![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
What is diabetes mellitus?
Cardinal feature? |
Syndrome resulting from absolute or relative deficiency of insulin
Cardinal feature: Hyperglycemia |
|
|
What is the criteria for the diagnosis of DM?
Why were these cutoffs selected? |
HgA1c > 6.5%
OR Plasma glucose > 200 at any time OR Fasting glucose > 126 (more than 8 hours since last meal) OR Plasma >200 after 75gm of glucose in oral glucose tolerance test (don't want to make the diagnosis on just one number) These cutoffs are the point at which the microvascular disease associated with diabetes begins. |
|
|
What is a Schiff base?
What conditions affect its number? |
HgA1c = Glucose + Hg -->(FAST) Schiff Base (reversible) -->(SLOW) HbA1c (stable)
Affected by mutations to glucose (increase or decrease) |
|
|
What changes affect the number of stable HgA1c molecules?
|
HgA1c = Glucose + Hg -->(FAST) Schiff Base (reversible) -->(SLOW) HbA1c (stable)
Decreased by shortened lifespan of RBC's (lower Hg available)--such as a hemolytic or iron deficiency anemias |
|
|
Diabetic retinopathy is associated with elevated levels of _____.
|
HgA1c
|
|
|
Describe the different types of Diabetes Mellitus.
|
IA: Immune-mediated
IB: insulin-deficient, not autoimmune II: Insulin resistance and insulin secretory deficiency Gestational Other (MODY, lipoatrophic, type A insulin resistant, endocrinopathies, drugs) |
|
|
Juvenile Onset Diabetes is Type ___ Diabetes.
|
Type I
has a broad range of onset, peaks at adolescence (can get it in 20's!) 50% onset before 20, other half after 20 |
|
|
Insulin is destroyed by autoimmune processes in this type of diabetes.
|
Type I
|
|
|
What are the long-term complications in diabetes?
|
Amputation (40 fold risk)
End Stage Renal Dz (25 fold) Blindness (20 fold) MI Stroke |
|
|
Long-term complications of diabetes are associated with ______.
|
Blood glucose levels
|
|
|
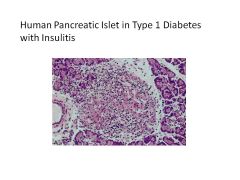
What pancreatic cells are affected by Type I Diabetes?
|
Beta Cells (no insulin produced)
Alpha Cells normal (have glucagon) |
|
|
Do diabetic patients need insulin in fasting states, i.e., sleeping?
|
Yes, bc endogenous glucose is formed.
|
|
|
Why do diabetic patients become hyperglycemia in a fed state?
What can this result in? |
1) No glucose uptake by tissues
2) No inhibition of gluconeogenesis or glycogenolysis (liver keeps pumping out glucose) Severe insulin deficiency results in breakdown of FA's and creation of Ketone Bodies leading to KETOACIDOSIS (only get ketoacidosis if have severely low insulin) |
|
|
Type I Diabetes is most prevalent in these regions.
Why might this be? |
Western Europe (FINLAND!)
May be due to environmental factors (Viruses, beta cell toxins--n-nitroso cmpds, vacor) |
|
|
What other autoimmune disorders do patients with DM present with?
|
Celiac
Graves' Addison's Suggests that Type I is an autoimmune process |
|
|
Mutations to HLA DR3/4 is a major risk factor for ________.
|
Type I Diabetes
Likely other genetic loci involved |
|
|
In Type I Diabetes, genetic predisposition and _________ may lead to an autoimmune attack, thus causing ____-cell destruction.
|
Environmental Insult (Infection, molecular mimicry and/or damage to beta cells)
Beta-cell destruction |
|
|
The progression of Type I Diabetes is correlated with _____.
|
Presence of Auto-Ab's
(Stratified into speed of progression based on level of Auto-Ab's) |
|
|
Effects of DM Type I treatment with CD3 monoclonal antibodies.
|
Monoclonal Ab's against CD3 suppresses immune response
Preserve ability to secrete insulin DM Type I develops anyway DELAYS THE PROCESS! (Note: before this cephalosporin was used to inhibit immune system, but side effects to severe) |
|
|
Effects of pancreatic islet transplantation in Type I Diabetes.
|
Can produce insulin for a few years
Beta cells die out (limited lifespan) DM Type I resumes |
|
|
DM Type II becomes more prevalent with _____ and _____.
|
Age and Obesity
|
|
|
HgA1c is a measure of _______.
|
Average blood sugar
|
|
|
Do patients with Type II DM exhibit a biphasic release of insulin?
|
Not really, may have an initial small release of insulin, and then a huge prolonged release of insulin (can result in hypoglycemia)
|
|
|
What physiologic defects are associated with Type II DM?
|
Beta Cell Secretory Defect
Insulin Resistance (Probably requires both of these defects) |
|
|
____ insulin secretion is a risk factor for Type II DM.
|
Low
|
|
|
___ insulin resistance is a risk factor for Type II DM.
|
High
|
|
|
Which diabetes exhibits the most risk for genetically inheriting the disease?
|
DM Type II
|
|
|
Mature Onset Diabetes of the Young:
Cause Symptoms Treatment |
Autosomal Dominant Inheritance
Onsets in childhood/early adulthood TYPE II (no autoimmunity) Can be treated with oral meds to begin with (treatment depends on inherited genes--genotype defines phenotype and treatment) |
|
|
Common forms of diabetes result from the effect of ____________.
|
multiple mutated genes
Single gene defects cause <5% of DM |
|
|
In type ____ diabetes, there is a gradual decline in beta cell function. Approximately 10 years later, blood glucose levels lead to a diagnosis.
|
TYPE II
|
|
|
Type I vs Type II:
Which has a greater number of active beta cells? |
Type II
|
|
|
What defines gestational diabetes?
Possible causes? |
COH intolerance with onset or first recognition during pregnancy
This can affect the fetus!!! Dx: Oral glucose tolerance test Causes: Placental insulin degradation Hormones inducing insulin resistance (hCS, cortisol, PG, PL) |
|
|
What are the criteria for prediabetes?
|
Fasting Glucose: 100-125
2-hour postload glucose: 140-199 Inc'd HbA1c: 5.7-6.4% |
|
|
_________ complications are higher in patients in a pre-diabetes state.
|
MACROvascular (cardiovascular)
pre-diabetes = impaired glucose tolerance |
|
|
What are the clinical features of metabolic syndrome?
|
3 out of 5:
Central Obesity Impaired Glucose Tolerance High TGs Low HDL-C HTN (may also be hypercoag, hyperlipid, inflamm vasculopathy, endothelial dysfn) |
|
|
|

