![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
Insulin Resistance causes what?
|
Dyslipidemia
|
|
|
What are PPARs? What do they do? P263
|
Peroxisome Proliferator-Activated Receptors. They are TFs that heterodimerize with FA ligands. Once dimerized, they bind to nuclear receptor Retinoid X Receptor (RXR) to affect expression of genes involved in lipid metabolism, glucose metabolism, and inflammation.
|
|
|
PPAR-alpha is an isoform of PPAR - what does it do?
|
It targets fibrates and stimulates genes involved in B-oxidation as well as increasing ApoA1 expression - a component necessary for HDL - effectively lowering TG levels and increasing HDL.
|
|
|
PPAR gamma is an isoform of PPAR - what does it do?
|
It's a target of thiazolidinediones (TZD), functioning as an agonist that lowers glucose levels, enhances insulin sensitivity, and increases SR-B1 receptor (facilitates uptake of cholesteryl esters from HDL in the liver i.e. reverse cholesterol transport).
|
|
|
What are the three features carachterizing Familial Hypercholesterolemia? (p264)
|
1. Elevated concentration of LDL in plasma
2. Deposition of LDL-derived cholesterol in tendons and skin (xanthomas) and in arteries (atheromas) 3. Inheritance as an autosomal dominant trait with gene dosage effect (homo- more severe than hetero-) |
|
|
What is the defect in FH? (p264)
|
It's a defect in the LDL receptor.
|
|
|
What are atheromas in coronary arteries called?
|
Atherosclerosis.
|
|
|
What are the three feature characterizing atherosclerosis?
|
1. Accumulation of cholesteryl esters in cells derived from the monocyte-macrophage line ("foam cells")
2. Smooth muscle cell proliferation 3. Fibrosis |
|
|
If a cell detects that there is too much cholesterol, what three things can it do? (p265)
|
1. Down reg HMG-CoA Reductase
2. Up reg ACAT - esterifying excess cholesterol for packaging 3. Down reg LDL receptor |
|
|
Where is LDL receptor protein synthesized? How does it get to the surface of the cell?
|
ER and to surface by secretory pathway.
|
|
|
In addition to the pathway on p265, review p 266 for more detail on who the cell manages extracellular fluctuations in cholesterol.
|
In addition to the pathway on p265, review p 266 for more detail on who the cell manages extracellular fluctuations in cholesterol.
|
|
|
There are 20 or so genes that mediate the uptake and synthesis of cholesterol...including the LDL receptor. What are they called? (p267)
|
Sterol regulatory element-binding proteins (SREBPs).
|
|
|
Describe how the LDL receptor levels are regulated by SREBPs. (p267)
|
SREBPs (Sterol regulatory element-binding proteins) and SCAP (SREBP cleavage-activiting protein) are the major players:
1. SCAP and SREBP associate with each other in the ER membrane 2. SCAP detects low levels of sterol and along with SREBP, they leave the ER and migrate to the golgi. 3. SCAP cleaves SREBP at two locations, freeing the N-terminal domain. 4. SREBP migrates to DNA and turns on genes for LDL receptor and HMG-CoA synthesis. |
|
|
What are the 5 classes of mutations that decrease the activity of the LDL receptor? (p. 268)
|
1. No protein made/defective
2. No transport from ER to golgi 3. LDLR cannot bind lipoproteins 4. LDLR cannot enter Clatherin-Coated pit (necessary for internalization) 5. LDLR cannot be recycled |
|
|
How does LDLR limit LDL production? (p268)
|
By efficiently removing its precursor, IDL, from circulation.
|
|
|
For heterozygote pts with FH, what are three ways you can help them lower their LDL?
|
1. Bile acid resins
2. Statins 3. Diet |
|
|
How do bile acid resins lower LDL?
|
Resins prevent reabsorption of bile acids (i.e. cholesterols) in the ileum. The liver detects a decrease in cholesterol levels and responds by absorbing LDL for their cholesterol and to produce more bile acids.
|
|
|
On the opposite side, there's a diagram of how LDLR's respond to the presence of bile resins. Describe what happens and how this is a useful treatment for FH heterozygotes.
|
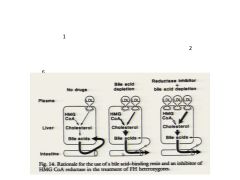
Bile acids are not re-absorbed, liver detects this, increases LDL receptor, effectively lowering the LDL concentration in circulation.
|
|
|
Describe how LDL apheresis works. (p269)
|
Blood is removed from the FH HOMOZYGOUS pt, apoB100 containing particles are removed (i.e. LDL), and blood is returned. Performed every 1-2 weeks.
|
|
|
What are the three (potential) treatment options for FH homozygote pts?
|
1. LDL plasma exchange
2. Liver transplant 3. Gene therapy |
|
|
Why is a liver transplant an option of FH homozygotes and what are the two major risks?
|
70% of the body's LDL receptors are in the liver.
Risky for pts with coronary disease. Lifelong need for immunosuppression carries substantial risk |

