![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
Carbon Dioxide |
Produced during cell metabolism
CO2 diffuses 20x more easily than O2, so it readily crosses cell membranes and physical barriers |
|
|
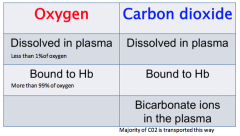
Methods of O2 and CO2 transport |
|
|
|
3 'forms' of CO2 in plasma |
1. Dissolved in plasma - amount of CO2 dissolved in plasma is proportional to PaCO2 and its solubility coefficient. - CO2 is 22x more soluble in water than O2 - the more pressure pushing the gas into the plasma, the more it will dissolve
2. Combined with plasma proteins - combine to form "carbamino compounds"(albumin, glycoproteins) - a relatively small number of amino groups on proteins are able to do this - accounts for a small fraction of transport
3. Combined with water in plasma to form H2CO3 - this happens very slowly because there is no loose carbonic anhydrase enzyme in plasma
Adding up all 3 of these mechanisms makes up less than 10% of the CO2. The rest is all carried by hemoglobin |
|
|
CO2 transport in red blood cells |
- CO2 readily diffuses from plasma into RBC's because they are so thin and squish between capillaries - RBC's have many more terminal protein groups that can react with CO2 to form carbamino compounds (ie. has more buffering capacity) - carbonic anhydrase enzyme inside RBCs |
|
|
Carbonic Anhydrase Enzyme |
Inside RBCs, the hydration reaction with water is enhanced by the carbonic anhydrase enzyme. This enzyme is only present in RBCs, which is why they are so much more effective at transporting CO2 than plasma. Once formed, H2CO3 quickly dissociates into H+ and HC03- ions inside the red blood cell.
CA CO2 + H20 <--> H2CO3 <---> HCO3 + H |
|
|
Bicarbonate Ions |
As more and more HCO3 is formed from the hydration of CO2, it diffuses out of the RBCs along it diffusion gradient into the plasma. - Cl diffuses into the RBCs to maintain electrical neutrality (the "chloride shift") - water also diffuses into cells so RBCs in venous blood are slightly larger than those found in arterial blood Most CO2 that is produced is transported as HCO3
|
|
|
When the CO2 reaches the lungs |
When venous blood reaches the capillaries in the lungs, CO2 that was dissolved in solution (plasma) diffuses out of the blood along its gradient into the alveoli.
Breathing/ventilation of alveoli keeps CO2 levels low, maintaining the gradient for diffusion of CO2 |
|
|
Haldane Effect |
Reactions in RBCs now in reverse. CO2 comes off the proteins and dehydration of H2CO3 forms CO2 and water. A conformational change occurs in Hb so that O2 can now bind. The exposure to O2 drives this change and enhances the release of CO2 into the alveoli for elimination from the body |
|
|
Normals levels of CO2 |
- Respiratory system is designed to maintain arterial CO2 levels around 40 mmHg (35-45mmHg) - If CO2 is increased, it becomes a stressor on the body (stimulates a sympathetic response) that increases heart rate, blood pressure, bronchodilation, and ventilation. - What's important is how much blood is delivered to the lungs, not so much the gas exchange. |
|
|
Ways to measure CO2 levels |
1. CO2 in the blood (artery, vein) with a blood gas analyzer
2. Expired air (end-tidal) with a capnograph. Black region = inspiration, no CO2 present. Blue = expired CO2. Monitors hypoventilation. High number means they aren't ventilating |
|
|
Control of Ventilation |
|
|
|
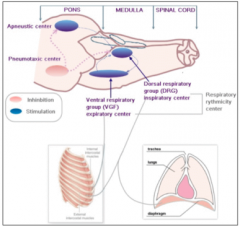
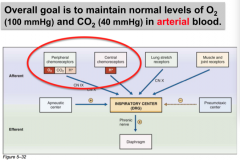
3 Components of the Respiratory Control System |
1. Sensors (peripheral and central) gather information about CO2, O2, pH, movement, etc. 2. Central controller in the brain coordinates information and determine what actions to take. 3. Effectors (muscles) induce a response and ventilate the animal. - Together they all form a feedback loop |
|
|
Overall goal of control system |
|
|
|
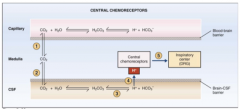
Central chemoreceptors |
- Located near the ventral surface of the medulla - Sensitive to changes in H+ levels (not O2 levels) in the interstitial fluid of the brain (but the BBB is not permeable to H+ ions) - CO2 is freely diffusible and indirectly exerts a stimulating effect on respiration through altering H+ levels in the brain. - Ventilation (increased tidal volume and respiratory rate) is stimulated by increases in PaCO2. Excitatory to the inspiratory centre (DRG) |
|
|
Central chemoreceptor diagram |
|
|
|
Peripheral chemoreceptors |
- Located in areas that are highly perfused with arterial (oxygenated) blood: aortic bodies along the aortic arch, and carotid bodies at the bifurcation of the carotid arteries. - Respond to changes in H+, PaCO2, and PaO2. They are responsive to the partial pressures of O2 and CO2, not the total amount or content (i.e. are active at high altitude, but not if the patient is anemic) - Ventilation is stimulated in response to low oxygen or high CO2 |
|
|
Peripheral chemoreceptors |
Excitatory to respiratory centre (stimulate ventilation) through the vagus nerve (aortic bodies) and the glossopharyngeal nerve (carotid bodies)
Account for ~30% of the normal ventilatory drive in response to changes in CO2. Central receptors account for the majority (70%) |
|
|
Peripheral responses to PaO2 |
When arterial O2 levels decrease, the receptors become very active and stimulate ventilation as a last ditch attempt to bring O2 into the body. This sometimes happens during euthanasia. |
|
|
The "Respiratory Centre" |

- Dorsal Respiratory Group (DRG) in the medulla - Ventral Respiratory Group (VRG) in the medulla - Pneumotaxic Centre in the rostral pons - Apneustic Centre in the caudal pons
|
|
|
Central Controller |
- Collections of neurons that are located in the brainstem (medulla and pons) - Generates the rhythmic, periodic pattern of regular breathing - Allows for unconscious adjustments to breathing pattern with exercise, disease, swallowing, etc. - Cortex also plays a role (e.g. conscious changes) |
|
|
Dorsal Respiratory Group (DRG) |
Generates the basic rhythm of breathing Receives input from the glossopharyngeal and vagal nerves. - mechanoreceptors in the pleura respond to stretch - peripheral chemoreceptors respond to O2 and CO2 levels Output is relayed via the phrenic nerve to the diaphragm. Stimulates contraction to initiate inspiration |
|
|
Ventral Respiratory Group (VRG) |
Expiration is normally a passive process due to elastic recoil of the lungs and chest wall
VRG not usually active with normal respiration
Primarily responsible for expiration when there needs to be an active component (e.g. exercise). Seen in a horse with heaves |
|
|
Pneumotaxic Centre |
Inhibits inspiration by regulating inspiratory volume and rate
Involved in "fine-tuning" of respiratory rhythm since normal rhythm can still exist in absence of this centre. Located in the dorsal part of the pons |
|
|
Apneustic Centre |
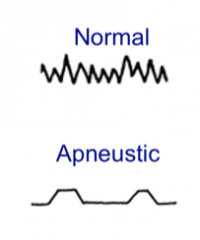
Least understood of the 4 areas, no consensus as to its role in respiration. Believed to be involved in deep breathing/apneustic breathing. Can be seen in certain situations: - ketamine-based anesthesia - brain injury or tumours (high ICP) |
|
|
Muscles of Respiration |
Diaphragm Intercostal muscles abdominal muscles accessory muscles
The central controller ensures that they all function in a coordinated manner |

