeletal muscle cells which are long, skinny, non-branching and multinucleate ▪ striated muscle ▪ cardiac muscle cells are intricately linked to one another by structures called intercalated discs. ▪ intercalated discs have 2 components. They consist of gap junctions (which provide an electrical link between all cardiac muscle cells) and desmosomes (which provide a mechanical link between all cardiac muscle cells) ▪ the electrical and mechanical connection created by the intercalated discs allow the thousands of cardiac muscle cells to behave as if they were one giant cell |
|
|
▪ "Autorhythmic" literally equates to "self-rhythm"
|
▪ Autorhythmic cells set the rhythm of the heart without any input from any external organs, tissues, or signals. They account for the intrinsic control of the heart rate, i.e. the means by which the heart determines its own rate
▪ Autorhythmic cells have the ability to spontaneously depolarize to threshold and generate action potentials. (skeletal muscle cells that need acetylcholine released by motor neurons to generate the action potentials that precede contraction) |
|
|
Resting potentials..
|
▪ All cells have a resting potential: an electrical charge across the plasma membrane with the interior of the cell negative with respect to the exterior
▪ due to the unequal distribution of salts in the intracellular and extracellular fluids ▪ Potassium ions are more concentrated inside the cell, while sodium ions are higher in concentration outside. ▪ Left to themselves, these ion concentrations would tend to equalize out...BUT ▪ cell membrane itself is impermeable to ions like sodium and potassium. ▪ Instead, the movement of ions across the membrane is restricted to tiny pores, known as ion channels whose opening and closing is tightly controlled |
|
|
Resting potentials..
|
▪ At rest, the sodium channels are closed, but some potassium channels are open. Potassium ions therefore tend to move out of the cell down their concentration gradient (red arrow) and because they are positively charged, this makes the inside of the cell around 70-80 mV more negative than the outside
▪ The whole system is then roughly in balance, because the negativity inside tends to resist further efflux of potassium ions. ▪ There is, however, a very slight leakage of sodium ions into the cell. Over the long run, this is opposed by so-called sodium pumps — protein molecules in the membrane that use energy to push sodium ions out of the cell, in exchange for potassium ions moving in. ▪ Thesodium/potassiummovementproduces ▪ a concentration of Na+ outside the cell that is some 10 times greater than that inside the cell ▪ a concentration of K+ inside the cell some 20 times greater than that outside the cell. ▪ The concentrations of chloride ions (Cl-) and calcium io |
|
|
Depolarisation
|
▪ external stimuli reduce the charge across the plasma membrane ▪ facilitated diffusion of sodium into the cell reduces the resting
potential at that spot on the cell ▪ Na+ rushes into the cell. The sudden complete depolarization of the membrane opens up more of the voltage-gated sodium channels in adjacent portions of the membrane. ▪ In this way, a wave of depolarization sweeps along the cell. This is the action potential |
|
|
The refractory period
|
A second stimulus applied to a neuron (or muscle fibre) less than 0.001 second after the first will not trigger another impulse The membrane is depolarized and the neuron is in its refractory period Not until the -70 mv polarity is re-established (position C above) will the neuron be ready to fire again
|
|
|
Repolarization
|
▪ Repolarization is first established by the facilitated diffusion of potassium ions out of the cell. Only when the neuron is finally rested are the sodium ions that came in at each impulse actively transported back out of the cell
▪ Other kinds of ions, flowing through their own specialized channels, may contribute to the action potentials of nerve and muscle fibres. For example, calcium entry plays a part in the action potentials of heart muscle, and chloride flow is important in the electrical activity of skeletal muscle. |
|
|
Location of autorhythmic cells
|
▪ Masses of autorhythmic cells are found in several locations in the heart: ▪ Sinoatrial Node (SA node) - Adjacent to the Superior Vena Cava opening in the
right atrium ▪ Atrioventricular Node (AV node) - Near the right AV valve at the bottom of the interatrial septum ▪ Atrioventricular Bundle (AV bundle or Bundle of His) - Inferior interatrial septum ▪ Left & Right Bundle Branches - Interventricular septum ▪ Purkinje Fibers - Distributed throughout the right and left ventricle |
|
|
SA node
|
▪ Little strip of muscle – 3mm wide, 1,"", thick and 15 mm long at the connection of S VC to the right atrium
▪ Very small cells- 3-5 microns (rbc 7) ▪ No actin and no myosin ▪ Myocardial cells that don’t contract – they are continuous with myocardium ▪ Cells are extremely ‘leaky’ to Na+ - this is the stimulus for depolarisation – membrane potential of an atrial SA node cell = - 40 mv – less effort to achieve depolarisation ▪ Cells contain fast and slow Na+ channels – this is a factor in the length of contraction |
|
|
Conduction pathway
|
▪ SA node direct to muscle of right atrium
▪ Through inter atrial pathway to left atrium – Bachmanns bundle ▪ Then enters AV node at base of right atrium via anterior, middle and intra-nodal pathways ▪ AV node: located behind AV valve near opening of the coronary sinus – only way through to ventricles ▪ AV node has 2 types of fibres – transitional, penetrating (P) fibres) ▪ Av node slightly slows down the rate of conduction - delay of the electrical wave in the AV node allows the atria to finish contracting prior to the ventricles contracting, thus providing for an atrial kick ▪ Av Bundle/Bundle of His ▪ Purkinje fibres |
|
|
Heart rate
|
▪ Determined by intrinsic properties of SA node ▪ Altered by autonomic nervous system and blood borne hormones e.g. adrenaline,
thyroxine ▪ Autorhythmicity – ability of SA node to generate impulses in absence of external stimuli ▪ AV node has autorhythmicity 40-60 beats and rest of system discharges at 15-40 beats/minute ▪ If removed autonomic impact - normal neutral resting rate of 50 bpm. Need sympathetic system to get it up to 70bpm ▪ To slow heart, turn off sympathetic system ▪ Strong parasympathetic stimulation can stop the heart! E.g. vasovagal effect / valsalva manoeuvre |
|
|
The ECG
▪ an upward deflection on the ECG represents depolarisation moving towards the viewing electrode ▪ a downward deflection represents depolarisation moving away from the viewing electrode. |
▪ The Electrocardiograph (ECG) is clinically very useful, as it shows the electrical activity within the heart, simply by placing electrodes at various points on the body surface
▪ determine the state of the conducting system and of the myocardium itself, as damage to the myocardium alters the way the impulses travel through it |
|
|
PQRST
|
▪ The P wave represents atrial depolarisation- there is little muscle in the atrium so the deflection is small
▪ The Q wave represents depolarisation at the bundle of His; again, this is small as there is little muscle there ▪ The R wave represents the main spread of depolarisation, from the inside out, through the base of the ventricles. This involves large amounts of muscle so the deflection is large ▪ The S wave shows the subsequent depolarisation of the rest of the ventricles upwards from the base of the ventricles ▪ The T wave represents repolarisation of the myocardium after systole is complete. This is a relatively slow process- hence the smooth curved deflection |
|
|
Extrinsic Influences on Heart Rate
|
▪ The autonomic nervous system provides a large influence on the activity of the heart
▪ Increased activity of the sympathetic nervous system (the "fight or flight" branch of the ANS) increases both the rate and the force of heartbeat ▪ Increased activity of the parasympathetic nervous system (the "rest and digest" branch of the ANS) decreases heart rate but has little effect on the force of contraction |
|
|
Extrinsic Influences on Heart Rate
|
The medulla oblongata within the brain stem contains:
▪ The cardioacceleratory centre - source of the sympathetic output to the heart - to the SA node, AV node, and the bulk of the myocardium ▪ The cardioinhibitory centre - source of the parasympathetic output to the heart - project via cranial nerve 10 (the vagus nerve) to the SA and AV nodes ▪ There is a resting tonic level of sympathetic and parasympathetic input to the heart sympathetic nerves release noradrenaline parasympathetic nerves release acetylcholine ▪ the endocrine system plays a role as various hormones (e.g., adrenaline, thyroxine, glucagon) can exert an effect on the heart's rhythm) |
|
|
Some conduction problems
|
▪ Arrhythmia - an irregular heart rhythm
▪ Fibrillation - condition of rapid and out-of-phase contractions. In ventricular fibrillation, the depolarization and contraction of the ventricular muscle cells is not coordinated ▪ Ectopic Focus - An abnormal pacemaker. A region of the heart becomes hyperexcitable and generates impulses faster than the SA node. Can lead to premature ventricular contractions ▪ Heart Block - Any damage to the AV node. Interferes with transmission of impulses to the ventricles. Can vary in severity |
|
|
Circulatory system
|
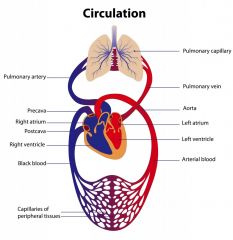
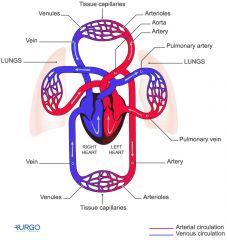
▪ On average, your body has about 5 litres of blood continually travelling through it by way of the circulatory system. The heart, the lungs, and the blood vessels work together to form the circle part of the circulatory system. The pumping of the heart forces the blood on its journey
▪ The body's circulatory system really has three distinct parts: pulmonary circulation, coronary circulation, and systemic circulation. Or, the lungs (pulmonary), the heart (coronary), and the rest of the system (systemic). Each part must be working independently in order for them to all work together |
|
|
The heart is a pump
|
• Blood is actually pumped through 2 separate circuits
• Pulmonary circuit: Runs between the heart and the gas exchange surfaces of the lungs • Systemic Circuit: Runs between the heart and the tissues of the rest of the body |
|
|
Blood vessels
|
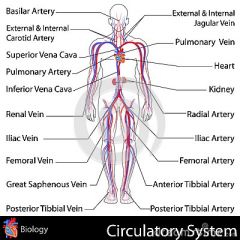
▪ Circuit of blood vessels / tubes
▪ Branching networks ▪ Blood carried away from heart in arteries ▪ Arteries branch to form smaller tubes – arterioles ▪ Arterioles lead into smaller networks – capillaries – at this level get exchange of materials between blood and body cells ▪ Capillaries merge to form venules ▪ Venules merge to form veins ▪ Venules and veins return blood to the heart |
|
|
Structure of blood vessels
|
▪ All except capillaries have same structure ▪ Tunica interna – single layer of flattened cells
▪ Supported by elastic tissue and connective fibres ▪ Tunica media: smooth muscle fibres ▪ supported by collagen and elastin fibres ▪ Tunica externa: elastin and collagen fibres ▪ Middle layer varies most across all vessels: absent in capillaries by near heart – made up elastin ▪ Smooth muscle layer innervated by sympathetic nervous system to aid contraction – muscle tissue laid down in rings around vessel - vasoconstriction |
|
|
Arteries
|
▪ Carry blood away from the heart
▪ Fast delivery ▪ Middle layer of artery wall – elastic fibres and circular layers of smooth muscle ▪ Fibres allow stretch and recoil ▪ Smooth muscle – contraction ▪ The stretch and recoil of arteries – pressure wave – a pulse ▪ Contraction of smooth muscle changes diameter of artery to reduce or increase blood flow – regulates distribution of blood |
|
|
Capillaries
|
▪ Only a few elastic fibres in the wall
▪ controllers of blood pressure ▪ Gatekeepers to capillary network: can be opened or closed depending on arteriole depending if smooth muscle allows blood through ▪ Arterioles respond to hormones, the sympathetic nervous system and local conditions minute by minute: modify blood pressure and blood flow |
|
|
Veins
|
▪ Capillaries merge to form venules – smallest veins
▪ Veins return blood to the heart ▪ Thinner walls of arteries ▪ Larger lumens ▪ Hold a large volume of blood – blood reservoirs holding 65% of blood ▪ Arteries13% ▪ Pulmonary circuit 9% ▪ Heart 7% ▪ Capillaries6% |
|
|
Returning blood to the heart
|
▪ The same amount of blood that left the heart must be returned to it ▪ No high pressure pump to help it ▪ In head and neck – gravity aids return ▪ Valves in veins prevent backflow of blood
▪ Contraction of skeletal muscle squeezes veins – pressure pushes blood past the valves ▪ Breathing causes pressure changes that move blood toward heart – blood moves to areas of lower pressure |
|
|
Systemic circuit blood arriving at the heart
|
▪ Blood from the systemic circuit is high in carbon dioxide and low in oxygen and will arrive in the right atrium from 3 vessels
▪ Superior vena cava - Drains head, torso, and upper arms ▪ Inferior vena cava - Drains abdomen, pelvis, and legs ▪ Coronary sinus - Drains the coronary circulation |
|
|
Systemic circuit blood leaving the heart
|
▪ blood leaves the heart through the aorta, goes to all the organs of the body through the systemic arteries, and then returns to the heart through the systemic veins
▪ Thus there are two circuits. Arteries always carry blood away from the heart and veins always carry blood toward the heart ▪ There are exceptions. The pulmonary arteries leaving the right ventricle for the lungs carry deoxygenated blood and the pulmonary veins carry oxygenated blood. ▪ If you are confused as to which way the blood flows through the heart, try this saying "When it leaves the right, it comes right back, but when it leaves the left, it's left." ▪ The blood does not have to travel as far when going from the heart to the lungs as it does from the heart to the toes – hence difference in ventricle size |
|
|
Pulmonary circuit blood arriving at the heart
|
▪ A right heart in the pulmonary circuit ▪ In the pulmonary circuit, blood leaves the heart through the pulmonary arteries,
goes to the lungs, and returns to the heart through the pulmonary veins ▪ Blood from the pulmonary circuit is low in carbon dioxide and high in oxygen and arrives at the left atrium from 4 blood vessels - the 4 pulmonary veins: ▪ right superior ▪ right inferior ▪ left superior ▪ left inferior pulmonary veins |
|
|
The aorta
|
▪ The aorta is the largest artery in the body ▪ It arises from the left ventricle of the heart, forms an arch, then extends
down to the abdomen where it branches off into two smaller arteries ▪ Carries and distributes oxygen rich blood to all arteries ▪ Most major arteries branch off from the aorta, with the exception of the main pulmonary artery ▪ The aorta is the largest artery in the body ▪ It arises from the left ventricle of the heart, forms an arch, then extends down to the abdomen where it branches off into two smaller arteries ▪ Carries and distributes oxygen rich blood to all arteries ▪ Most major arteries branch off from the aorta, with the exception of the main pulmonary artery |
|
|
The vena cavae
|
▪ The vena cavae are the two largest veins in the body
▪ They carry de-oxygenated blood from various regions of the body to the right atrium. The superior vena cava is formed by the joining of the brachiocephalic veins. The inferior vena cavae is formed by the joining of the common iliac veins ▪ Superior Vena Cava: Brings de-oxygenated blood from the head, neck, arm and chest regions of the body to the right atrium ▪ Inferior Vena Cava: Brings de-oxygenated blood from the lower body regions to the right atrium |
|
|
|
|
|
|
|
|

|
|
|
nil
|

