![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
122 Cards in this Set
- Front
- Back
|
Most common causes of meningitis:
Newborn-->6m |
Group B Strep
E coli Listeria |
|
|
Most common causes of meningitis:
Children 6m-6y |
Strep pneumo
Neisseria meningitides H influenza Enteroviruses |
|
|
Most common causes of meningitis:
6y-->60y |
Strep pneumo
N. meningitidies Enteroviruses HSV (temporal lobe encephalitis) |
|
|
Most common causes of meningitis:
60+y |
Strep pneumo
Gram neg rods Listeria |
|
|
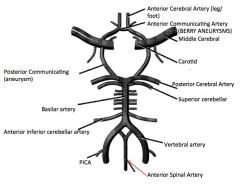
What portion of the brain is supplied by the anterior cerebral artery?
|
Medial surface--Premotor/sensory of legs and feet
|
|
|
What portion of the brain is supplied by the middle cerebral artery?
|
Lateral surface--Broca's, Wernicke's, motor/sensory of face and arms
|
|
|
What group of genes is responsible for skeletal development?
|
Hox genes
|
|
|
What is the classic clinical presentation of a thyroglossal duct cyst?
|
Asyx mass, midline neck
Moves with swallowing Younger than 30 Can become infected and cause abscess; must be resected |
|
|
Which hepatic phase of metabolism is lost first by geriatric patients?
|
Phase I
|
|
|
Which hepatic phase of metabolism is mediated by cytochrome p450?
|
Phase I
|
|
|
What are the 4 obligate aerobic bacteria?
|
Nocardia
Pseudomonas aeruginosa M. tuberculosis Bacillus spp (Nagging Pests Must Breathe) |
|
|
Which vasculitis:
Necrotizing granulomas of lung and necrotizing glomerulonephritis |
Wegener's granulomatosis
|
|
|
Which vasculitis:
Necrotizing immune complex inflammation of visceral/renal vessels |
Polyarteritis nodosa
|
|
|
Which vasculitis:
Young Asian women |
Takayasu's arteritis
|
|
|
Which vasculitis:
Young asthmatics |
Churg-Strauss Syndrome
|
|
|
Which vasculitis:
Infants and young children; involved coronary arteries |
Kawasaki's Dz
|
|
|
Which vasculitis:
Most common vasculitis |
Temporal arteritis (Giant cell)
|
|
|
Which vasculitis:
a/w hepatitis B infection |
Polyarteritis nodosa
|
|
|
What can prevent the neurotoxicity of isoniazid?
|
Pyridoxine (vit B6)
|
|
|
What is the treatment for TCA cardiotoxicity?
|
NaCO2 to alkalinize plasma/urine
|
|
|
What is the treatment for theophylline cardiotoxicity?
|
beta-blockers
|
|
|
What is the difference between malingering and facticious disorder?
|
Malingering--conscious creation of symptoms to conscious motivation; ex: gain disability, get free food from hospital cafeteria
Facticious--creation of symptoms but motivation is unconscious, i.e., to assume sick role |
|
|
What artery is damaged:
Aneurysm causes the eye to look down and out |
Posterior Communicating Artery-->CN III palsy
|
|
|
What artery is damaged:
Aneurysm may cause bilateral loss of lateral visual fields |
Anterior Communicating Artery
|
|
|
What artery is damaged:
Broca's or Wernicke's aphasia |
MCA
|
|
|
What artery is damaged:
Unilateral lower extremity sensory and/or motor loss |
Anterior Cerebral Artery
|
|
|
What artery is damaged:
Unilateral facial and arm sensory and/or motor loss |
Middle Cerebral Artery
|
|

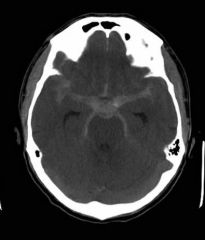
Label.
|
|
|

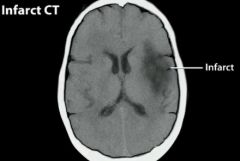
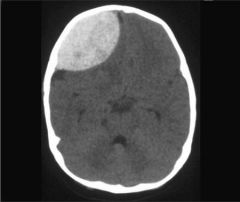
Artery affected.
|
PCA
|
|
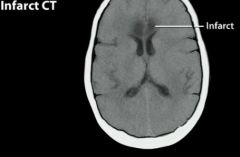
Artery affected.
|
MCA
|
|
|
Medial Medullary Syndrome:
Pathophys AKA Presentation |
Occlusion of anterior spinal artery (from vertebral artery)-->unilateral infarct of medial portion of rostral medulla
AKA anterior spinal artery syndrome Syx: -Contralateral spastic hemiparesis -Contralateral tactile and kinesthetic defects -Tongue deviates toward side of lesion (hypoglassal nuc/nerve damage) PAIN AND TEMP PRESERVED |
|
|
What is the hallmark sign of a general brainstem lesion?q
|
Alternating syndromes where there are long tract symptoms on one side (hemiparalysis) and cranial nerve symptoms on other side.
|
|
|
Wallenberg Syndrome:
Pathophys AKA Presentation |
AKA Lateral Medullary Syndrome
Caused by occlusion of one of the posterior inferior cerebellar arteries (PICA)-->unilateral infarct of lateral portion of rostral medulla Syx: Loss of pain/temp over contralateral body Loss of pain/temp over ispislateral face Hoarsness, diff swallowing, lose gag reflex Ipsilateral Horner's syndrome Vertigo, nystagmus, n/v Ipsilaterial cerebellar deficits (ataxia, past pointing) |
|
|
Lateral Inferior Pontine Syndrome:
Pathophys Presentation |
Occlusin of anterior inferior cerebellar arteries (AICA)
Syx: Ipsilateral facial nerve paralysis Ipsilateral loss of taste from anterior 2/3 tongue Ipsilateral deafness, tinittus Nystagmus, vertigo, n/v Ipsilateral limb/gait ataxia Ipsilateral loss pain/temp from face Contralat loss pain/temp sensation No paralysis! |
|
|
Posterior Cerebral Artery:
Lesion effects |
Contralateral hemianopia (blindness) w/macular sparing; supplies occipital cortex
|
|
|
Weber's Syndrome:
Pathophys Presentation |
Midbrain infarct from occlusion of Posterior Cerebral Artery
Syx: Cerebral peduncle lzn-->contralateral spastic paralysis (hemiparesis) Oculomotor nerve (CN III) palsy-->ipsilateral ptosis, pupillary dilation, lateral strabismus (eye looks down and out) |
|
|
Middle Cerebral Artery:
Lesion Effects |
Contralateral face/arm paralysis, sensory loss
Aphasia (dominant sphere) Left-sided neglect |
|
|
Anterior Cerebral Artery:
Lesion Effects |
Loss of motor/sensory of brain, leg-foot areas
|
|
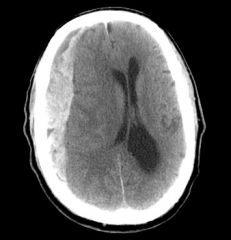
Artery effected.
|
ACA
|
|
|
Anterior Communicating Artery:
Lesion Effects |
Visual field defects--blurry, or bitemporal hemianopia (loss of lateral visual fields)
|
|
|
Posterior Communicating Artery:
Lesion Effects |
CN III palsy; eye looks down and out (strabismus)
|
|
|
Watershed Zones:
When are they lesioned? Effects |
Damaged in severe hypotension-->upper leg/upper arm weakness, defects in higher-order visual processing
|
|
|
Basilar Artery:
Lesion Effects |
Locked-in syndrome (CN III typically intact)
|
|
|
Stoke of Anterior Circle of Willis:
Effects |
General sensory/motor dysfn, aphasia
|
|
|
Stroke of Posterior Circle of Willis:
Effects |
CN deficits (vertigo, visual deficits), coma, cerebellar deficits (Ataxia), dominant hemisphere (ataxia), nondominant (neglect)
|
|
|
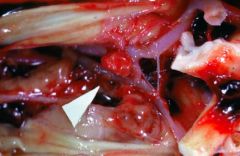
How can a lumbar puncture distinguish between an acute an several day old subarachnoid hemorrhage?
|
Acute--bloody
Several day old--xanthochromia (bilirubin present bc RBCs broken down) |
|
|
Berry aneurysm
|
|

|
Berry aneurysm
|
|
|
SAH
|
|
|
Epidural hematoma
|
|
|
Subdural hematoma
|
|

|
Parenchymal hemorrhage
|
|
|
Epidural hematoma:
Pathophys Presentation CT findings |
Rupture of middle meningeal artery (branch of maxillary artery); often 2º to fracture of temporal bone
Presents with lucid interval prior to CN III palsy (eye looks down and out) due to rapid expansion under systemic arterial pressure CT shows biconvex disk not crossing suture lines Can cross falx, tentorium. |
|
|
Subdural hematoma:
Pathophys Presentation CT findings |
Rupture of bridging veins
Slow venous bleedings, late onset of syx Seen in elderly, alcoholics (tend to fall); shaken babies Crescent-shaped hemorrhage that crosses suture liens. Cannot cross falx, tentorium. |
|
|
Subarachnoid hemorrhage:
Pathophys Presentation CT findings |
Rupture of aneurysm (usually berry aneurysm in Marfan's, Ehlers-Danlos, APCKD).
Patient complains of "worst HA of my life" Bloody or yellow (xanthochromic) spinal tap Asterisk-shaped lesion on CT |
|
|
Parenchymal hematoma:
Pathophys |
Caused by hypertension, amyloid angiopathy--lobar strokes all over brain, DM, tumor
|
|
|
Brain's healing response to atherosclerotic thrombus.
|
Leads to ischemic stroke-->subsequent necrosis.
Brain then forms cystic cavity with reactive gliosis (line with astroglia?) |
|
|
Assessment of stroke:
CT vs MRI |
CT won't show ischemia until after 24 hours
MRI will identify ischemia within 3-30 mins of stroke |
|
|
Describe the path of CSF. Begin with its site of production.
|
CSF made by choroid plexus
Absorbed by venous sinus arachnoid granulations -->Lateral ventricle-->3rd ventricle via FORAMEN OF MONROE -->Third ventricle-->4th ventricle via CEREBRAL AQUEDUCT -->4th ventricle-->Subarachnoid space via: -Foramina of Lushka (Lateral) -Foramen of Megendie (Medial) |
|
|
How does CSF enter venous circulation?
|
CSF-->Venous Sinus arachnoid granulations-->Superior saggital sinus
|
|
|
Hydrocephalus:
Communicating vs Obstructive-- Pathophys |
Communicating--dec'd CSF absorption by arachnoid villi-->inc'd ICP, papilledema, herniation
Obstructive (noncommunicating)--structural blockage of CSF circulation within ventricular system (stenosis of aqueduct of Sylvius for ex) |
|
|
Normal pressure hydrocephalus:
Pathophys Presentation |
Wet, wobbly, wacky
Doesn't result in inc'd subarachnoid space volume. Expansion of ventricles distorts fibers of corona radiata and leads to dementia, ataxia, and urinary incontinence (reversible cause of dementia in elderly) |
|
|
Hyrocephalus ex vacuo:
Pathophys |
Appearance of inc'd CSF in atrophy.
ICP normal Triad not seen |
|
|
Which spinal nerves innervate the diaphragm?
|
C3, C4, C5
|
|
|
Which spinal nerves are responsible for erectile response?
|
S2, S3, S4
|
|
|
Which spinal tract:
Touch, vibration, and pressure sensation |
Doral columns--fasciculus gracilis, cuneatues
|
|
|
Which spinal tract:
Voluntary motor command from motor cortex to body |
Lateral/ventral corticospinal tracts
|
|
|
Which spinal tract:
Voluntary motor command from motor cortex to head/neck |
Corticobulbar tract
|
|
|
Which spinal tract:
Alternate routes for the mediation of voluntary movement |
Reticulospinal and rubrospinal tracts
|
|
|
Which spinal tract:
Pain and temperature sensation |
Lateral spinothalamic tract
|
|
|
Which spinal tract:
Important for postural adjustments and head movements |
Vestibulospinal tract
|
|
|
Which spinal tract:
Proprioceptive information for the cerebellum |
Dorsal/ventral spinocerebellar tracts
|
|
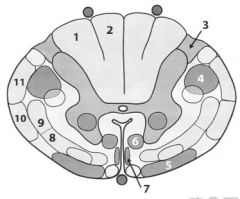
Label
|
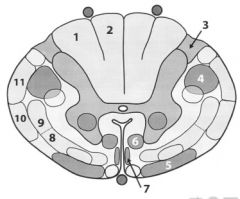
1. Fasciculus cuneatus (info from arms)
2. Fasciculus gracilis (info from legs) 3. Lisshauer's tract (pain/temp) 4. Lateral corticospino tract (movement info) 5. Vestibulospinal tract (reflexive info; postural adj) 6. Reticulospinal tract 7. Anterior/ventral corticospinal tract (motor from brain) 8. Anterior/ventral spinothalamic tract 9. Lateral spinothalamic tract (pain and temp) 10. Anterior spinocerebellar tract (info to cerebellum) 11. Posterior/drosal spinocerebellar tract (proprioception info to cerebellum) |
|
|
Dorsal column:
Tract Function Synapses |
Medial lemniscal PW
Ascending pressure, vibration, touch, proprioception, sensation Sensory nerve ending->DRG Cell body-->Ascend in dorsal column ->Ipsilateral nucleus cuneatus or gracilis (medulla)-->Decussates in medulla-->ascends contralaterally in medial lemniscus -->VPL of thalamus-->sensory cortex |
|
|
Spinothalamic column:
Tract Function Synapses |
Ascending pain and temperature sensation
Sensory nerve (A-delta, C fibers)-->Cell body in DRG-->ipsilateral gray matter Decusates at anterior white commissure-->VPL of thalamus-->Sensory cortex |
|
|
Lateral corticospinal tract:
Tract Function Synapses |
Descending voluntary movement of contralateral limbs
Upper MNs--cell body in primary motor cortex-->decends ispilaterally until decussating at caudal medulla-->descends contralaterally -->cell body of anterior horn -->Leaves spinal cord -->NMJ |
|
|
Upper vs Lower Motor Neuron Lesions:
General |
LMN: Hyporeflexia, atrophy (mm not receiving motor info)
UMN: hyperreflexive, Babinski reflex positive (spinal innervation intact, but no motor info from brain), spastic paralysis MUSCLE WEAKNESS IN BOTH |
|
|
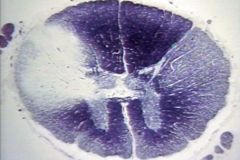
Random, asymmetric white matter lesions-->MS
|
|

|

Brainw/periventricular white matter plaques of demyelination, gross.
Demyelination occurs in bilateral asymmetric distribution. MULTIPLE SCLEROSIS |
|
|
Poliomyelitis:
Method of spread Presentation Lab values |
Poliovirus (fecal-oral)
Malaise, HA, , fever, nausea, abdominal pain, sore threat LMN lesions--muscle weakness, atrophy, fasciculations, hyporeflexia Findings: CSF w/lymphocytic pleocytosis with slight elevation of protein (no change in CSF glucose) Virus recovered from stool or throat |
|
|
Multiple Sclerosis:
Pathophys Presentation Diagnosis |
Autoimmune inflammn and demyelination of CNS (brain and SC)
Presentation: optic neuritis (sudden loss of vision), MLF syndrome (internuclear ophthalmoplegia), hemiparesis, hemisensory syx, bowel/bladder incontinence Relapsing and remitting course Mostly affects women in 20s and 30s; more common in whites (Classic triad of MS is SIN: Scanning speech, INtention tremor, INcontinence, INternuclear ophthalmoplegia, and Nystagmus) Tx: beta-IFN or immunosuppressant tx Labs: elevated IgG in CSF; oligoclonal bands (of IgG) diagnostic (MRI is gold standard) |
|
|
Internuclear ophtalmoplegia:
Pathophys Presentation |
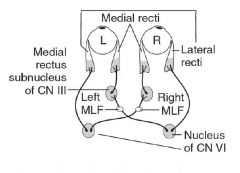
Lesion in medial longitudinal fasiculus (MLF)-->medial rectus palsy on attempted lateral gaze
Nystagmus in abducting eye Convergence is normal Seen in MS! (When looking left, left nucleus of CN VI fires, which contracts left lateral rectus and stimulates right nucleus of CNIII via right MLF to contract right medial rectus) |
|
|
Amyotrophic lateral sclerosis:
Pathophys Presentation |
Combined upper and lower MN deficits with no sensory deficit. Both upper and lower MN signs.
No oculomotor deficits. Can be caused by defect in superoxide dismutase 1 (SOD1). Commonly presents as fasciculations and eventual atrophy; progressive and fatal. |
|
|
Complete occlusion of anterior spinal artery:
Effects |
Spares dorsal columns and Lissauer's tract
Lose everything except touch, vibration, proprioception, pressure info |
|
|
Tabes Dorsalis:
Effects |
Tertiary syphilis
Degeneration of dorsal roots and dorsal columns; impaired proprioception, locomotor ataxia Lose joint sensation (Charcot's joint) |
|
|
Syringomyelia:
Effects |
Damages anterior white commissure (cervical lesion)
Results in b/l loss of pain/temp sensation of hands/arms |
|
|
Vitamin B 12 Neuropathy:
Effects What other conditions exhibit this? |
Demyelination of dorsal columns, lateral corticospinal tracts, spinocerebellar tracts
Results in: -ataxic gait Hyperreflexia Impaired posn and vibration sense Also exhibited by: Vitamin E deficiency Friedrich's Ataxia |
|
|
Friedreich's Ataxia:
Pathophys Presentation |
GAA repeat disorder (encodes frataxin)
Friedreich is Frat-tastic (frataxin): Favorite frat brother, always stumbling, staggering, and falling Leads to impairment in mitochondrial fn-->staggering gait, falling, nystagmus, dyarthria, hypertrophic CM (cause of death) |
|
|
Brown-Sequard Syndrome:
Pathophys Effects |
Hemisection of spinal cord.
Presentation: -ipsilateral UMN (corticospinal tract) below lesion -ipsilateral loss of tactile, vibration, proprioception (dorsal column) below lesion -Contralateral pain and temp loss (spinothalamic tract) below lesion -ipsilateral loss of sensation at level of lesion -LMN signs (flaccid paralysis) at level of lesion |
|

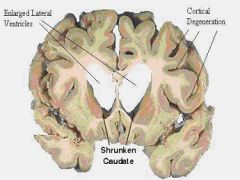
Identify caudate.
|
|
|
|
What are the findings of Brown-Sequard Syndrome?
|
UMN signs ipsilaterally below lzn
Dorsal column loss of info ipsilaterally below lzn Contralateral loss of pain and temp 2-3 segments below lzn LMN signs, flaccid paralysis All sensation lost ipsilaterally at level of lzn |
|
|
What is the most common site of a berry aneurysm?
What diseases are often a/w berry aneurysms? |
Anterior Communicating Artery
a/w: Ehlers-Danlos syndrome Marfan's syndrome ADPKD |
|
|
Site of decussation:
Dorsal columns |
Medulla after nuc
|
|
|
Site of decussation:
Lateral corticospinal tract |
Medullary pyramids
|
|
|
Site of decussation:
Spinothalamic tract |
Anterior white commissure ~3 segments above region of innervation
|
|
|
What is the classic presentation of syringomyelia?
What malformation is a/w syringomyelia? |
b/l loss of pain and temp sensation typically in upper extremities
weakness, atrophy of hand mm |
|
|
What are the cardinal features of Parkinson's disease?
|
TRAP
tremor rigidity (cogwheel) akinesia postural instability |
|
|
What are the classic signs of an upper motor neuron lesion? Of a lower motor neuron lesion?
|
UMN:
spastic paralysis hyperreflexia LMN: flaccid paralysis atrophy fasciculations |
|
|
A man in his 40s begins to develop early dementia and uncontrollable movements of his upper extremities.
Where in the brain do you expect to see atrophy? |
Caudate (HD)
|
|
|
A male patient presents with involuntary flailing of one arm.
Where is the lesion? |
Hemiballismus-->Contralateral subthalamic nucleus
|
|
|
Most common cause:
Myocarditis |
Coxsackie or Echovirus
|
|
|
A 28 year-old chemist presents with MPTP exposure.
What neurotransmitter is depleted? |
Dopamine
|
|
|
A patient cannot abduct her left eye on lateral gaze and convergence is normal.
She is also having difficulty smiling. Where is the lesion? |
Abducens and Facial nerve affected
must be a pontine lesion |
|
|
A lesion of what artery causes locked-in syndrome?
|
Basilar artery
|
|
|
When performing a lumbar puncture for anesthesia, where is the anesthesia dosed?
Where is CSF found? |
Anesthesia dosed to Epidural space, CSF in subarachnoid space
|
|
|
A 28-year old women is involved in an MVA. She initially feels fine, but minutes later she loses consciousness.
CT scan reveals intracranial hemorrhage that does not cross suture lines. Which bone and vessel were injured? |
Classic for epidural hematoma
RUpture of Middle Meningeal Artery caused by injury to temporal bone |
|
|
A 40 year-old man with a history of Marfan's syndrome and hypertension presents with severe headache. A head CT is normal at presentation and examination of the CSF reveals numerous RBCs.
What is the cause of the man's headache? |
Subarachnoid hemorrhage due to ruptured berry aneurysm
|
|
|
An 85 year-old man with Alzheimer's disease falls at home and presents 3 days later with severe headache and vomiting.
What is the mostly likely diagnosis? What structures were damaged? |
Subdural hematoma due to rupture of bridging veins
|
|
|
Most common cause:
Hypoparathyroidism |
Thyroidectomy
|
|
|
Most common cause:
Metastatic disease to brain |
Lots of bad stuff kills glia
Lung Breast Melanome RCC GI tumors |
|
|
Most common cause:
Lysosomal storage disease |
Gaucher's Dz
|
|
|
Horner's Syndrome:
Pathophys Presentation |
A/w lesion of spinal cord above T1, e.g., Pancoast's tumor, Brown-Sequard syndrome (hemisection), late stage syringomyelia
PAM is horny (Horner's) Ptosis Anhidrosis (absence of sweating) and flushing of affected side of face Miosis (pupils constrict) Due to pancoast tumor |
|
|
C2 dermatome
|
Skull cap
|
|
|
C3 dermatome
|
high turtleneck shirt
|
|
|
C4 dermatome
|
low collar shirt
|
|
|
T4 dermatome
|
Nips
|
|
|
T7 dermatome
|
Xiphoid process
|
|
|
T10 dermatome
|
umbilicus (belly butTEN)
|
|
|
L1 dermatome
|
Inguinal ligament (LI is IL)
|
|
|
L4 dermatome
|
Kneecaps, anterior thigh
|
|
|
Spinal nerves for penile and anal sensation.
|
S2, S3, S4
|
|
|
What spinal nerves account for clinical reflexes?
|
Reflexes count up in order:
Achilles: S1, S2 Patella: L3, L4 Triceps: C5, C6 Biceps: C7, C8 |

