![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
what are the 5 signs of inflammation |
redness swelling pain heat loss of function |
|
|
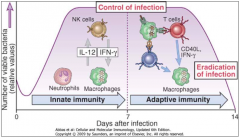
in what order to acute and chronic immune responses and inflammatory responses occur |
acute then chronic |
|
|
is inflammation the normal response to bacterial infection? |
|
|
|
give an example of an infection which has both an acute and chronic immune repsonse |
TB |
|
|
what is the resolution of an immune response |
it is the ability to eliminate pathogens (through what ever means) |
|
|
give 3 potential problems with can occur with the normal immune response |
-innocent by-standers (innate just "bombs" the whole area) -non-resolution -self-recognition and attack |
|
|
as part of the incorrect response to infection is autoimmunity, what potential problem can occur and when does this problem occur |
chronic inflammation this occurs as part of the adaptive immunity |
|
|
define autoimmunity |
loss of immunological tolerance to self |
|
|
as many as how many people have autoimmunity disease or other |
5% we all have the potential for it |
|
|
through what mechanisms can autoimmunity work |
-dysfunction in tolerance -presentation of self-antigens -molecular mimicry -loss of regulatory mechanisms |
|
|
what stops everyone from getting autoimmune diseases |
the immune system has regulatory checks |
|
|
what is tolerance |
the unresponsiveness to self even tho you have the capacity to do so
tolerance is when “you’ve decided not to attack something but tolerate it instead…obvs |
|
|
are the mechanisms of autoimmunity slower or faster than normal immune reactions |
slower |
|
|
what are the factors affecting the mechanisms of autoimmunity |
genetic and environmental |
|
|
does the course of an autoimmune disease continue as normal normally, or does it usually encounter problems? |
the course of the autoimmune disease does not continue on a normal path and can remit and relapse
remitx --> stop relapse --> go back? |
|
|
how many stimuli does the immune system usually need before it "overreacts" as part of the immune response |
2 |
|
|
give examples of organ specific autoimmune disease |
Myasthenia Gravis, Thyroiditis, vitiligo, type1 diabetes, autoimmune hepatitis, pernicious anaemia, Addison’s disease, psoriasis |
|
|
give examples of non-organ specific autoimmune disease |
Rheumatoid Arthritis (IgG), SLE (dsDNA), systemic sclerosis |
|
|
there are elevated levels of what type of cell in the synoviums of individuals with RA |
WBCs |
|
|
in the pannus of an individual with RA, what are the major and minor cell types present |
major cell types: T lymphocytes Macrophages
minor cell types: fibroblasts plasma cells endothelium dendritic cells |
|
|
what are the major cell types present in the synovial fluid of individuals with RA |
neutrophils |
|
|
what is an autoantibody |
An autoantibody is an antibody produced by the immune systemthat is directed against one or more of the individual's own proteins |
|
|
what are the 2 autoantibodies in RA |
Rheumatoid Factor (RF) Anti-CCP antibodies
|
|
|
what does the CCP stand for in anti-CCP |
cyclic citrullinated peptide |
|
|
what does the citrulline in anti-CCPs do in a person with RA |
it binds to the place where arginine usually is and replaces it |
|
|
RF binds to what immunoglobulin |
IgG |
|
|
on what part of the IgG does the RF bind to |
Fc portion of the IgG |
|
|
explain how environmental factors such as smoking or a gut micro biome can lead to arthritis and RA |
the environmental factors (e.g. smoking or gut microbiome) lead to altered post transcriptional regulation, this leads to self protein citrullination which then leads to loss of tolerance which subsequently leads to a transition to arthritis |
|
|
what does DMARD stand for |
disease modifying anti-rheumatic drugs |
|
|
what is the main DMARD used for treating RA |
methotrexate |
|
|
are combinations of different DMARDs better or is it better to use one at a time in isolation |
combinations have been found to work better |
|
|
under normal circumstances what happens when an inflammatory cytokine binds to a cytokine receptor on a cell surface |
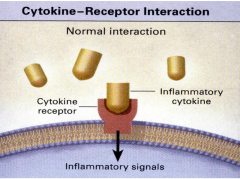
inflammatory signals are given into the cell |
|
|
what are biologic agents |
Drugs such as monoclonal antibodies, receptors or peptides which have been developed rationally by targeting processes important in disease pathogenesis: Eg Cytokines, T cells, B cells |
|
|
in RA TNF-α is inhibited, what effect does this have? |
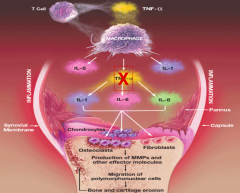
|
|
|
what methods can be used to "neutralise cytokines" so that they do not 'secrete' inflammatory signals into the cell and what is the method of action of each of these |
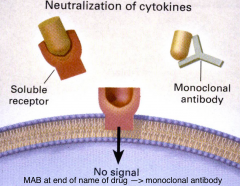
-a soluble receptor can be used to bind to the cytokine and prevents the cytokine from binding to the cytokine receptor -a monoclonal antibody can also be used, it has a similar means of action |
|
|
if a drug ends in 'MAB' then what does this mean |
it is a monoclonal antibody |
|
|
give an example of a soluble TNF -receptor to treat RA |
Enbrel (Etanercept) |
|
|
what does TNF maintain in TB |
it maintain TB granulomas |
|
|
if a drug has ib at the end of it what does that mean |
it has small molecules |

