![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
139 Cards in this Set
- Front
- Back
|
LN follicles:
Cortex vs Paracortex (cell contents, function) |
Cortex: B cells located here, proliferate here
Paracortex: T Cells; between follicle and medulla; where blood enters |
|
|
In extreme cell immune response, this region of the LN becomes enlarged.
|
Paracortex--responsible for LAD
|
|
|
Patients with DiGeorge have a poorly developed _____ of the lymph node.
|
Paracortex not weel dev'd (low T cell count)
|
|
|
LN:
Cords vs Sinus (cell contents) In what region are both of these located? |
Medulla:
Sinus: macs Cords: Plasma cells |
|
|
Sinusoids of spleen:
B vs T Cell locations |
PALS--periarterial lymphatic sheet contains T cells
B cells in follicles, white pulp |
|
|
What cell type is responsible for removing encapsulated bacteria from blood?
Where is this cell located? |
Macs in spleen remove encapsulated bacteria
|
|
|
Vaccine requirements for the asplenic.
Why? |
Need immunization against encapsulated bacteria--strep pneumo, h flu, n meningitidis, salmonella, klebsiella) need pneumovax, h flu vaccine, meningococcus
Bc no longer have macs to get rid of encaps bacteria |
|
|
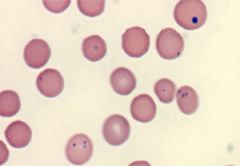
Howell-Jolly Bodies: Asplenic
|
|

|
Splenic infarct (wedge shape/triangle = classic sign of ischemia)
|
|
|
Axillary node
|
Upper limb, lateral breast
|
|
|
Celiac node
|
Stomach
|
|
|
Superior mesenteric node
|
Duodenum, jejunum
|
|
|
Colic node
|
Sigmoid colon
|
|
|
Inferior mesenteric node
|
Sigmoid colon
|
|
|
Internal iliac node
|
Rectum (above pectinate line)
|
|
|
Superficial inguinal node
|
Anal canal
Scrotum Superficial thigh |
|
|
Superficial and deep plexuses (nodes)
|
Testes
|
|
|
Para-aortic node
|
Scrotum
|
|
|
Popliteal node
|
Lateral side; dorsum of foot
|
|
|
Right lymphatic duct
|
Right arm, right half of head
|
|
|
Thoracic duct
|
Everything right lymphatic duct doesn't drain (remember Right lymphatic drains Right arm, right half of head)
|
|
|
The thoracic duct drains at the_______.
|
Junction of left subclavian in internal jugular vein
|
|
|
Thymus:
Cortex vs Medulla (cells and processes) |
Cortex has immature T Cells
Corticomedullary junction: where selection occurs Medulla-->mature T cells; AKA selection |
|
|
Embryologic origin of thymus.
|
Thymus comes from epithelium of third branchial pouch
|
|
|
Innate immune system:
Cells involved |
Nphils, macs, DCs (APCs for macs), NKCs, complement
|
|
|
Adaptive immune system:
Cells involved |
T cells, B cells, circulating Abs
|
|
|
NKCs:
Enzymes used When are they activated? |
Perforins and granzymes to induce apoptosis of virally infected cells
(Only lymphocyte member of innate immunity!) Activated when receive nonspecific activation signal on target cell and/or absence of MHC I on target cell surface |
|
|
These cytokines enhance NKC activity.
|
IL-12, IFN-beta, IFN-alpha
IFN very important for inducing NKCs and cells neighboring infected cells to generate substances that will inhibit viral protein synthesis |
|
|
This cytokine stimulates T cells.
|
IL-2
|
|
|
This cytokine stimulates macrophages.
|
IFN-gamma
|
|
|
This cytokine inhibits T cells and macrophages.
|
IL-10
|
|
|
This cytokine stimulates B cells.
|
IL-4, IL-5
|
|
|
Beginning with BM, describe maturation of T cells.
Include CD markers. |
BM-->Thymus Cortex (CD4+8+)-->Positive and Negative Selection at corticomedullary jn in thymus(negatively selected cells undergo apoptosis)-->CD4+ or CD8+
|
|
|
CD8+ cells:
Role Enzymes used |
Kills virus-infected cells directly
Neoplastic cells Donor graft cells ~NKCs Use perforins (helps deliver granzymes) and granzymes (activates apoptosis) CD8 binds MHC1 |
|
|
These cells recognize the absence of MHC1.
|
NKCs
|
|
|
These cells are activated by binding MHC1.
|
CD8+
|
|
|
What type of cytokine induces a T helper cell to become Th1?
|
IL-12
|
|
|
This cytokine is elevated in times of viral infection.
|
IL-12
|
|
|
These cytokines are released by Th1 cells.
|
IL-2-->stimulates T cells
IFN-gamma-->stimulates macs IL-10-->inhibits Th1 |
|
|
This cytokine induces formation of Th2 cells.
|
IL-4 (humoral response--B cell response)
|
|
|
These cytokines are released by Th2 cells.
|
IL-4, 5-->stimulate B cells
IL-10-->inhibit Th cells; inhibits macs |
|
|
What is class switching and what cells undergo this?
|
IgM-->IgG = class switching (for B Cells)
|
|
|
Describe steps necessary to activate CD4+ cell.
|
MHCII on APC recognizes TCR (T cell receptor) and presents antigen to CD4+
B7 on APC co-stimulates CD28 on T cell T helper cells will then produce cytokines |
|
|
Describe steps necessary to activate CD8+ cell.
|
CD8 activation
Virally infected cells present antigen on MHC1 molecule, TCR recognizes it; CD8 helps Th1 cells release IL-2 and this binds IL-2 receptor on CD8+ cell (co-stimulation) |
|
|
Describe steps necessary to activate B cell.
|
B cell activation
Th2 release IL-4,5,6 CD40L on Th cell binds CD40 on B cell and allow for co-stimulation |
|
|
Th1 vs Th2 cells:
General roles Cytokines secreted by them Cytokines inhibiting them |
Th1:
regulates cell-mediated response Secretes IL-2, IFN-gamma Activates macs and CD8+ cells Inhibited by IL-10 from Th2 Th2: Regulates humoral response Secretes IL-4, IL-5, IL-10 Helps B cells make Ab (IgE>IgG) Inhibited by IFN-gamma from Th1 cell |
|
|
Functions of IL-1,2,3,4,5.
|
Hot T Bone StEAk
HOT: IL-1 (fever) T: IL-2 (stimulates T cells) Bone: IL-3 (stimulates BM) StEak: IL-4 (IgE production) SteAk: IL-5 (IgA production) |
|
|
B cell:
Immunoglobulins CD Markers |
IgM
IgD CD-19,20,21 |
|
|
Epstein-Barr Virus infects this cell.
|
CD21+
You drink Beer at the Barr when you're 21. |
|
|
MHC II is present on these cells.
|
Macrophages
B cells (can act as presenting cells) |
|
|
Macropahges:
CD markers Receptors |
CD14, 40, 16
Receptors for Fc and C3b (these are opsonins) |
|
|
NKCs:
CD markers Receptors |
CD16--binds Fc of IgG
Receptor for MHCI |
|
|
CD16 is present on this cell.
|
Macrophages and NKCs
|
|
|
What CD markers protect host cells from complement mediated damage?
|
WBC, RBC, platelets
Protected by CD55 and CD59 |
|
|
What are the acute phase cytokines?
What cell releases these? |
Macrophages release IL-1, IL-6, TNF-alpha
These substances mediate fever and ramp up immune system. |
|
|
What are the 2 pathways to stimulate macrophages to make acute phase cytokines?
|
1) strep pyogenes, staph aureus release super ag's: crosslink TCR to MHCII on APCs, causes uncoord'd release of IFN-gamma from Th1 and subsequent release if IL-1,6, and TNF-alpha from macs
2) Endotoxins (LPS of gram neg bact); bind CD14 (endotoxin receptor). doesn't require T helper cells. |
|
|
CD14:
Role |
Binds endotoxins (LPS) and activates macs
|
|
|
This cytokine actives eosinophils.
|
IL-5
|
|
|
IL-1:
Role Secreted by |
Endogenous pyrogen
Causes fever, acute inflammn Activates endothelium to express adhesion molecules Secreted by macs |
|
|
IL-6:
Role Secreted by |
Endogenous pyrogen
Secreted by Th1 cells and macs |
|
|
IL-8:
Role |
Major chemotactic factor for nphils
"Clean up on aisle 8"-->neutrophils recruited by IL-8 to clear infection |
|
|
These cytokines recruit neutrophils.
|
IL-8
LT-B4 C5a |
|
|
IL-12:
Role |
Activates NK and Th1 cells
|
|
|
This cytokine mediates septic shock.
|
TNF-alpha
|
|
|
TNF-alpha:
Role |
Activates endothelium
Causes leukocyte recruitment, vascular leakage |
|
|
Anti-TNF-alpha drugs:
Examples Uses Considerations |
Etanercept
Infliximab Adalimumab These are all MAbs! Uses: RA, ankylosing spondylitis Must check for latent Tb prior to dosing, because will make prone to infection! |
|
|
Cytokine released by all T cells
Role? |
IL-3: Supports growth and diff of BM SC's
~GM-CSF |
|
|
Cytokines released by Th1 cells.
Role? |
IL-2:
Stimulates growth of helper and cytotoxic T cells IFN gamma: activates macs and Th1 cells; antiviral and antitumor properties |
|
|
Cytokines released by Th2 cells.
Role? |
IL-4: induces diff into Th2 cells. Promotes growth of B cells. Class switching to IgE, IgG
IL-5: Promotes differentiation of B cells. Enhances switching to IgA. Stimulates growth and diff of ephils. IL-10: Modulates inflamm response. Inhibits activated T cells and Th1. Activates Th2. |
|
|
This cytokine is released by regulatory T cells.
|
IL-10
|
|
|
Interferon:
Mechanism |
alpha and beta: inhibit viral protein synthesis
gamma: inc'd MHCI and II expression and Ag presentation in all cells Activates NK cells to kill virus-infected cells |
|
|
IFN-alpha:
Clinical use |
HBV
HCV Kaposi's Leukemia Malignant melanoma |
|
|
IFN-beta:
Clinical use |
MS
|
|
|
IFN-gamma:
Clinical use |
Chronic granulomatous disease
|
|
|
Aldesleukin:
Clinical use |
AKA IL-2
Renal cell carcinoma Metastatic melanoma |
|
|
EPO:
Clinical use |
Anemias; esp in renal failure or pts undergoing chemotx
|
|
|
Filgrastim:
Clinical use |
(gra stim-->granulocyte stimuln) AKA granulocyte CSF
BM recovery (after chemo) |
|
|
Sagramostim:
Clinical use |
Granulocyte macrophage colony stim factor
BM recovery (after chemo) |
|
|
This cytokine is similar to GM-CSF in its effects.
|
IL-3 (Bone of Hot T Bone mnemonic)
|
|
|
Oprelvekin:
Clinical use |
IL-11; use in thrombocytopenia
|
|
|
Thrombopoietin:
Clinical use |
Thrombocytopenia
|
|
|
HLA genes that encode MHC II.
|
HLA DR
HLA DQ HLA DP Doctor walks into DQ to get a Dr Pepper |
|
|
CD marker displayed only by helper T cells.
|
CD4
|
|
|
CD marker displayed only by cytotoxic T cells.
|
CD8
|
|
|
CD marker displayed on all T cells.
|
CD3
|
|
|
CD marker displayed by B cells.
|
CD19,20,21
|
|
|
CD marker displayed by all NKCs.
|
CD16 (binds IgG)
|
|
|
CD marker that inhibits C9 binding.
|
CD55, 59
|
|
|
CD marker that acts as endotoxin receptor.
|
CD14 (on macs)
|
|
|
This cytokine promotes B cell growth and differentiation.
|
IL-4,5
|
|
|
This cytokine is produced by Th1 cells.
|
IL2, IFNgamma
|
|
|
This cytokine is produced by Th2 cells.
|
IL-10
|
|
|
This cytokine is involved in growth and activation of eosinophils.
|
IL-5
|
|
|
This cytokine inhibits macrophage activation.
|
IL-10
|
|
|
Pyrogens secreted by monocytes and macrophages.
|
IL1,6; TNF alpha
|
|
|
This cytokine inhibits Th1 cell production.
|
IL-10
|
|
|
This cytokine inhibits Th2 cell production.
|
IFN-gamma
|
|
|
This cytokine mediates inflammation.
|
IL-1,6, TNF alpha
|
|
|
This cytokine enhances synthesis of IgE and IgG.
|
IL-4
|
|
|
This cytokine enhances synthesis of IgA.
|
IL-5
|
|
|
This cytokine is released by virally infected cells.
|
IFN-alpha, beta
|
|
|
This cytokine supports growth and differentiation of BM SCs.
|
IL-3
|
|
|
This cytokine supports T cell proliferation, differentiation, and activation.
|
IL-2
|
|
|
Bond that holds antibodies together.
|
Disulfide bonds holds Ab together; connect heavy chain to light chain, light chain to light chain, etc.
|
|
|
Fab region of antibody:
Function Comprising regions |
Antigen-binding
Determines idiotype--unique Ag binding pocket; only 1 antigenic specificity expressed per B cell (B Cells produce Abs!) Composed of 2 light chain and 2 heavy chain regions |
|
|
Fc region of antibody:
Function Comprising regions |
Constant
Carboxy terminal Complement binding Carbohydrate side chains Determines isotype (IgM, IgD, etc) 2 heavy chains! |
|
|
List 5 types of heavy chains and corresponding immunoglobulins.
|
Mu--IgM
Delta--IgD Gamma--IgG Alpha--IgA Epsilon--IgE |
|
|
List types of light chains
Ratio? |
Lambda
Kappa No functional difference between these 2! Should have 2 kappa per 1 lambda If have multiple myeloma, this ratio will be thrown off based on type of Ab creating. |
|
|
IgG structure:
Heavy and light chains |
2 gamma heavy chains
2 either lambda or 2 kappa regions (light chains) |
|
|
Terminal deoxynucleotidyl transferase:
Role |
Adds nucleotides to DNA during VJ (light chain) or VDJ (heavy chain) rearrangement
|
|
|
What initiates VDJ recombination?
|
Recombination activating gene complex RAG 1 and RAG2 recognize RSSs and initiate VDJ recombination
Results break in dsDNA at Recombination Signal Sequences (RSS) that flank V, D, and J regions |
|
|
Mutations in RAG genes
|
Inability to initiate VDJ rearrangement and results in arrest of B and T cells development
B and T cells can't express unique Ag receptors (Antibodies) |
|
|
Half-life of IgG
|
21 days--passive immunization requires monthly inoculation
|
|
|
Main antibody in secondary response to antigen.
|
IgA (delayed response = secondary response)
|
|
|
Main antibody in primary response to antigen.
|
IgM (immediate response = primary response)
|
|
|
Immunoglobulin associated with allergies because it's bound by mast cells and basophils.
|
IgE
|
|
|
Immunoglobulin that comprises 75% of total immunoglobulin pool.
|
IgG
|
|
|
Immunoglobulin present in large quantities on membrane of B cells.
|
IgD, IgM
|
|
|
Immunoglobulin that crosses the placenta and confers immunity to neonates.
|
IgG
|
|
|
Immunoglobulin that can occur as dimer.
|
IgA
|
|
|
Immunoglobulin largely confined to intravascular pool.
|
IgM (early Ab)
|
|
|
Immunoglobulin distributed evenly between intravascular and extravascular pools.
|
IgG
|
|
|
Immunoglobulin in mucoserous secretions such as saliva, colostrum, milk, genitourinary secretions.
|
IgA
|
|
|
Immunoglobulin that can occur as pentamer.
|
IgM
|
|
|
Thymus independent Ag's vs Thymus dependent antigens:
General Examples |
Thymus independent: no peptide component; MHC can't bind anything, ex: LPS on gram neg bact
Results in release of IgM, don't form memory Thymus dep Ag's: ex: vaccines, will create memory Allows for class-switching: IgM-->IgG Release of IL-4,5,6 |
|
|
What stimulates alternative pathway of complement?
|
Microbial (LPS)
|
|
|
Classic PW:
What stimulates it? Complement factor involved? |
Ag-Ab complexes
C1 = first copmlement involved C1 esterase inhibits cleavage of C1 (prevents cascade) |
|
|
Complement factors associated with anaphylaxis.
Why? |
C3a, C5a: Anaphylaxis
C3a-->**mast cells, basophils-->histamine -->edema, vasc perm-->BP drops bc fluid is trapped in swelling Tx w/epi |
|
|
Complement factor associated with neutrophil chemotaxis.
|
C5a: nphil chemotaxis
|
|
|
Complement factors associated with membrane attack complex.
|
C5b-9: makes membrane attack complex
|
|
|
C1 esterase:
Role Effect of deficiency |
C1 esterase inhibits cleavage of C1 and prevents classic PW activation
Deficiency leads to hereditary angioedema (results in elevations of bradykinin) |
|
|
Deficiency of this complement factor results in recurrent pyogenic sinus and respiratory tract infections.
|
C3
Recurrent infections withstrep pneumo, h flu Inc'd susceptibility to type III hypersens rxns (esp GN) |
|
|
Deficiency of this complement factor results in neisseria bacteremia.
|
Deficiency of C5-C8--
(gonococcal and meningococcal bacteremia) These are involved in MAC (membrane attack complex) |
|
|
Deficiency of this results in lysis of RBCs and paroxysmal nocturnal hemoglobinuria.
|
Deficiency of Decay Accelerating factor (CD55)
|
|
|
Paroxysmal nocturnal hemoglobinuria:
Presentation Dx Tx |
Hemosiderinuria-->iron deficiency anemia
Chronic intravascular hemolysis Thrombosis Dx with Ham's test--RBCs lyse at low pH Tx: Iron Warfarin (too many platelets) BM transplant (bc due to |
|
|
Which vaccines result in rapid immunity after exposure to the bug?
|
To Be Healed Rapidly:
Give pre-formed Ab's and vaccine for: Tetanus Botulinum HBV Rabies Also RSV (respiratory syncytial virus for premature babies in winter months) |
|
|
What is anergy?
|
Self-reactive T cells become nonreactive without co-stimulatory molecule (tolerance to self)
|
|
|
List granulomatous diseases
|
Tb (only one that is caseating)
Fungal infections (histo, blasto) Syphilis (gummas) Leprosy Cat scratch fever Sarcoid Crohn's Berylliosis Listeria Foreign bodies Wegner's granulomatosus Chronic granulomatous disease |
|
|
This bacteria results in cat scratch fever.
|
Bartonella henselae
|

