![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
What are the three most common types of stroke (in order of rate of occurrence)?
|
1) Ischemic
2) Intracerebral Hemorrhage 3) Subarachnoid Hemorrhage |
|
|
Fatality rate for Intracranial Hemorrhage? Recovery rate?
|
40% mortality rate
20% recovery (with functional independence) |
|
|
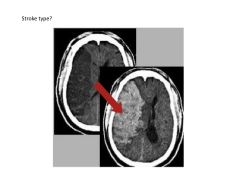
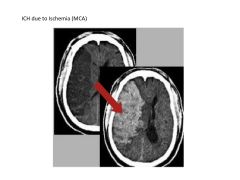
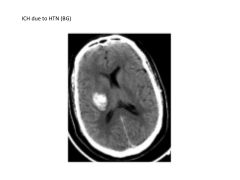
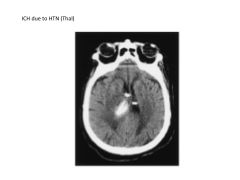
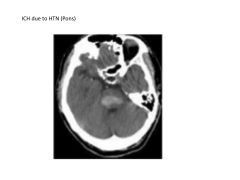
What are the two leading causes of intracranial hemorrhage?
|
1) HTN: combination of lipid deposition, atherosclerosis, necrosis
2) Cerebral Amyloid Angiopathy (CAA): dposition of amyloid-beta peptide and degenerative changes in vasculature |
|
|
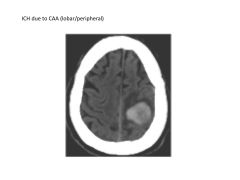
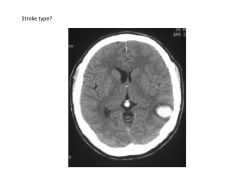
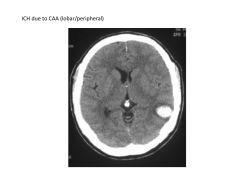
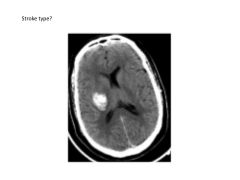
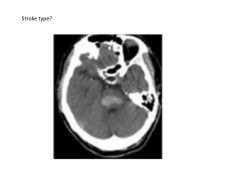
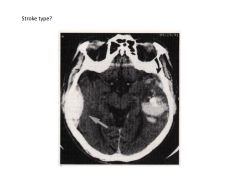
What types of stroke are associated with cerebral amyloid angiopathy? Brain regions affected?
|
sporadic (lobar/peripheral) ICH in elderly (not fixable)
|
|

|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|

|
|
|
|
|
|
What is the clinical presentation of a patient with intracranial hemorrhage?
|
Often elevated BP (>150/90)
Sudden onset with gradual evolution 50% report hemorrhage One-time event |
|
|
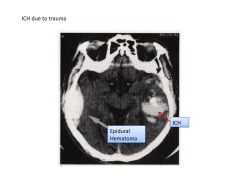
Imaging preference for ICH?
|
CT: fast, sensitive to acute blood, cheap
|
|
|
Treatment for patient with ICH if taking warfarin?
|
Anticoagulant reversal via FPP, vit k, or protrhombin complex (2,7,9,10)
|
|
|
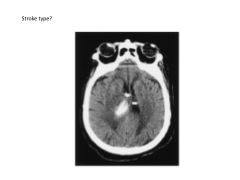
Mortality rate for subarachnoid hemorrhage?
Presenting symptoms? |
25-30% mortality
Sx: Worst headache of life (hit by lightning, 2x4, brick); sudden onset May be accompanied by nausea, vomiting, seizure, change in level of consciousness |
|
|
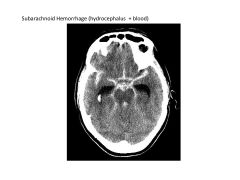
If a patient presented with subarachnoid hemorrhage, what evaluations would you perform?
|
Evaluate for hydrocephalus
Evaluate intracranial vasculature to prevent rerupture |
|
|
Nimodipine: mechanism, use
|
calcium channel blocker, used in pts with subarachnoid hemorrhage because of neuroprotective (unspecified) effects
|
|
|
What risk does vasospasm pose to patients with subarachnoid hemorrhages?
How can it be monitored? When is it more likely to occur? How can it be treated? |
Leads to secondary ischemic injury and stroke (as high as 40%)
Peaks between day 3-13 post rupture; pts monitored with transcranial doppler evaluation of blood flow through intracerebral vessels Occurs most often if thick clots seen on CT Tx: hemodynamic augmentation, euvolemia (maintain body fluids), HTN Or intra-arterial tx: Vasodilators (ca2+ ch blockers) Angioplasty |
|

|
|

