![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
112 Cards in this Set
- Front
- Back
|
Foregut vs Midgut vs Hindgut:
Anatomic regions Blood supply |
Foregut: Pharynx-->Duodenum; celiac artery
Midgut: Duodenum to transverse colon; SMA Hindgut: Transverse colon to rectum; Inferior mesenteric Artery |
|
|
Gostroschisis:
What is it? Liver extrusion? Other anomalies (common/uncommon) |
Extrusion of abdominal contents through abdominal folds; not covered by peritoneum
Other anomalies uncommon Liver never protrudes |
|
|
Omphalocele:
What is it? Liver extrusion? Other anomalies (common/uncommon) |
Persistence of herniation of abdominal contents into umbilical cord; covered by peritoneum
Liver commonly protrudes Other anomalies COMMON--GI, GU, CV, CNS, MS |
|

|
Omphalocele
|
|
|
Describe the development of the midgut beginning at 6 weeks.
What can go wrong in this process? |
Midgut herniates through umbilical ring.
10th week: returns to abdominal cavity and rotates around SMA -if doesn't return to abdomen-->omphalocele -malrotation of midgut-->intestinal obstruction, volvulus |
|
|
Tracheoesophageal fistula:
What is it? Most common form? |
Abnl connection b/t esophagus and trachea
Blind esophageal pouch (atresia) Stomach (lower esophagus technically) attached to trachea |
|
|
Polyhydramnios is a sign of ______.
|
Inability to swallow (anancephaly--lack brain center to execute swallowing; tracheoesophageal fistula where esophagus = blind pouch)
|
|
|
Congenital pyloric stenosis:
What is it? |
Hypertrophy of pylorus causing obstruction
Results in nobilious projectile vomiting at ~2 weeks of age Tx = surgery |
|
|
Palpable olive mass in epigastric region of new born
Projectile vomiting (non-bilious) |
Congenital pyloric stenosis
Can also result in hypochloremic metabolic alkalosis |
|
|
Spleen is derived from ____.
|
Mesentery
|
|
|
Pancreas is derived from ____.
|
Mesoderm
|
|
|
Annular pancreas:
What is it? How does it arise? Presentation |
Ventral pancreatic bud abnormally encircles duodenum, forms ring of pancreatic tissue that may cause duodenal narrowing
2/3 of pts asyx throughout life Symptom onset includes children w/bilious vomiting, feeding intolerance, abdominal distention Adults present with abdominal pain, postprandial fullness/nausea, peptic ulceration, pancreatitis |
|
|
Ureteric bud:
Origin Role |
Derived from mesonephros
Gives rise to ureter, renal pelvises, and, through BRANCHING, calyces and collecting ducts Fully canalized by 10th week |
|
|
Pronephros vs Mesonephros vs Metanephros:
General roles |
Pronephros: around 'til week 4, then degenerates
Mesonephros: interim kidney for 1st trimester; contribtues to male genital system Metanephros: permanent kidney |
|
|
Potter's syndrome:
Pathophys Presentation |
Caused by malformation of ureteric bud
B/L renal agenesis-->oligohydramnios-->limb deformitis, facies, pulm hypoplasia |
|

|
Horseshoe kidney--normal function; inferior poles of both kidneys fuse during development, trapped under inferior mesenteric artery and remain low in abdomen
|
|
|
Horseshoe kidney:
Pathophys |
Inferior poles of both kidneys fuse and as they ascend, get trapped under INFERIOR MESENTERIC ARTERY
Kidney fn is nl |
|
|
SRY gene:
Role |
On Y chromosome
Contribute to testes development; Gene for Müllerian inhibiting factor from Sertoli cells to suppress paramesonephric ducts |
|
|
Role of Leydig cells in male genitourinary development.
|
Leydig cells secrete androgens to promote dev't of mesonephric ducts (everything except prostate)--SVs, Epididymis, Ejaculatory Duct, Ductus Deferens (SEED)
|
|
|
Why is female GU development considered the default?
|
Will occur unless receive inhibition by Müllerian inhibitory factor from Sertoli cells
Mesonephric duct will degenerate (no androgens) and paramesonephric duct will develop |
|
|
Bicornuate uterus:
What is it? Pathophys |
Incomplete fusion of paramesonephric ducts
|
|
|
Genital tubercle:
What does it become (in males and females)? Based on which hormones? |
If estrogen (female): glans clitoris, vestibular bulbs
If DHT (male): glans penis, corpus cavernosum, spongiosum |
|
|
Urogenital Sinus:
What does it become (in males and females)? Based on which hormones? |
Estrogen (female):
Vestibular glands Urethral, paraurethral glands DHT (male): bulbourethral glands prostate |
|
|
Urogenital Folds:
What does it become (in males and females)? Based on which hormones? |
Female (E2):
Labia minora Men (DHT): Ventral shaft of penis (penile urethra) |
|
|
Labioscrotal swelling:
What does it become (in males and females)? Based on which hormones? |
E2-->labia majora
DHT-->scrotum |
|
|
Epispadias vs Hypospadias
|
Epispadias--urethra opens on dorsal side of penis
Hypospadias--urethra opens on ventral side of penis |
|
|
Exstrophy of the bladder is associated with _______.
|
Epispadias (dorsal urethra)
|
|

|
Exstrophy of bladder--assocd w/epispadias in males
|
|
|
Who has Barr bodies?
|
Women and men with Klinefelter's (have an extra X chromosome)
|
|
|
47XXY
|
Klinefelter's
|
|
|
45XO
|
Turner syndrome
|
|
|
Turner Syndrome:
Chromosomal abnormality Presentation Hormone levels |
45XO
Short stature Streak overies with infertility WEBBED NECK Shield chest Most common cause of primary amenorrhea! Low E2-->high LH and FSH |
|
|
This chromosomal disorder causes women to lack a Barr body.
|
Turner's
Don't have Barr body because only have 1 X chromosome--no need to inactivate |
|
|
Very tall
Severe Acne Normal fertility Anti-social behavior |
Double Y Syndrome--XYY
|
|

|
Klinefelter's:
gynecomastia no secondary sex chars hypogonadism |
|

|
Turner's Syndrome:
webbed neck shield chest |
|
|
Diagnose:
High testosterone High LH |
Defective androgen receptor (at level of CNS--no negative feedback)
|
|
|
Diagnose:
High testosterone Low LH |
Testosterone-secreting tumor
Exogenous steroids |
|
|
Diagnose:
Low testosterone High LH |
Primary hypogonadism
|
|
|
Diagnose:
Low testosterone Low LH |
Hypogonadotropic hypogonadism
|
|
|
True hermaphrodite vs Pseudohermaphrodite:
General Karyotype |
True hermaphrodite: both ovary and testicular tissue present (ovotestis); ambiguous genitalia. RARE
(46 XX or 47XXY) Pseudohermaphrodite: External genitalia ≠ gonadal sex (testes vs ovaries) Female: XX; ovaries present but external genitalia are virilized/ambiguous (inappropriate exposure to androgens during early gestation) Male: XY; testes present but external genitalia are female or ambiguous. Most common form is androgen insensitivity syndrome (testicular feminization) |
|
|
Androgen insensitivity:
Pathophys Presentation Hormone levels? |
Defect in androgen receptor-->normal-appearing female externally, but with rudimentary vagina
Develops testes---often found in labia majora; surgically removed to prevent malignancy High T, E, and LH (AR's aren't being activated, so keep pumping out T) |
|
|
Ambiguous genitalia until puberty
|
5-alpha reductase deficiency--inability to convert testosterone to DHT
Puberty provides inc'd T to cause masculinization and growth of external genitalia |
|
|
What is cryptorchidism?
Risks? |
Failure of testis to descend into scrotum
Usually unilateral 35x inc'd risk of malignant tumor in undescended testicle (usually germ cell tumor) |
|
|
23 year-old patient presents with one testicle.
What is the patient at risk of? |
Undescended testicle-->germ cell tumor
|
|
|
24 year-old male develops testicular cancer.
Metastatic spread occurs by what route? |
Para-aortic LNs-->body
|
|
|
16 year-old female presents with amenorrhea. She lacks a uterus and uterine tubes and there are 2 round structures in the midline superior to the labia majora.
Cause of amenorrhea? |
Androgen insensitivity syndrome
|
|
|
Female homologue:
Scrotum |
Labia majora
|
|
|
Female homologue:
Prostate gland |
Urethra and paraurethral glands
|
|
|
Female homologue:
Glans penis |
Glans clitoris
|
|
|
Female homologue:
Corpus spongiosum |
Vestibular bulb
|
|
|
Female homologue:
Bulbourethral glands |
Vestibular glands
|
|
|
Female homologue:
Ventral shaft of penis |
Labia minora
|
|
|
Gene that codes for testes determining factor
|
SRY on Y chrom
|
|
|
Female short stature
No Barr body |
Turner's
|
|
|
XXY
|
Kleinfelter's
|
|
|
XO
|
Turner's
|
|
|
Presence of ovaries with external male genitalia
|
Female pseudohermaphrodite
|
|
|
Unable to generate DHT
|
5-alpha-reductase deficiency
|
|
|
Both ovarian and testicular tissues present
|
True hermaphrodite
|
|
|
Webbing of neck
|
Turner's
|
|
|
Male with Barr body in PMNs
|
Kleinfelter's
|
|
|
Ambiguous genitalia until puberty, then masculinization
|
5-alpha-reductase deficiency
|
|
|
Congenital cause:
Most common cause of early cyanosis |
Tetralogy of Fallot
|
|
|
Congenital cause:
Most common cause of late cyanosis |
VSD-->Eisenmeyer's syndrome
|
|
|
Congenital cause:
Most common cause of primary amenorrhea |
Turner's
|
|
|
Congenital cause:
Most common chromosomal disorder |
Down's
|
|
|
Congenital cause:
Most common cause of Mental Retardation Second most common? |
FAS followed by Down's and Fragile X
|
|
|
Congenital cause:
Most common cause of lethal genetic disease in Caucasians |
CF
|
|
|
Congenital cause:
Most common cause of congenital malformations in US |
FAS
|
|
|
Germ layer:
Retina |
Neuroectoderm
|
|
|
Germ layer:
Salivary glands |
Surface ectoderm
|
|
|
Germ layer:
Pancreas |
Endoderm
|
|
|
Germ layer:
Muscles of abdominal wall |
Mesoderm
|
|
|
Germ layer:
Thymus |
Endoderm
|
|
|
Germ layer:
Spleen |
Mesentary
|
|
|
Germ layer:
Aorticopulmonary septum |
NCC (ectoderm technically?)
|
|
|
Germ layer:
Anterior pituitary |
Surface ectoderm
|
|
|
Germ layer:
Posterior pituitary |
Neuroectoderm
|
|
|
Germ layer:
Bones of skull |
NCC
|
|
|
Germ layer:
Cranial nerves |
NCC
|
|
|
What is the most common type of TE fistula?
|
Blind esophagus, lower esophageal segment attached to trachea
|
|
|
What is Potter's syndrome?
|
Bilateral renal agenesis due to malformation of ureteric bud
|
|
|
Classic presentation of congenital pyloric stenosis?
|
Olive mass
Poor feeding Projectile vomiting (non-bilious) Hypochloremia metabolic alkalosis |
|

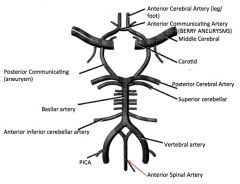
Label
|
|
|
|
Anti-centromere antibodies
|
Scleroderma (CREST)
|
|
|
Anti-desmoglein antibodies
|
Pemphigus vulgaris (blistering)
|
|
|
Anti-glomerular BM antibodies
|
Goodpasture's Syndrome (GN and hemoptysis)
|
|
|
Anti-histone antibodies
|
Drug-Induced lupus (hydralazine, INH, phenytoin, procainamide)
Not HIPP to have Lupus! |
|
|
Anti-IgG antibodies
|
Rheumatoid artrhitis
|
|
|
Anti-mitochondrial antibodies
|
Primary biliary cirrhosis (female, cholestasis, portal HTN)
|
|
|
Anti-neutrophil cytoplasmic antibodies
|
Vasculitis--
C-ANCA: Wegener's P-ANCA: Churg-Strauss Microscopic polyangitis |
|
|
Anti-platelet antibodies
|
Idiopathic thrombocytopenic purpura (ITP)
|
|
|
Anti-topoisomerase antibodies
|
Diffuse scleroderma
|
|
|
Anti-transglutaminase/anti-gliadin
|
Celiac
|
|

|
Bamboo spine featuring calcifications between vertebrae
Ankylosing Spondylitis |
|
|
Azurophilic granular needles in leukemic blasts
|
Auer rods--AML; esp. promyelocytic type
|
|
|
Bamboo spine on x-ray
|
Ankylosing spondylitis (HLA-B27)
|
|
|
Basophilic nuclear remnants in RBCs
|
Howell-Jolly Bodies
|
|
|
Basophilic stippling of RBCs
|
Lead poisoning
Sideroblastic anemia |
|
|
Bloody tap on LP
|
SAH
|
|
|
Boot-shaped heart on x-ray
|
Tetralogy of Fallot
RVH |
|
|
Branching gram-positive rods with sulfur granules
|
Actinomyces israeli
|
|
|
Bronchogenic apical lung tumor
|
Pancoast's Tumor
|
|
|
Brown tumor of bone
|
Hemorrhage causes brown color of osteolytic cysts; due to Hyperparathy
|
|
|
Cardiomegaly with apical atrophy
|
Chagas' Disease
|
|
|
Cardiomegaly
Megacolon Megaesophagus |
Chagas'
|
|
|
Cellular crescents in Bowman's capsule
|
Rapidly progressive crescentic glomerulonephritis
|
|
|
Chocolate cyst of ovary
|
Endometreiosis
|
|
|
Circular grouping of dark tumor cells surrounding pale neurofibrils
|
Homer Wright rosettes--neuroblastoma (it's an adrenal tumor!!), medulloblastoma, Ewing sarcoma
|
|
|
Colonies of mucoid Pseudomonas in lung
|
Cystic Fibrosis (CFTR mutation in Caucasians-->fat-soluble vitamin deficiency and mucus plugs)
|
|
|
Anti-nuclear antibodies
|
ANAs: anti-Smith and anti-dsDNA-->SLE (type III hypersens)
|

