![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
PTH Effects:
Bone Kidney |
Bone: Calcium and PO4 resorption (release)
Kidney: Calcium reabsorption; PO4 excretion; 25 Vit D (inactive)-->1,25 Vit D (Active) |
|
|
_________ triggers the release of PTH.
|
Decrease in serum calcium
|
|
|
1,25 Vitamin D Effects:
Intestines Kidney |
Intestines: calcium and PO4 reabsorption from gut
Kidney: PO4 reabsorption |
|
|
The conversion of 25 Vit D to 1,25 Vit D is INHIBITED by ________.
|
HIGH PO4 concentrations (thus preventing Ca and PO4 reabsorption from gut then PTH release)
|
|
|
Where are calcium sensing receptors located?
|
Parathyroid Gland (PTH secretion)
Loop of Henle (Ca secretion from renal tubules) |
|
|
What is the 'setpoint' for calcium?
|
8.5
|
|
|
What are the main causes of hypoparathyroidism?
What lab values correlate with each cause? When would hungry bone be present? |
-No parathyroid gland (low PTH; low Ca and High/LOW PO4; IF LOW PO4-->HUNGRY BONE)
-No PTH production/secretion (low; PTH; low Ca, High PO4) -PTH resistance (receptor level; HIGH PTH; low Ca and high PO4) |
|
|
DiGeorge Syndrome
|
Congenital (no Parathyroid Gland)
|
|
|
Most common disorder of parathyroid gland?
|
Irradiation of neck (thyroid usually)
|
|
|
A manipulation of blood supply (to the thyroid region) could result in _____.
|
Transient hypoparathyroidism
|
|
|
What is hungry bone syndrome?
|
Inc'd rate of bone resorption as a result of hypoparathyroidism
When you do a thyroidectomy, bone wants to remineralize, and HOGS up all serum Ca, PO4, Mg |
|
|
What is the effect of a transient activating Ca-SR antibody?
|
Not destructive, but results in decreased PTH secretion
|
|
|
Mutation in preproPTH results in _______.
|
Abnormal PTH synthesis (hypopara)
|
|
|
What is the effect of an activating mutation to CaSR on the calcium set point?
|
Lower set point (requires lower Ca2+ concentration to activate)
|
|
|
Mutation in GNAS1 results in ______.
|
PTH Resistance (receptors don't bind PTH)-->hypopara
|
|
|
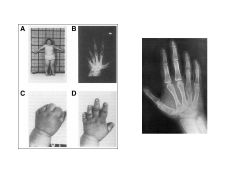
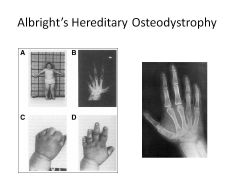
Albright's Hereditary Osteodystrophy:
Symptoms Cause |
Round facies
Short stature Short fourth metacarpals obesity Subcut calcifications Developmental delay Cause: PTH resistance (maternal transmission) (If paternally transmitted would be pseudopseudohypoparathyroidism) |
|
|
Vitamin D:
Sources |
Sunlight (7-dehydrocholesterol-->Cholecalciferol--Vit D3)
Diet: D3, D2 |
|
|
Effect of LOW Vitamin D on:
GI Parathyroid Gland Bone Kidney |
GI: decreased Ca and PO4 absorption
Parathy: Increase PTH Bone: increase resorption Kidney: increase Ca resorption |
|
|
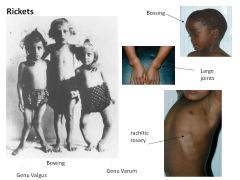
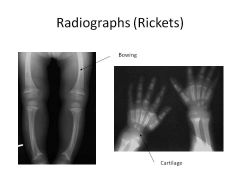
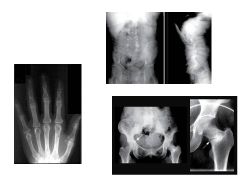
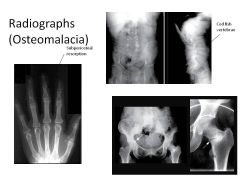
How does low vitamin D result in Osteomalacia/Rickets?
Osteomalacia vs Rickets? |
Bone growth and mineralization requires Ca and PO4
Low Vit D-->Low Ca and PO4 Osteomalacia: impaired mineralization of bone matrix (ADULTS) Rickets: Deficient mineralization of growth plate cartilage (CHILDREN); chondrocytes get resorbed! |
|
|
Extraskeletal manifestations of Vit D deficiency.
|
Delay of motor milestones
Dec'd muscle tone Wasting Proximal mm weakness Waddling gait Seizures Hypoplasia of dental enamel Dentin defects (abscess and decay) |
|
|
Vitamin D Deficiency:
Causes |
-Deficient uptake, absorption (diet, sun exposure)
-Defective 25-hydroxylation (liver issue; anticonvulsants) -Defective 1-alpha-25-hyrdoxylation (hypopara, renal failure, enzyme defect) -Vitamin D Receptor defect (VDDR-2) |
|
|
1-alpha hydroxylase deficiency results in ________.
|
Defect in D25-->D1,25
|
|
|
What is Vitamin D-Dependent Rickets Type II?
|
Hereditary Vitamin D-resistant Rickets (mutation to vit D receptor)
More alopecia-->more severe disease |
|
|
What type of vitamin D is present in PO supplements? Requirement?
|
D2 (cholecalciferol)/D3 (ergocalciferol)
Both require hepatic hydroxylation to calcitriol (need functional liver!) D3 (ergocalciferol) is more potent; used in Rickets and osteomalacia |
|
|
What Vitamin D supplement is best for a patient with renal failure?
|
1,25-OHD (Calcitriol)
Don't need a liver either! |
|
|
A patient presents with signs of osteomalacia/Rickets.
What tests do you run to find the cause? |
Measure 25-OH D
If low-->Vit D Deficiency If normal, measure 1,25-OH D If 1,25-OH D Low-->defect in 1-alpha hydroxylase (can't convert 25-->1,25) If high-->dysfn of Vit D Receptor (have working enzyme) |
|
|
Extravascular Deposits of Calcium:
Causes |
Hyperphosphatemia (renal failure, excess intake)
Osteoblastic mets (BrCa, ProsCa) Acute pancreatitis Hungry bone post-parathyroidectomy |
|
|
Intravascular Complexing of Calcium:
Causes |
Chelators (Citrate, Lactate)--bind Ca and ionized levels drop
Alkalosis |
|
|
Effect of magnesium levels on PTH.
|
Hypomagnesemia-->PTH resistance, reduced secretion (assocd w/malabsorption, EtOH, diuretics, etc)
Hypermanesemia: Suppress PTH secretion |
|
|
Hypocalcemia:
Causes Symptoms |
Hypoparathyroidism
Vitamin D Def Low of Calcium from circulation Disorders of Mg Syx: -Tetany, twitching, seizures -CV: prolonged QT, arrythmia -Chovstek's Sign -Trousseau's Sign |
|
|
What is Chovstek's sign and what does it indicate?
|
Tap facial nerve-->muscle contracts
HYPOCALCEMIA |
|
|
What is Trousseau's sign and what does it indicate?
|
Put on BP cuff-->forearm contracts
HYPOCALCEMIA |
|
|
Total Calcium is a measure of _____.
|
Calcium bound to protein (albumin) -45%
Calcium bound to anion (phosphate, citrate)-15% Free or ionized calcium-40% |
|
|
In a critically ill patient with hypocalcemia, what test would you order?
|
IONIZED calcium (calcium-albumin complex altered by pH; acidosis reduces binding, alkalosis increases binding)
|
|
|
|
|
|

|
|

|
|
|

|
|
|
|
|

