![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
How do you calculate cardiac output?
|
CO = SV * HR
|
|
|
How does HR affect preload?
|
/\ HR -> \/ preload because less time to fill (after /\ 160 bmp will lower SV)
|
|
|
What does the cardiac function curve demonstrate?
|
t
|
|
|
What does the cardiac function curve demonstrate?
|
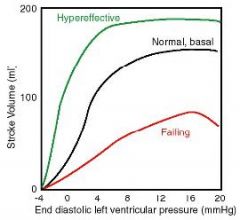
contractile performance. a shift up in cardiac function curve indicates a hypereffective, increased contractility functioning heart. notice that the x axis is the EDP which is a measurement of preload and the y axis (SV) is a measure of performance and thus contractility.
|
|
|
What are some intrinsic factors that increase contractility?
|
1. norepi and epi w beta-adrenergic receptors (sympathetic nerves)
2. beta agonists 3. digitalis that inhibit Na pump (raising IC Na) -> raising IC Ca 4. thyroid hormone |
|
|
What are some extrinsic factors that decrease contractility?
|
1. ACh (parasympathetics)
2. Ca channel blocking drugs 3. MI, infection, toxins, hypoxia, hypthermia or anything else that induces failure |
|
|
What are the best ways to measure preload?
|
1. ED fiber length
2. EDV 3. EDP 4. R atrial pressure 5. Central venous pressure |
|
|
What change (ESV or EDV) indicates a del preload?
|
del EDV exclusively is an ideal situation where del preload has occurred. a real world example would be a del EDV > del ESV
|
|
|
What change (ESV or EDV) indicates a del contractility?
|
del ESV exclusively is an ideal situation where del contractility has occurred.
|
|
|
What does exclusively del preload do to EF?
|
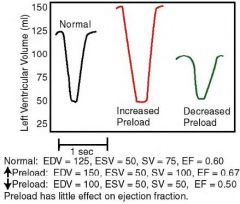
very little. del preload does not really change EF much.
|
|
|
What does del contractility do to EF?
|
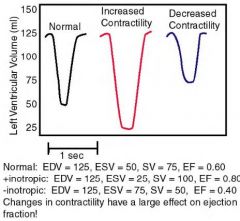
huge effect. EF =SV/EDV and this ratio increases with increased contractility as well as decreases with decreased contractility
|
|
|
How does increased preload manifest in the PV loop as SV, ESV, EDV and shape and size?
|
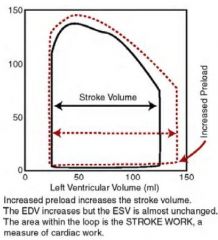
increased preload
increased SV increased EDV no change ESV little change in peak force widens shape |
|
|
What happens to the venous and arterial pressure when the cardiac output is forced to change? This relates to a vascular function curve.
|
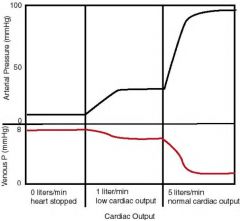
1. no CO => high Pv and low Pa
2. low CO => slightly reduced Pv, slightly increased Pa 3. normal CO => Pv = very little, Pa = 100% increase |
|
|
What is Pmcf?
|

Pmcf is the central venous pressure in terms of the mean circulatory filling pressure. It is the mean circulatory filling pressure. It can be visualized on the vascular function curve which is CO vs central venous pressure where CO = 0, central venous pressure = Pmcf.
|
|
|
What will cause a shift upward or downward without changing the slope in a vascular function curve?
|

increased (relative) volume like a transfusion
decreased (relative) volume like a hemorrhage relative because if del venomotor tone occurs, it looks like del blood volume. /\ venomotor tone => veins gets relatively smaller => relative /\ blood volume => /\ central venous pressure. snap. |
|
|
What happens to the vascular function curve when arterial tone changes?
|

The Pmcf does NOT change, but the slope does change. With arteriolar vasodilation, the slope decreases and the pressure rises. With arteriolar vasoconstriction slope increases and the pressure lowers.
|
|
|
Over what HR does the CO benefit decrease and the SV tolerance drop to levels that are no longer helpful in increasing CO?
|
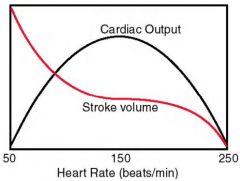
~ 150 bpm
|
|
|
What is the Bowditch effect?
|
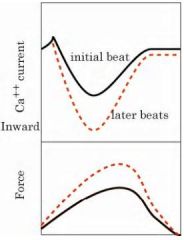
this is rate-induced regulation. up to a certain HR there is a summation-like effect occurring in cardiac cells for 2 reasons:
1. /\ APs => /\ Ca influx => Ca accumulation and /\ residual Ca 2. /\ Ca current during each AP but after a certain HR diastole shortens so much that preload is shortened, the AP decreases amplitude because it occurs during relative refractory period => SV reduction. |
|
|
What is postextrasystolic potentiation?
|
When an extra-systole occurs wherein an anomalous extra beat generated by a latent pacemaker occurs, the extrasystolic beat is less, but because of the extra Ca the postextrasystolic beat is greater than normal.
Beats after the postextrasystolic beat gradually, over the course of 2 or 3 beats, return to normal tension. |
|
|
What is a premature contraction?
|
the earlier a premature contraction occurs, the weaker it is because of a lower Ca current. this represents a lower preload.
|
|
|
What is the normal resting EF?
|
~ 0.6
|
|
|
What is the normal dP/dT?
|
~ 3000 mmHg/sec
|
|
|
A 35-year-old male presents with cyanosis and serious decrease of arterial blood pressure. The patient's L ventricular EF is 0.75 and dP/dTmax is 4800 mmHg/sec. HR is 120 bpm. What is the most likely cause of his hypotension?
a. \/ sympathetic activity b. /\ sympathetic activity c. failure of L ventricular contractility d. hemorrhage e. /\ parasympathetics |
d. hemorrhage
|
|
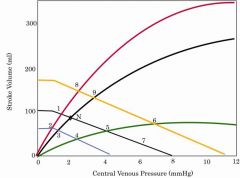
What point best represents 30 minutes after abrupt occlusion of the left circumflex?
|
moments after - point 4
30 min after - point 5 days after - point 6 green curve because contractility has decreased venous pressure has not changed in 30 minutes |
|
What point represents compensated response to loss of 20% of blood volume? No renal fluid retention or replacement has occurred.
|
first point 3 - loss of blood volume
then point 2 - after contractility compensation |
|
What point best represents the response 30 seconds after bolus intravenous injection of a large dose of beta1-adrenergic agonist?
|
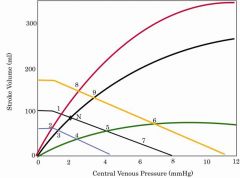
point 1 - before volume expansion
point 8 - after volume expansion (increased preload) |
|

What point would normal go to with a rapidly infused 1.5 L of plasma?
|
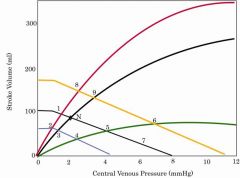
point 9 - volume expansion with no compensation
|
|
|
How does one estimate the CO by the Fick Principle?
|
Fick Principle is mass is neither created or destroyed and since concentration (C) = mass (M) / volume (V) => V=M/C then we can consider the following and crack this goose:
1. pulmonary blood flow = CO 2. deoxygenated venous blood goes to the lungs to get to arterial oxygen levels 3. oxygen consumed per minute (VO2) can be measured 4. arterial (CaO2) and venous (CvO2) oxygen concentrations can be measured OK... so if you take the amount of blood pumped per minute (CO) and multiply it by the concentration of oxygen consumed (CaO2-CvO2) then you should get the oxygen consumed per minute (VO2). Rearrange that shit: CO = VO2/(CaO2-CvO2) bam. CO. |

