![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
|
Control of renin release |
1) Decreased afferent arteriolar perfusion pressure --> stimulates release 2) B1 adrenergic receptors --> stimulates release 3) Decrease salt delivery to macula densa (distal tubule) --> stimultes release 4) Angiotensin II --> direct feedback inhibition |
|
|
What happens when there is too much NaCl flowing by the macula densa? |
Adenosine is released --> constriction of afferent arteriole --> decreased GFR Renin reduction will also be decreased (mostly a systemic effect) |
|
|
RAA Axis |
1) Renin converts angiotensinogen to ang I (rate controlling step is produciton/release of renin) 2) Ang I --> Ang II via ACE 3) Angiotensin II stimulates aldosterone secretion --> leads to increased sodium and water retention + increased preload 4) Angiotensin II also stimulates constriction of vascular smooth muscle --> increased afterload |
|
|
What happens if you continuously infuse angiotensin II? |
Blood pressure will continue to increase up until a certain point -- ang II will feedback negatively on renin and cause the blood pressure to plateau/decrease |
|
|
What happens if there is a decrease in blood volume or blood pressure? |
1) Juxtaglomerular cells of kidneys sense the decrease in blood pressure 2) Secretion of renin --> RAA axis 3) Angiotensin II leads to vasoconstriction of arteries which causes an increase in BP 4) Ang II also stimulates aldosterone secretion (along with increased K+ in ECF) 5) Aldosterone leads to increased Na + water reabsorption in the kidney and increased secretion of K+/H+ ions into urine --> inc blood volume --> inc blood pressure |
|
|
Stimuli that indicate decrease in blood volume/pressure? |
Dehydration, Na+ deficiency, or hemorrhage |
|
|
Glomerular effects of angiotensin II |
-Ang II mediates vasoconstriction of the efferent arteriole -This helps maintain adequate intraglomerular pressure for transcapillary glomerular perfusion |
|
|
Proximal tubular effects of angiotensin II |
-Causes constriction of efferent arteriole -Leads to increased glomerular blood pressure and filtration and reduces BP in peritubular capillary -Reduces resistance to tubular reabsorption -Tubular reabsorption increases (increases proximal tubular Na+ absorption)e -Urine volume is less but concentration is high |
|
|
Acute and chronic effects of angiotensin II systemically |
-Sympathetic nervous system activation -Blood vessel vasoconstriction, remodeling, endothelin release, atherosclerosis -Heart hypertrophy, LV remodeling, fibrosis -Aldosterone secretion -Kidney: sodium retention, glomerular filtration, proteinuria |
|
|
What is cleaved to go from Ang I --> Ang II? |
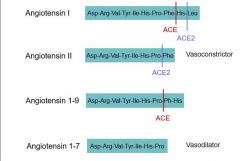
ACE removes His-Leu residue from the end of Ang I |
|
|
Where can ACE2 cleave? |
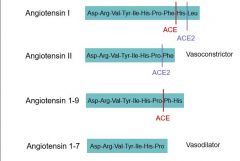
-ACE2 will cleave just the Leu residue off of Ang I which forms Ang 1-9 -ACE2 will cleave just the Phe residue off of Ang II which forms Ang 1-7 |
|
|
what does ACE do to Ang 1-9? |
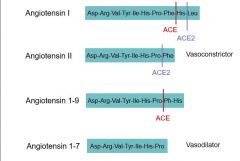
Cleaves a Ph-His residue off to form Ang 1-7 (vasodilator) |
|
|
Effects of angiotensin II? Ang 1-7? |
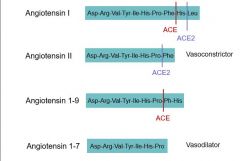
Ang II = vasoconstrictor Ang 1-7 = vasodilator (main product of ACE2) |
|
|
Effects of angiotensin II vs angiotensin 1-7 |
-Ang II binds to AT1 receptor --> vasoconstriction, endothelial dysfunction, proliferation/hypertrophy, fibrosis, atherosclerosis, thrombosis, arrhythmogenesis -Ang 1-7 binds to Mas receptor --> vasodilation, increased endothelial function, antiproliferation, decreased hypertrophy, dec fibrosis, dec thrombosis, antiarrhythmic |
|
|
Inhibitors of the RAAS System |
-Renin inhibitors inhibit conversion of Angiotensinogen --> Ang I (ex - aliskiren) -ACE inhibitors inhibit conversion of Ang I to Ang II (as well as the breakdown of bradykinin) -ARBs inhibit angiotensin II binding to AT1 |
|
|
ARB effects on AT1 vs AT2 receptors |
-AT1 receptors are inhibited by ARBs - this inhibits: vasoconstriction, SNS activation, increased aldosterone, increased vasopression, increased oxid stress, negative feedback for renin release -AT2 receptors are stimulated by ARBs - this stimulates vasodilation, apoptosis, antiproliferation, increased bradykinin, NO release |
|
|
Effect locations for drugs that block the RAAS |
-Renin blockers/impaired release of renin -ACE inhibitors -ARBs -Impaired aldosterone metabolism -Aldosterone receptor blockers -Sodium channel blockers (block reuptake induced by aldosterone) |
|
|
Location of aldosterone receptors |
-Kidneys -Brain -Arteries -Heart |
|
|
Why do ACE inhibitors cause cough? |
Decreased breakdown of bradykinin, which can lead to cough reflex |
|
|
What does aldosterone blockade do to urinary excretion of albumin? |
Aldosterone blockade decreases urinary albumin excretion rate (decreases proteinuria) |
|
|
Aldosterone blockade + cardiac mortality? |
Decreased cardiac mortality compared to placebo |
|
|
Type IV renal tubular acidosis |
-Hyperkalemic, hyperchloremic, metabolic acidosis -Not a tubular defect -Caused by aldosterone resistance or deficiency - most often present in cases of diabetic nephropathy or interstitial nephritis with mild/moderate renal insufficiency -Relative hypoaldosteronism leads to impaired secretion of K+ and H+ by collecting tubule, causing hyperkalemia + acidosis -Hyperkalemia impairs proximal tubular production of ammonia - urine pH is appropriately low but the amount of buffer (NH4+) is reduced |
|
|
Causes of hypokalemia |
-Decreased intake -Shift into cells: metabolic alkalosis, insulin -Renal loss: excess aldosterone, diuretics, renal tubular acidosis, Batter's syndrome, hypomagnesemia |
|
|
Causes of hyperkalemia |
-Decreased excretion: renal failure, aldosterone resistance, aldosterone deficiency -Shift out of cells: metabolic acidosis, digoxin, beta blockers, lack of insulin |
|
|
How does hypo/hyperkalemia affect RMP of cells? |
If you are hyperkalemic, less K+ will come out of cells (hypopolarization) If you are hypokalemic, more K+ will leave cells (hyperpolarization) |
|
|
How does hypo/hypercalcemia affect RMP of cells? |
Hypercalcemia = more depolarized Hypocalemia = more hyperpolarized |
|
|
What happens if you have hypocalcemia + hyperkalemia? |
Your resting membrane potential and threshold potential are very close --> cells are extremely easy to excite |
|
|
To distinguish primary aldosterone deficiency from other causes of hyperkalemia, get a ____ |
plasma renin activity level |
|
|
To distinguish renal from GI losses as a cause of hypokalemia, use the _____ |
Transtubular K+ gradient (TTK): TTK = [K+]urine x osmolality(blood)/[K+] blood x osmolality(urine) TTK <4 in presence of hypokalemia, >6 in presence of hyperkalemia |

