![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
What are the layers of the epidermis? (In order)
|
Californians Like Girls in String Bikinis
Striatum Corneum Lucidum Granulosum Spinosum Basalis |
|
|
Where are blood vessels located in the skin?
|
BVs in dermis, none in epidermis (gets nutrition by diffusion)
|
|
|
Zona occludens:
Role |
tight junction--prevents diffusion across paracellular space (composed of claudins and occludins)
|
|
|
Zona adherens:
Role |
Intermediate jn--surounds perimeter below zona occludens; cadherins connect to actin
|
|
|
Macula adherens:
Role |
Desomosome; small, discrete sites of attachment; cadherins connect to intermediate filaments
|
|
|
Pemphigus vulgaris:
Pathophys |
Autoantibodies to DESMOSOME (MACULA ADHERENS)
|
|
|
Hemidesmosome:
Role |
COnnects cells to underlying ECM
|
|
|
Bullous pemphigoid:
Pathophys |
Autoantibodies to HEMIDESMOSOME
|
|
|
Describe the steps of leukocyte extravasation.
Include the adhesion molecules and cytokines needed. |
1. Rolling--E-selectin, P-selectin
2. Tight binding: ICAM-1 3. Diapedesis (leukocyte travels between endothelial cells and exits BV)--PECAM-1 4. Migration--leukocyte travels through interstitium to site of injury, guided by chemotactic signals--CILK: C5a, IL-8, LTB4, Kallikrein |
|
|
What are the acute phase cytokines?
|
IL-1
IL-6 TNF-alpha |
|
|
Which of the following joins only cells of the same type and does not attach cells to the basement membrane?
Hemidesmosome Cadherin Integrin ICAM-1 |
Cadherin
|
|
|
What is the unhappy triad?
|
Force from lateral side injuring:
MCL ACL Lateral meniscus |
|
|
ACL vs PCL:
Attachment |
ACL: Anterior tibia
PCL: Posterior tibia |
|
|
Pudendal nerve:
Innervation |
Saddle region (block this area to relieve pain of delivery)
|
|
|
Where are lumbar punctures performed?
|
Between L3 and L4 (iliac crest)
|
|
|
Rotator cuff:
Components and their actions Which component is most commonly injuyed? |
SItS (small t for teres minor :))
Supraspinatus--abducts arm initial 10 degrees; most commonly injured Infraspinatus--laterally rotates arm (pitching injury) Teres minor--adducts and laterally rotates arm Subscapularis: medially rotates and adducts arm |
|
|
Which muscles of rotator cuff:
Initial 15 degrees of arm abduction |
Supraspinatus
|
|
|
Which muscles of rotator cuff:
Lateral rotation of the arm |
Infraspinatus
Teres minor |
|
|
Which muscles of rotator cuff:
Medial rotation of the arm |
Subscapularis
|
|
|
Where does new bone formation take place in growing long bones?
|
Epiphyseal plate
|
|
|
A football plays who was kicked in the leg suffers from a damaged medial meniscus.
What else is likely to have been damaged? |
ACL
MCL Lateral meniscus (UNHAPPY TRIAD) |
|
|
What is the difference between a dislocated and separated shoulder?
|
Dislocated--head of humerus rotates out of glenoid cavitiy
Separated--clavicle separates from acromion and coracoid process of scapula |
|
|
What structure can be damaged in anterior shoulder dislocation?
How would you test for this? |
Axillary nerve damage--test sensation over deltoid
Supraspinatus tendon |
|
|
Lateral vs Medial epicondylitis:
Pathophys |
Lateral epicondylitis: tennis elbow
Medial epicondylitis: golf elbow Both are degenerative injuries due to repeated use; leads to tiny tears in tendons and muscles. May be inflammatory. |
|
Label
|
|
|
|
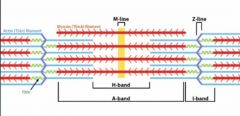
Type 1 vs Type 2 Muscle fibers
|
One slow red ox!
Type 1: Slow twitch, red fibers due to inc'd mitochondria and myoglobin concentration (inc'd ox-phos)-->sustained contractions Type 2: Fast twitch, white fibers due to dec'd mitochondria and myoglobin concentrations (inc'd anerobic glycolysis); ex: weight training |
|
|
Endochondrial vs Membranous FR3Ossification
|
Endochondral: Longitudinal bone growth, cartilaginous model of bone first made by chondrocytes
Membranous ossification: flat bone growth (skull, facial bones, axial skeleton); woven bone formed directly without cartilage. |
|
|
Achondroplasia:
What is it? Mutation? Risk of inheritance? |
Failure of longitudinal bone growth (endochondral)
Due to mutation in FGFR3 AUTOSOMAL DOMINANT: 50% risk of inheritance if one normal parent, one dwarfed parent |
|
|
Osteoporosis:
Risk factors Presentation Prophylaxis |
Note: normal bone mineralization and lab values!!
Risks: older age smoking steroids white thin No weight-bearing exercise Poor ca2+, vit D hypogonadism (menopause included) heparin Presents with vertebral crush fractures (acute back pain, kyphosis, loss of height) Femoral neck fracture Prophylaxis: exercise, calcium ingestion before age 30 Tx: SERMs, calcitonin, bisphosphonates! |
|
|
Bisphosphonates:
Suffix MOA AE |
-dronates
MOA: inhibit osteoclasts AE: corrosive esophagitis; must remain upright for a few hours after ingesting drug |
|
|
Osteopetrosis:
Pathophys Lab values |
Failure of normal bone resorption-->thik, dense bones prone to fracture
Due to abnl fn of osteoclasts Labs: Normal ALP, normal Ca2+, normal phosphate Dec'd marrow space-->anemia, low PLT, infection (PANCYTOPENIA), inc'd extramedullary hematopoiesis |
|
|
Osteomalacia/Rickets:
Pathophys Lab values |
Vitamin D deficiency, low calcium levels, inc'd PTH, low serum phosphate
|
|
|
Paget's Disease of Bone:
Pathophys Lab values Treatment |
Abnl bone architecture caused by inc in both oblast and oclast activity
Hat size can be inc'd, hearing loss common due to auditory foramen narrowing Labs: inc'd ALP with anl bone architecture Tx: bisphosphonates |
|
|
Vitamin D intoxication:
Effects What disease can mimic this? |
Inc'd absorption of Ca2+ and PO4
Dec'd PTH ALP normal Granulomatous dz ~sarcoidosis can cause elevated vitamin D |
|
|
Effect of renal insufficiency on:
Calcium Phosphate PTH |
Dec'd serum Ca2+ (can't activate Vit D as well)
Elevated PTH Elevated Phosphate (can't excrete) |
|
|
Polyostotic fibrous dysplasia:
Pathophys Presentation |
Bone replaced by fibroblasts, collagen, irregular boney trabeculae
A form of this is McCune-Albright Syndrome--precocious puberty, unilateral pigmented lesions (cafe-au-lait spots) |
|
|
Which bony disease:
Reversible when Vitamin D replaced |
Osteomalacia/Rickets
|
|
|
Which bony disease:
Excess osteoclastic activity results in disorganized bony architecture |
Paget's
|
|
|
Which bony disease:
Bone replaced by fibroblasts, collagen, irregular bony trabeculae |
Polyostotic fibrous dysplasia
|
|
|
Which bony disease:
Soft bones due to defective mineralization of osteoid |
Osteomalacia/Rickets
|
|
|
Which bony disease:
Failure of bone resorption-->thickened and dense bones |
Osteopetrosis
|
|
|
Which bony disease:
Genetic deficiency of carbonic anhydrase II |
Osteopetrosis
|
|
|
What are the following lab values like in Paget's disease?
Serum Ca Serum Phos Alk Phos PTH |
Elevated Alk Phos
|
|
|
What are the following lab values like in osteomalacia/Rickets?
Serum Ca Serum Phos Alk Phos PTH |
Low vit D-->Low serum Ca
Elevate PTH (phosphorus trashing hormone!) Low serum phos |
|
|
What are the following lab values like in osteitis fibrosa cystica?
Serum Ca Serum Phos Alk Phos PTH |
PTH high
High serum Ca Inc'd Alk Phos Low serum phos |
|
|
What are the following lab values like in osteoporosis?
Serum Ca Serum Phos Alk Phos PTH |
ALL NORMAL :)
|
|
|
What are the following lab values like in osteopetrosis?
Serum Ca Serum Phos Alk Phos PTH |
ALL NORMAL :)
|
|
|
Osteosarcoma:
Incidence Risk factors Presentation on x-ray |
Peak incidence in men 10-20 years of age
Risk factors: Paget's dz, bone infarcts, XRT, familial retinoblastoma (Rb gene) Poor prognosis Codman's triangle or sunburst pattern (form elevation of periosteum) on x-ray |
|
|
Ewing's sarcoma:
Presentation Hallmark feature |
Anaplastic small blue cell tumor (malignant) in boys <15
Extremely aggressive with early mets, but responsive to chemo Hallmark = onion-skin appearance in bone (going out for eWINGS and ONION rings) Pseudorosettes |
|
|
Which bone tumor:
Most common malignant primary bone tumor of children |
Osteosarcoma
|
|
|
Which bone tumor:
Most common malignant primary bone tumor in adults |
Multiple myeloma
|
|
|
Which bone tumor:
Most common benign bone tumor |
Osteochondroma
|
|
|
Which bone tumor:
11;22 translocation |
Ewing Sarcoma
|
|
|
Which bone tumor:
Soap-bubble appearance on x-ray |
Giant Cell Tumor
|
|
|
Which bone tumor:
Onion-skin appearance of bone |
Ewing Sarcoma
|
|
|
Which bone tumor:
May actually be a hamartoma |
Osteochondroma
|
|
|
Which bone tumor:
Codman's triangle on x-ray |
Osteosarcoma
|
|
|
Which bone tumor:
Associated with Gardner's syndrome |
Osteoma; note Gardner's syndrome = familial adenomatous polyposis!!!!!!
|
|
|
Osteoarthritis:
Pathophys Risk Factors Presentation Treatment |
Pathophys: Wear and tear dz; wear away cartilage
Risk factors: age, obesity, joint deformity Presentation: pain in weight-bearing joints after use (at end of day for example) NON INFLAMMATORY Tx: acetaminophen, NSAIDS, COX-2 inhibitors, injected steroids into joint |
|
|
Rheumatoid Arthritis:
Pathophys Diagnosis Presentation Treatment |
SYSTEMIC autoimmune dz--affects MCP, PIP (not DIP)
This is a TYPE III HYPERSENS RXN; 80% of pts have RF (+) Presentation: Morning stiffness > 30 minutes and improving with use, symmetric joint involvement, systemic syx (fever, fatigue, pleuritis, pericarditis) Treatment: NSAIDs, TNF-alpha inhibitors (Etanercept, infliximab, adalimumab) |
|
|
Sjogren's Syndrome:
Presentation Diagnosis |
Can't see, can't spit, can't climb up shit:
Dry eyes, dry mouth, arthritis Dx: SS-A (Ro), SS-B (La) antibodies; parotid enlargement (inc'd risk B cell lymphoma) |
|

|
Swan neck deformity-->RA
|
|
|
Gout:
Presentation Diagnosis Treatment |
Asymmetric joint distribution. Joint is swollen, red, painful.
Classic at MTP joint of BIG TOE (podagra). Tophus formation often of external ear, olecranon bursa, or Achilles tendon. Acute attack after large meal or alcohol consumption ELEVATED URIC ACID LEVELS ≠ GOUT DIAGNOSIS Dx: Negatively birefrignent uric acid crystals! Tx: Acute: Indomethacin (NSAID), colchicine Chronic: Allopurinol, probenecid (uricosuric) |
|
|
Colchicine:
MOA |
Bind and stabilizes tubulin to inhibit polymerization, impairing leukocyte chemotaxis and degranulatoin (it's an NSAID)
|
|
|
Probenecid:
MOA |
Inhibits reabsorption of uric acid in PCT
|
|
|
Allopurinol:
MOA |
Inhibits xanthine oxidase; dec'd conversion of xanthine to uric acid
|
|
|
NSAIDs:
MOA |
-Inhibit both COX-1 and COX-2
-Block PG synth |
|
|
This drug can close PDAs.
|
Indomethacin--an NSAID
|
|
|
Celecoxib:
Drug Class |
Irreversible COX-2 inhibitor
|
|
|
What is the treatment of acute out exacerbation?
|
Colchicine
NSAIDs--DRUG OF CHOICE Steroids |
|
|
What is the treatment of chronic gout?
|
Probenecid
Allopurinol Colchicine NSAIDs |
|
|
Pseudogout:
How does it differ from gout? Diagnosis? |
Calcium pyrophosphate crystals (Rhomboid)
Weakly positive birefringent Dx: Chondrocalcinosis; cartilage has calcium deposits (in knee for ex bc pseudogout affects large joints) Gold standard = joint aspirate |
|
|
Young, sexually active person with a swollen knee.
Cause? |
Infectious arthritis--Neisseria gonorrhoeae
|
|
|
Man presents with pain and swelling of knees, subcutaneous nodules around joints and Achilles tendon, and exquisite pain in the metatarsophalangeal joint of his right big toe.
Biopsy reveals needle-like crystals. Diagnosis? |
Gout
|

